Today, I review, link to and excerpt from The Cribsiders’ #92: Don’t Miss a Beat: Evaluation of Stable Arrhythmias in the Outpatient Setting.* August 30, 2023 | By Sam Masur.
*Ledingham L, Kamp A, Raymond-Kolker B, Cruz M, Masur S, Chiu C, Berk J. “92: Don’t Miss a Beat: Evaluation of Stable Arrhythmias in the Outpatient Setting”. The Cribsiders Pediatric Podcast. https:/www.thecribsiders.com/ August 30, 2023.
All that follows is from the above resource.
AUDIO
Summary:
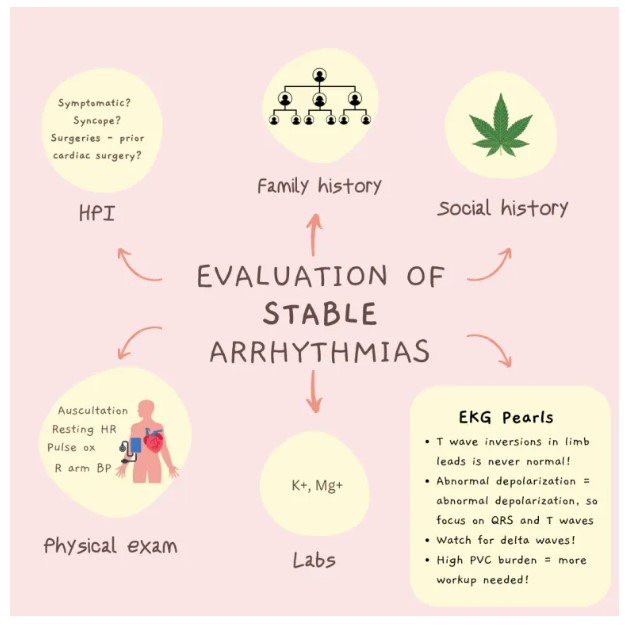
Does hearing about your patient’s palpitations give YOU palpitations because you don’t know what to do next? Treat your tachycardia with this episode of the Cribsiders, as we talk with special guest Dr. Anna Kamp, a pediatric electrophysiologist at Nationwide Children’s Hospital, about her approach to stable arrhythmias in the outpatient setting. We learn about “red flags” in the history and physical exam that warrant immediate referral to cardiology, whether you should order an echo or event monitor before sending a patient to cardiology, and how you can incorporate wearable EKG technology into your practice.
Arrhythmia Pearls
- Palpitations with syncope, whether occurring at rest or with exercise, is never benign and should always warrant an urgent referral to cardiology.
- Sudden death due to cardiac causes is very rare in children; however, if you are questioning whether you need to exercise restrict your patient, you should refer to cardiology.
- In addition to obtaining symptom history, take a detailed family and substance use history to help risk stratify patients with possible arrhythmias. Recreational marijuana has a very strong association with tachyarrhythmias.
- You should order an EKG and basic chemistry at the initial primary care visit. You do not need to order an event monitor, and only very rarely should think about ordering an echo before sending the patient to cardiology (see below).
- Situations that always warrant an echo include a neonate with SVT, exertional syncope even in the presence of a normal EKG, and in a patient with Wolff-Parkinson-White syndrome.
- Abnormal depolarization leads to abnormal repolarization, so make sure to study the QRS interval and T waves in your EKG. Inverted T waves in the limb leads are never normal and should raise your suspicion for underlying myocardial disease predisposing to arrhythmia.
- The best way to use smart technology with EKG capabilities is to teach the patient how to record an EKG when they are symptomatic. They can then bring this strip into the cardiology office for more accurate interpretation.
- As a pediatric resident or general practitioner, know what you know and what you don’t. When you’re out of your scope, do not hesitate to take advantage of your resources and your colleagues’ expertise.
Common Pediatric Arrhythmias
These vary by age. The “can’t miss” arrhythmias also vary by age, as SVT in a neonate who cannot express symptoms is far more dangerous than SVT in a teenager who is able to complain about the presence of palpitations and will get treated faster. A neonate with SVT is also more concerning because there is a strong association between SVT in the neonatal period and congenital heart disease.
Neonatal period
- Premature atrial contractions.
- Premature ventricular contractions.
- Can’t miss: SVT – infant can’t tell you they’re in it, so can sit for weeks and present with severe cardiac dysfunction.
Childhood
- Sinus arrhythmia: Not a true arrhythmia but can present very profoundly.
Teenagers
- SVT: 1 in 250 children.
- PACs and PVCs are also frequent, but patients are usually asymptomatic so may be unrecognized .
Key Elements of the History
Have you had any syncopal episodes?
- Palpitations with syncope are never normal and always warrant a stat referral to cardiology.
- Exertional syncope also warrants a stat referral to cardiology, and you should call your cardiologist after placing the referral to make sure the patient is seen in a timely fashion.
Do you have symptoms? If so:
- What do the symptoms feel like?
- How long do they last?
- Is there a trigger?
- Do they happen when you’re at rest?
- Do they happen when you’re active or both?
- Do you have any associated dizziness or syncope? If so, see above.
Family History:
- Any known family history of cardiac disease, particularly cardiac disease diagnosed at a young age?
However, many patients will not know if there is a history of cardiac disease. Therefore, more focused questions include:
- Has anyone ever died as a single driver in an automobile accident at a young age?
- Has anyone died via drowning?
- Has anyone had a lot of miscarriages?
Substance Use History:
- Marijuana has a strong documented associated with tachyarrhythmias.
Physical Exam and Initial Workup
- Vitals are vital: make sure to document a resting heart rate, right arm blood pressure (don’t miss a coarctation regardless of the patient’s age!), and a pulse oximetry reading.
- If a resting heart rate is abnormal, you should not attribute the symptoms to anxiety.
- Always order an EKG as part of the vitals.
- Basic metabolic panel to rule out electrolyte abnormalities.
- Do not order a Holter or event monitor, as this may delay care. It is easier to let the cardiologist decide if they want one. It is also important to consider that Holter and event monitors are very expensive and are unlikely to truly document an arrhythmia if the patient is only experiencing symptoms once every 3 months.
- You do not need to order an echocardiogram unless you have a patient in the following situations: a neonate with SVT, a child with exertional syncope (even if the EKG is normal!), or a child with Wolff-Parkinson-White syndrome.
How to risk stratify these patients
Higher risk features of the history and physical include the presence of symptoms (particularly syncope), history of repaired congenital heart disease, and the presence of a murmur on exam. “Triggers” vary greatly by person and are less helpful in risk stratification, as both a deconditioned patient walking around the block and a high school athlete at practice in hot weather may perceive benign sinus tachycardia as uncomfortable.
Arrhythmia diagnosis
EKG is the only way to record and diagnose an arrhythmia. Asking about the timing of symptoms in the history is key because this will help determine whether you will be able to document an arrhythmia. Ways to document an arrhythmia include: the standard 12 lead EKG, which provides a snapshot in time; a 24 hour Holter monitor, which records every heart beat over a 24 hour period; a 14 or 30 day event monitor; and rarely, an implantable monitor with a battery life of 3 – 5 years. If you believe that patient symptoms correspond with the arrhythmia and the patient is only having symptoms once every few months, the chances of capturing this arrhythmia for diagnosis is much lower.
What to look for in the EKG in the evaluation of an arrhythmia
- Who is reading it: studies have shown that EKGs are more accurately read by pediatric cardiologists than general internists. Be cautious when responding to the “official” read if you are unsure who has read it or if they are adequately trained to interpret pediatric EKGs.
- If the patient is symptomatic, watch for WPW as it has a relatively high prevalence (1 in 500 kids).
- Abnormal depolarization leads to abnormal repolarization, so pay special attention to QRS and T wave morphology. Inverted T Waves in limb leads is not normal at any age and should cause you to think about myocardial disease that predisposes to unsustained arrhythmias.
- EKGs are very malleable and there is significant intrapatient variation. If you are not sure if an EKG is abnormal in the absence of symptoms, schedule a follow up appointment to repeat the EKG in the future to compare the two.
- A normal EKG does not exclude every potential cause of sudden cardiac death.
Should I care about PVCs?
- There is limited data studying PVCs in children. In adults, studies have shown individuals with a >25% PVC burden can still have a structurally normal heart but there have also been studies showing a high PVC burden is associated with the development of cardiac dysfunction.
- If there is a high PVC burden in children, you should make sure that the patient is not developing cardiac dysfunction and also attempt to identify the underlying etiology of PVCs (i.e. structural vs electrolyte abnormality).
- The burden of PVCs affects follow-up from a cardiology standpoint.
- Make sure to look at the sinus beats surrounding the PVC. If these beats are abnormal, this is concerning for cardiomyopathy and further evaluation is warranted.
Should I get a screening EKG for sports clearance?
- Screening EKGs are not as beneficial as a thorough history and exam because they are dependent on variable factors such as lead placement, interpreter, etc.
- Sinus bradycardia alone in otherwise healthy and asymptomatic athletes is not cause for concern and does not necessitate referral to cardiology.
- QT abnormality, QRS prolongation, or any AV block or voltage criteria for LVH should be referred to cardiology for further evaluation.
Role of patient wearables in documenting arrhythmias
- Patient wearables refer to smart watch technology and other newer monitoring devices that can be purchased online.
- These are usually single lead but are actually very good quality. To note, even Holter and event monitors are only single lead.
- Patient wearable algorithms to diagnose arrhythmias are not designed for or tested in pediatric populations. Make sure to tell your patient and families to ignore the automatic read as it is not accurate in the pediatric population especially!
- Wearables are very helpful in the pediatric population if the patient and family is trained to record an EKG when they are feeling symptoms. They can then bring this to the cardiologist for direct interpretation. So, train your patients with smart watches how to record an EKG!
- Another advantage is affordability: patient wearables are frequently much less expensive ($100 – $300) than Holter or event monitors, which may cost upwards of $2000.
- The disadvantages to patient wearables are that the patient needs to be symptomatic in order to recognize when to record an EKG, so it may miss asymptomatic arrhythmias and there is currently no way to bill for interpretation of patient wearable device data.
How to counsel families
If there are concerning features in the history or exam as discussed above, you should refer to cardiology for further evaluation and counseling. However, if the history, physical exam, including EKG, and the family history are reassuring, there is a very low chance that this is anything life threatening. Sudden death due to cardiac causes occurs very, very rarely in children: only 1 to 2 per 100,000 patient years. Counsel families on the “red flags”, such as syncope with palpitations, that would warrant further evaluation. As a general rule of thumb, patients should take it easy during exercise and participation in sports if they are not feeling well. Make sure to warn families that automatic readings of smart watch technology and patient wearables are rarely accurate in children and reinforce the importance of using these devices to capture an EKG if the patient is symptomatic that they can then bring to the cardiologist for interpretation. Families can work to further reduce risk by encouraging schools to have AEDs and have staff members that are trained to use them.