I’m taking the upcoming the Pediatric Trauma Life Support Course at IU Health’s Emergency Response Training Institute. And these are excerpts
The Course uses the textbook, Pediatric Trauma Life Support For Prehospital Care Providers, 3rd Edition, 2009. There is a free 2017 online update PDF.
This post is on notes from the Chapter 10 of textbook along with additional resources.
Here are excerpts:
Introduction
According to the Center for Disease Control, in the United States,children with head injuries result in 435,000 emergency department visit a year and more than 2,600 deaths annually. Although most head trauma is minor, 80 percent to 90 percent of pediatric trauma.
Brain Injuries
The brain, as a result of trauma, can sustain both primary and secondary injury. Primary injury occurs as a direct result of trauma (i.e., skull fractures, contusions, lacerations, and concussions). Once incurred, this injury is seldom influenced by therapeutic interventions. . . . Complications from other injuries, such as hypoxia (lack of oxygen), hypercapnia (lack of ventilation), or shock (lack of tissue perfusion) all further aggravate the overall severity of injury [causing secondary brain injury].
Treatment of the head-injured child is aimed at preventing the secondary injury and, thus, improving outcome.
Pearls:
Bleeding may be significant from a scalp wound and frighten the child, parents and the prehospital provider. Remember to use basic wound management, especially direct pressure , on the wound.
A child’s head is the largest part of his body, especially in infancy, when it is 25 percent of their total body. Suspect head injury in any child with a signicant mechanism of injury.
It is the prehospital provider’s job to prevent secondary injury to the brain by providing adequate oxygenation, ventilation and perfusion. Care attention to ABCs can help to identify the need for correct intervention.
Avoid hyperventilation; provide adequate ventilation with 100% oxygen to the head-injured child. Contact medical direction in the event of rapid deterioration of the child.
Assume that any child with an altered mental status has a head injury.
Prolonged seizure activity, even without a history of trauma, may be a sign of an occult head injury. Consider stabalization of the cervical spine. This will also help maintain neutral positioning of the airway. This will also help maintain neutral position of the airway.
Summary
- Head trauma is the leading cause of traumatic death in the pediatric population.
- The large side of the head and weak neck muscles of children predispose them to serious head injury.
- Careful assessment and appropriate interventions such as oxygenation, appropriate ventilation, and maintenance of cerebral blood flow are necessary to prevent secondary brain injury and to control intracranial pressure.
- All serious head injuries should be considered life-threatening and require aggressive management of the ABCs,
- Rapidly package any child with an altered mental status and transport to the nearest appropriate facility.
- Currently, the only indication for hyperventilation is in the child with impending cerebral herniation.
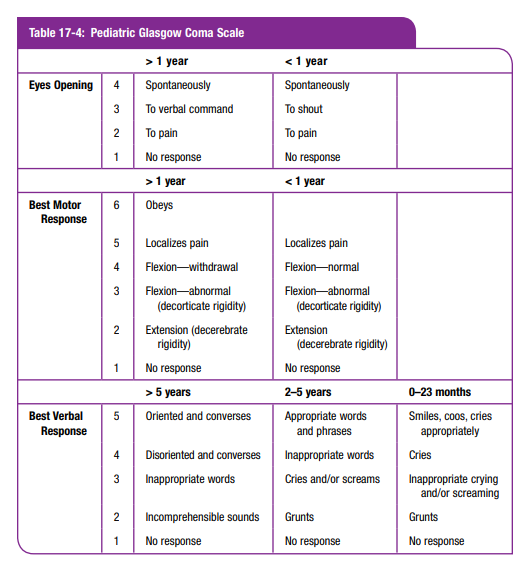
The above chart is from The International Trauma Life Support Course For Emergency Care Providers, 8th ed, 2016. [Please note, this is not an affiliate link.]




