Following rapid sequence intubation (RSI), the physician will iniate mechanical ventilation.
Recommended initial ventilator settings for adult patients: (1)
Mode Assist Control (AC)
Tidal Volume (Vt) 7 ml per kg IBW
Frequency (f) 12 to 20 breaths per minute
Fraction of Inspired O2 (FiO2) 1.0
Positive End Exiratory Pressure (PEEP) 5.0 cm
Inspiratory Flow Rate (IFR) 60 L per minute
Recommendations for mechanical ventilation for adult patients with outflow obstruction: (2)
Use as large an ETT as possible
Cut the ETT to minimize the length
See RR of 8 to 10 breaths per minute
Set tidal volume of 6 to 7 cc per kg IBW
Increase the IFR to 90 to 120 L per minute
Ventilation Modes
Three commonly used modes of mechanical ventilation are:
Control Mode Ventilation (CMV)
Assist Control (AC)
Synchronized Intermittent Mandatory Ventilation (SIMV with or without Pressure
Support [PS])
The ventilation mode is characterized by three variables: the trigger, the limit, and the cycle (mneumonic—TLC).
The trigger is the variable that ventilator sensors monitor to initiates the mechanical ventilation, the tidal volume. The trigger may be a fall in the ventilatory circuit pressure when the patient tries to take a breath. The trigger may be time from the onset of the last breath. In this case the ventilator is time triggering as in a patient who has no or a very low spontaneous respiratory rate.
The limit is the variable that the ventilator sensors monitor to regulate the inspiration. The variable may be rate of airflow or it may be the airway pressure.
The cycle is the variable that the ventilator sensors monitor to terminate the inspiration. The variable may be either a set volume delivered (in volume cycled ventilation) or set pressure delivered over a set time period (in pressure cycled ventilation). And finally, the cycle variable may be a change in the ventilator circuit pressure when the patient ends his inspiratory effort (in pressure support ventilation).
“Assist control (AC) is the preferred mode for patients in respiratory distress. The clinician sets the tidal volume (TV or Vt), respiratory rate (RR), inspiratory flow rate (IFR), peak end expiratory pressure (PEEP), and the fractional concentration of inspired oxygen (FiO2). In contrast to all other modes, the trigger that initiates inspiration can be either patient effort or an elapsed time interval.”* (3)
*In control mode ventilation (CMV) which is usually used in the operating room, it is the ventilator sensors that trigger, limit, and cycle all of the breaths; the patient cannot trigger a ventilation. Synchronized intermittent manatory ventilation (SIMV with or without pressure support) basically is equivalent to assist control mode if the patient’s intrinsic respiratory rate is below the rate set by the ventilator. SIMV is basically only pressure support ventilation if the patient intrinsic respiratory rate is above the machine set rate. If the patient’s spntaneous respiratory rate is above the ventilator set rate, SIMV can lead to excessive work of breathing. Both CMV and SIMV are well discussed in the reference.
Volume Cycled Ventilation
In volume cycled ventilation, the flow rate is selected and in adults the initial peak flow rate is usually set at 60 L per minute. With volume cycled ventilation, the rate of flow can be varied, thus changing the peak inspiratory pressure (PIP) and inspiratory time (Ti) for the selected tidal volume. The limit variable is the airflow rate. And the cycle variable is the selected tidal volume.
Pressure Cycled Ventilation
In pressure cycled ventilation the limit variable is the set airway pressure. The cycle variable is the inspiratory time (Ti). And the tidal volume can vary from breath to breath based on a number of factors including airway resistance, patient effort, and lung compliance. Thus the tidal volume is indirectly controlled by the selected airway pressure and inspiratory time. Airway pressure and inspiratory time should be selected so that tidal volume is 7 ml per kg of ideal body weight.
The inspiratory to expiratory ratio (I/E ratio) is the inspiratory time divided by the expiratory time and is normally 1:2.
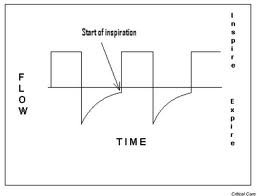 “The I/E ratio is usually determined by simply observing the pressure and flow waveforms on the ventilator monitor. After the inspiratory pressure is adjusted to meet the goal Vt, the Ti is adjusted while monitoring end-expiratory flow. Terminal end expiratory flow should approach zero to confirm expiration is complete, and there is no retained Vt in the thorax. Even small volumes of retained Vt are quickly compounded by the ventilator and lead to dynamic hyperinflation with increased intrathoracic pressure known as auto-PEEP.” (4)
“The I/E ratio is usually determined by simply observing the pressure and flow waveforms on the ventilator monitor. After the inspiratory pressure is adjusted to meet the goal Vt, the Ti is adjusted while monitoring end-expiratory flow. Terminal end expiratory flow should approach zero to confirm expiration is complete, and there is no retained Vt in the thorax. Even small volumes of retained Vt are quickly compounded by the ventilator and lead to dynamic hyperinflation with increased intrathoracic pressure known as auto-PEEP.” (4)
Manual of Emergency Airway Management 4th ed, 2012. RM Walls and MF Murphy. p. 65.
Ibid.
Ibid., p. 61.
Ibid., p. 64.




