What follows are excerpts from the Asystole Case, pp 120 – 128 of the Advanced Cardiac Life Support Provider Manual c. 2016:
Introduction
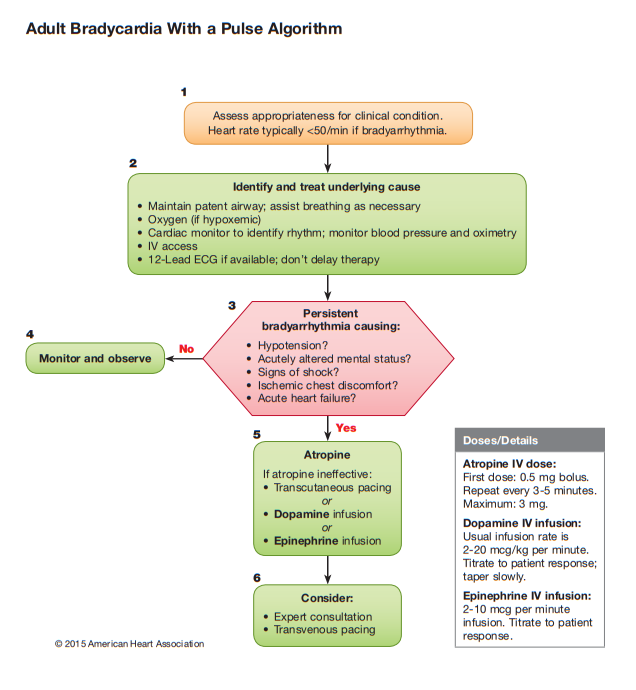
This case discusses assessment and management of a patient with symptomatic bradycardia (heart rate less than 50/min).
The cornerstones of managing bradycardia are to:
- Differentiate between signs and symptoms that are caused by the slow rate versus those that are unrelated
- Correctly diagnose the presence and type of AV block
- Use atropine as the drug intervention of first choice
- Decide when to initiate transcutaneous pacing (TCP)
- Decide when to start epinephrine or dopamine to maintain heart rate and blood pressure
- Know when to call for expert consultation about complicated rhythm interpretation, drugs, or management decisions.
In addition, you must know the techniques and cautions for using TCP.
Rhythms for Bradycardia
This case involves these rhythms:
- Sinus bradycardia
- First-degree AV block
- Second-degree AV block
- Type I (Wenckebach/Mobitz I)
- Type II (Mobitz II)
- Third-degree AV block.
You should know the major AV blocks because important treatment decisions are based on the type of block present. Complete AV block is generally the most important and clinically significant degree of block. Also, complete or third-degree AV block is the degree of block most likely to cause cardiovascular collapse and require immediate pacing. Recognition of a symptomatic bradycardia due to AV block is a primary goal. Recognition of the type of AV block is a secondary goal.
Definitions
Bradyarrythmia or bradycardia [terms are interchangeable]:
Any rhythm disorder with a heart rate less than 60/min — eg, third-degree AV block — or sinus bradycardia. When bradycardia is the cause of symptoms, the rate is generally less than 50/min.
Symptomatic bradyarrhythmia:
Sinus bradycardia may have many causes. [Some need treatment and some don’t – eg a well conditioned athelete]
This case will focus on the patient with a bradycardia and a heart rate less than 50/min. Key to the case management is the determination that the symptoms or signs due to the decreased heart rate. A symptomatic bradycardia exists when 3 criteria are present:
- The heart rate is slow.
- The patient has symptoms.
- The symptoms are due to the slow heart rate.
Signs and Symptoms of Bradycardia
You must perform a focused history and physical examination to identify the signs and symptoms of a bradycardia.
Symptoms include:
- chest discomfort or pain
- shortness of breath
- decreased level of consciousness
- weakness
- fatigue
- light-headedness
- dizziness
- presyncope or syncope
Signs include
- hypotension
- drop in blood pressure on standing (orthostatic hypotension)
- diaphoresis
- pulmonary congestion on physical exam or chest x-ray
- frank congestive heart failure or PE
- bradycardia-related (escape) frequent premature ventricular complexes or VT
Application of the Bradycardia Algorithm
Introduction
In this case, you have a patient presenting with symptoms of bradycardia. You conduct appropriate assessment and interventions as outlined in the Bradycardia Algorithm. At the same time, you are searching for and treating possible contributing factors.
Identification of Bradycardia
Identify whether the bradycardia is:
- Present by definition, ie, heart rate less than 50/min
- Inadequate for the patient’s conduction
Next, perform the Primary Assessment, including the following:
- A – Maintain patent airway
- B – Assist breathing as needed, give oxygen in case of hypoxemia, monitor oxygen saturation.
- C – Monitor blood pressure and heart rate: obtain and review a 12-lead ECG; establish IV access.
- D – Conduct a problem-focused history and physical examination; search for and treat possible contributing factors.
Decision Point: Adequate Perfusion? You must decide if the patient has adequate or poor perfusion:
- If the patient has adequate perfusion, observe and monitor (Step 4 above)
- If the patient has poor perfusion, proceed to Step 5 (above)
Treatment Sequence Summary
If the patient has poor perfusion secondary to bradycardia the treatment sequence is as follows:
- Give atropine as first-line treatment
- Atropine 0.5 mg IV – to a total dose of 3 mg. [You can repeat the dose every 3 to 5 minutes up to the 3 mg maximum]
- If atropine is ineffective
- Begin transcutaneous pacing or
- Dopamine 2 to 20 mcg/kg per minute (chronotropic or heart rate dose)
- Epinephrine 2 to 10 mcg/min
Indications for Transcutaneous Pacing
- Hemodynamically unstable bradycardia (eg, hypotension, acutely altered mental status, signs of shock, ischemic chest discomfort, acute heart failure [AHF] hypotension)
- Unstable clinical condition likely due to the bradycardia
- For pacing readiness in the setting of AMI as follows:
- Symptomatic sinus bradycardia
- Mobitz type II second-degree AV block
- Third-degree AV block
- New left, right, or alternating bundle branch block or bifascicular block
- Bradycardia with symptomatic ventricular escape rhythms
Precautions for TCP are as follows:
- TCP is contraindicated in severe hypothermia and is not recommended for asystole.
- Conscious patients require analgesia for discomfort unless delay for sedation will cause/contribute to deterioration.
- Do not assess the carotid pulse to confirm mechanical capture; eletrical stiulation causes muscular jerking that may mimic the carotid pulse.
Technique: Perform Transcutaneous Pacing are as follows:
- Step 1: Place pacing electrodes on the chest
- Step 2: Turn the Pacer on.
- Step 3: Set the demand rate to approximately 60/min. This rate can be adjusted up or down (based on patient clinical response) once pacing is established.
- Step 4: Set the current milliamperes output 2 mA above the dose at which consistent capture is observed (safety margin).
Most patients will improve with a rate of 60 to 70/min if the symptoms