The following are excerpts from the show notes of Episode 101 GI Bleed Emergencies Part 1 dealing with Transfusion In GI Bleed [link is to the podcast and show notes] from Emergency Medicine Cases:
Initial fluid management in massive GI bleed emergencies
Avoid excessive crystalloid resuscitation. While there is no literature to guide us specifically in this patient [in the case discussed at the beginning of the podcast].
population a general rule of thumb is that hemodynamically unstable bleeding patients need blood products. Practically speaking, there are often delays in obtaining blood products, so our experts recommend giving a minimum amount of fluid to maintain MAP > 60 mm Hg.
Transfusion management in GI bleed emergencies
General principles of transfusion management in GI bleed emergencies
Hemodynamic instability: Transfuse regardless of hemoglobin level
Shock index: A shock index (HR/SBP) of >1 should trigger consideration for massive transfusion
Don’t trust the Hb: Hemoglobin often lags behind bleeding, so trend it by repeating the hemoglobin in an hour or two.
Consider clinical factors: Presyncopal patient, high volume blood loss or brisk bleeding should trigger consideration for red cell transfusion.
Be flexible: Lower your threshold to transfuse in patients with co-morbidities such as coronary artery disease or coagulopathy.
Most GI bleed patients can tolerate low hemoglobins: Stable patients with a chronic GI bleed of small volume can generally tolerate low hemoglobins.
Portal bleeding: Restitution of blood volume may be associated with recurrence of portal bleeding.
While there is no specific literature for hemoglobin transfusion thresholds for LGIB a landmark study out of NEJM in 2013 in patients with stable UGIB suggested that a hemoglobin threshold of 7 for red cell transfusion [6].
Stable UGIB patients in the liberal transfusion arm (Hb<9) had increased bleeding, higher mortality, increased need for surgery and increased length of stay when compared to the restricted transfusion group (Hb<7). Note that this study was conducted in a highly controlled environment with rapid access to endoscopy and therefore, may not be applicable to resource limited settings.
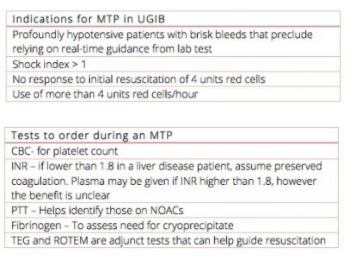
Indications for Massive Transfusion Protocol in GI bleed emergencies
GI bleed patients bleed differently compared to trauma patients. GI bleeds do not impart the same hyperfibrinolysis of that of a trauma bleed and so do not require as much coagulation support. A close look at the TRIGGER Study [7] out of the UK, reveals that only 5% of variceal bleeds require a massive transfusion protocol. In other words, 95% of GI bleed patients require only red cell transfusions. Over-activation of massive transfusion protocols lead to unnecessary complications such as Transfusion Associated Circulatory Overload (TACO) and wasted blood products. The following are Dr. Jeannie Callum’s recommendations for when to trigger a Massive Transfusion Protocol and what tests to order.
*The shock index (SI) is a bedside assessment defined as heart rate divided by systolic blood pressure, with a normal range of 0.5 to 0.7 in healthy adults. From Shock Index and Early Recognition of Sepsis in the Emergency Department: Pilot Study 2012
Pitfall: Administering plasma for liver patients with an elevated INR [See the Table above]. Patients with liver disease and high INRs are not at the same bleeding risk as those on Warfarin and have high INRs. They will therefore not require the same plasma therapy.
Dr. Jeannie Callum’s 7 T’s for Massive Transfusion Protocol (MTP)
Trigger: Know when, know how to activate your local MTP [See Indications for MTP in UGIB in the table above].
Team: Ensure the lab, nurses, and required consulting services (ICU, hematology) are notified early.
Testing: Q1H labs (don’t forget the fibrinogen level!)
TXA: Most patients receiving massive transfusion will require TXA as well.
Temperature: Maintain body temperature >36. Each degree lower worsens bleeding.
Transfuse to target hemoglobin: Start with 4 units uncrossmatched.
Termination: Know when to stop an MTP based on hemodynamics and hemoglobin level and redirect blood products back to the blood bank for use in other acute patients.
Pitfall: Forgetting to order fibronogen level in patients requiring massive transfusion. An initial fibrinogen is essential to help assess the need for cryoprecipitate administration in the massive GI bleeder.
Platelet replacement for patients on anti-platelet agents
Though intuitive that replacing platelets for those on medications that inhibit platelet function, studies such as the PATCH Trial for intracranial hemorrhage [8] have found that there is an increased risk of death and length of hospitalization due to associated thromboembolism. As such, platelet replacement therapy should probably be avoided in GI bleed patients who are taking anti-platelet agents.
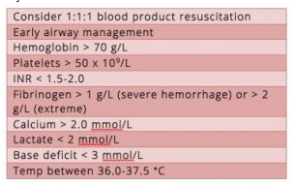
Goals of resuscitation for massive GI bleed
There is little data to guide our resuscitation in this patient population. Extrapolating from trauma literature, there are a few goals recommended by Dr. Callum:
Should Tranexamic Acid (TXA) be given for all patients with GI Bleed?
Our experts recommend administering TXA for all hemodynamically unstable GI bleed patients who do not have specific contraindications (see below).
For UGIB patients there is moderate evidence for improved survival with TXA based on a 2014 systematic review [13]. A 2012 Cochrane review showed no significant difference in bleeding, surgery, or transfusion requirements although there was a trend toward reduction in bleeding and mortality [14]. Overall, there are insufficient data on the effectiveness and safety of TXA use in all-comers with UGIBs. HALT-IT is a large multi-center study in progress looking to assess the impact of TXA on UGIB morbidity and mortality [15]. For LGIB there is no evidence for benefit or harm.
Contraindications to tranexamic acid
- History of coronary stent(s)
- History of active hematuria (it is thought that administration of TXA in the patient with hematuria may cause a clot resulting in obstructive uropathy)
- History of venous thromboembolic disease