For much more on the use of ketamine, see my posts, Resources (2) through (7), after this post in Resources below.
The following are extracts from Resource (1) below on IV ketamine for acute pain:
There is an extensive discussion of each of the questions below in text of the article. I have placed each question’s final summary after the question.
Key Questions
Guideline Question 1: Which Patients and Acute Pain Conditions Should Be Considered for Ketamine Treatment?
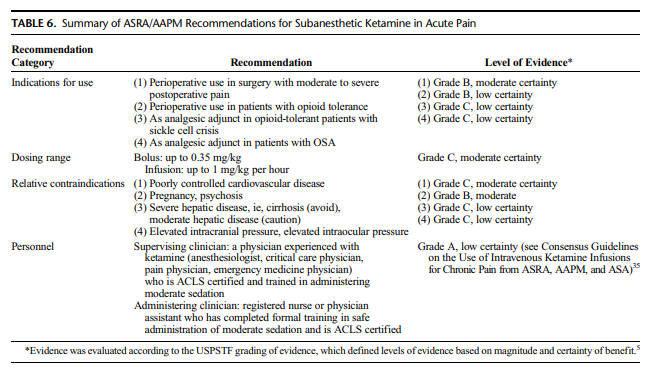
Overall, we conclude that subanesthetic ketamine infusions should be considered for patients undergoing painful surgery (grade B recommendation, moderate level of certainty). Ketamine may be considered for opioid-dependent or opioid tolerant patients undergoing surgery (grade B recommendation,
low level of certainty). Because evidence is limited
to case reports and series as well as the clinical experience of the committee, ketamine may be considered for opioid dependent or opioid-tolerant patients with acute or chronic sickle cell pain (grade C recommendation, low level of certainty). For patients with sleep apnea, ketamine may be considered as an adjunct to limit opioids (grade C recommendation,
low level of certainty).Guideline Question 2: What Dose Range Is Considered Subanesthetic, and Does the Evidence Support Dosing in This Range for Acute Pain?
Therefore, we recommend that ketamine bolus doses do
not exceed 0.35 mg/kg, and infusions for acute pain generally do not exceed 1 mg/kg per hour in settings without intensive monitoring, but we also acknowledge that individual pharmacokinetic and pharmacodynamic differences, as well as other factors (eg, prior ketamine exposure), may warrant dosing outside this range. Ketamine’s adverse effects will prevent some patients from tolerating higher doses in acute pain settings, and unlike for chronic pain therapy, lower doses (ie, 0.1–0.5 mg/kg per hour) may be needed to achieve an adequate balance of analgesia and adverse effects (grade C recommendation, moderate level of certainty).Guideline Question 3: What Is the Evidence to Support Ketamine Infusions as an Adjunct to Opioids and Other Analgesic Therapies for Perioperative Analgesia?
Overall, we conclude that moderate evidence supports use of subanesthetic IV ketamine bolus doses (up to 0.35 mg/kg) and infusions (up to 1 mg/kg per hour) as adjuncts to opioids for perioperative analgesia (grade B recommendation, moderate level of certainty).
Guideline Question 4: What Are the Contraindications to Ketamine Infusions in the Setting of Acute Pain Management, and Do They Differ From Chronic Pain Settings?
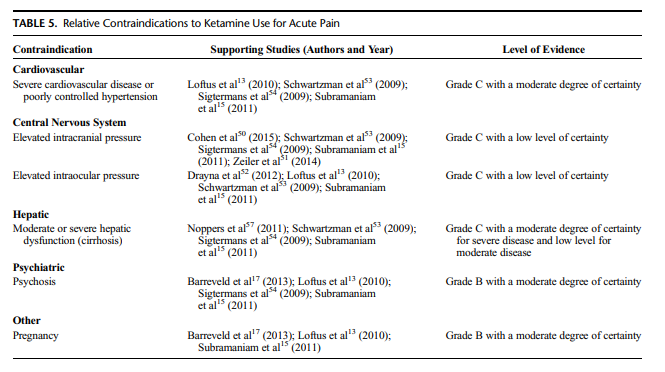
Evidence indicates that ketamine should be avoided in
individuals with poorly controlled cardiovascular disease (grade C evidence, moderate level of certainty) and pregnancy or active psychosis (grade B evidence, moderate level of certainty). For hepatic dysfunction, evidence supports that ketamine infusions should be avoided in individualswith severe disease (eg, cirrhosis) and used with caution (ie, with monitoring of liver function tests before infusion and during infusions in surveillance of elevations) in individuals
with moderate disease (grade C evidence, low level
of certainty). Evidence indicates that ketamine should be avoided in individuals with elevated intracranial pressure and elevated intraocular pressure (grade C evidence, low level of certainty). Relative contraindications are shown in Table 5.Guideline Question 5: What Is the Evidence to Support
Nonparenteral Ketamine for Acute Pain Management?Based on a review of these studies, we conclude that the
use of IN ketamine is beneficial for acute pain management, providing not only effective analgesia but also amnesia and procedural sedation. Particular scenarios in which this should be considered include individuals for whom IV access is difficult and children undergoing procedures (grade C recommendation,
low-to-moderate level of certainty). For oral ketamine,
the evidence is less robust, but small studies and anecdotal reports suggest it may provide short-term benefit in some individuals with acute pain (grade C recommendation, low level of certainty).Guideline Question 6: Does Any Evidence Support Patient-Controlled IV Ketamine Analgesia forAcute Pain?
Overall, we conclude that evidence is limited for the benefit of IV-PCA–delivered ketamine as the sole analgesic for acute or periprocedural pain (grade C recommendation, low level of certainty). We conclude that moderate evidence supports the benefit of the addition of ketamine to an opioid based IV-PCA for acute and perioperative pain management (grade B recommendation, moderate level of certainty).
FUTURE DIRECTIONS AND CONCLUSIONS
By current standards, ketamine is an old drug that has been
used clinically as an anesthetic agent since the 1970s.76 The desire for analgesic alternatives to opioids, especially in light of the current public health crisis and evidence that short-term opioid use may lead to chronic opioid therapy in some patients,77 has led to renewed interest in the use of ketamine as an analgesic in the acute pain setting. . . . These guidelines have attempted to summarize existing literature with a particular focus on crucial issues that directly impact ketamine’s use in acute pain, including expert opinion when evidence is lacking.
The published evidence demonstrates a clear short-term, opioid sparing effect when ketamine is used in subanesthetic doses as a
perioperative adjunct, regardless of whether it is given as a bolus, infusion, or via PCA.Nonparenteral ketamine, especially IN ketamine, is likely to
continue to increase in use for acute exacerbations of chronic pain conditions. It has been studied mostly in the emergency medicine setting, where it provides brief but potent analgesia, especially for procedures. Studies focused on long-term use of IN ketamine are important to establish sustained benefit and better characterize the adverse effect profile. The lack of FDA approval of nonparenteral ketamine formulations for any indication will likely make these studies difficult to perform.In conclusion, despite its drawbacks, ketamine remains a powerful and inexpensive tool for practitioners who manage
acute pain. We believe its use will continue to expand as more
institutions treat increasingly challenging patients in the perioperative period as well as those with painful disease exacerbations while trying to combat the opioid epidemic. More research is needed to refine selection criteria for the treatment of acute pain and possible prevention of chronic pain, to determine the ideal dosing and treatment regimen to include coadministration of ketamine with opioids and adjuvants, and to better understand the long-term risks of ketamine in patients who receive serial treatments for frequent acute pain exacerbations.
Resources:
(1) Consensus Guidelines on the Use of Intravenous Ketamine Infusions for Acute Pain Management From the American Society of Regional Anesthesia and Pain Medicine, the American Academy of Pain Medicine, and the American Society of Anesthesiologists [PubMed Abstract] [Download PDF]. Reg Anesth Pain Med. 2018 Jun 7. doi: 10.1097/AAP.0000000000000806. [Epub ahead of print].
(2) Ketamine Induced Laryngospasm – A Link To Guidance From First10EM And Other Resources Posted on August 27, 2017 by Tom Wade MD.
(3) Links To Laryngospasm After Ketamine From Resus.me and Two Other Resources
Posted on October 17, 2016 by Tom Wade MD
(4) Ketamine for Analgesia AND MORE From Dr. Fox
Posted on October 16, 2016 by Tom Wade MD
(5) Ketamine Use In The Emergency Department (ACEP Guideline)
Posted on September 28, 2015 by Tom Wade MD
(6) Etomidate and Ketamine for Rapid Sequence Intubation
Posted on April 24, 2012 by Tom Wade MD
(7) The Seven Ps of Rapid Sequence Intubation
Posted on April 23, 2012