This blog and the posts on it are my study notes which I put up to help me reinforce my learning on the subjects I review.
I’m reviewing all of the excellent diagnostic schemas from the Clinical Problem Solvers.
And today I review the diagnostic schema, Lymphedema [This link is to the web page where the video of this schema is reviewed. I’ve also embedded the video below].
Here is the link to the Lymphedema and Dyspnea podcast:
Here is the Diagnostic Schema For Lymphedema [Link is to the PDF]:
Here are the show notes of Episode 33 [Link is to the PDF]:
Episode 33
Problem Representation
A 58-year-old man with a history of lower extremity lymphedema and COPD presented with subacute dyspnea, found to have bilateral chylothoraces and nail dystrophy.
Schemas
The CPSers’ schema for pleural effusions utilizes Light’s criteria (fluid protein/serum protein ratio > 0.5; fluid/serum LDH ratio > 0.6; pleural fluid LDH > 200 IU or >2/3 of the upper limit of
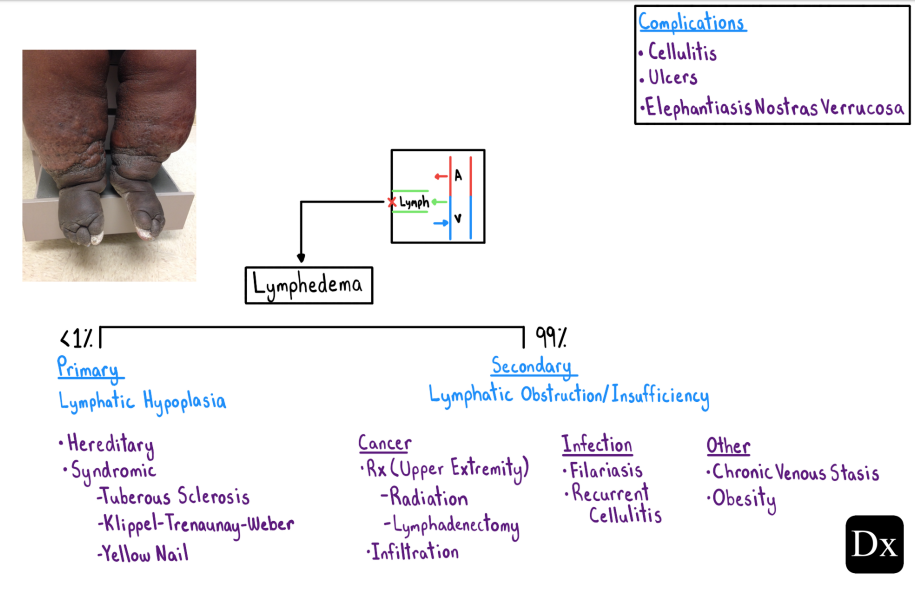
normal) to distinguish between transudative and exudative effusions.We also included a schema for lymphedema that distinguishes between primary (due to lymphatic hypoplasia) and the far more common secondary (due to lymphatic obstruction/insufficiency) causes of lymphedema.
Diagnosis
Based on the findings of nail dystrophy, lymphedema, and chylothorax, the patient was found to meet diagnostic criteria for yellow-nail syndrome, a rare cause of primary lymphedema and pulmonary findings!
Teaching points
- A chylothorax1 occurs when chyle (milky fluid containing lymph and fats transported by
chylomicrons) accumulates in the pleural space. This most commonly occurs due to
disruption of the thoracic duct secondary to trauma during surgery or as the result of
malignant compression. The diagnosis is supported by finding elevated triglyceride levels
(i.e. > 110 mg/dL) in the pleural fluid.- Lymphedema2 refers to the accumulation of protein-rich interstitial fluid that occurs due to impaired lymphatic drainage in the setting of normal capillary function. The most common cause of secondary lymphedema worldwide is lymphatic filariasis3 (infection with Wuchereria bancrofti or Brugia malayi), while malignancy/cancer treatment and cellulitis predominate in the developed world. Complications of lymphedema include recurrent
skin infections (due to regional immune dysfunction), cutaneous ulceration, and elephantiasis nostras verrucosa (hyperkeratotic skin changes).- Yellow-nail syndrome4 (YNS) is a rare syndrome (~1/1,000,000 people) characterized by
dystrophic/discolored nails, pulmonary abnormalities, and primary lymphedema. While the etiology of this syndrome is unknown, its pathogenesis is thought to largely be related to impaired lymphatic flow. Respiratory manifestations include cough, pleural effusions (including chylothoraces), bronchiectasis, and recurrent sino-pulmonary infections.Clinical Reasoning Pearl
As learners, we will inevitably encounter clinical scenarios with which we are unfamiliar. In those instances, our reasoning should then focus on how to best describe the problem, so that someone familiar with the diagnosis (or our search engine) may immediately recognize it.
For example:
Reza ultimately turned to google to help him solve the case – but not before destilling down what he believed to be the essential descriptive elements of the patient’s presentation.References
1. McGrath EE, Blades Z, Anderson PB. Chylothorax: aetiology, diagnosis and therapeutic options. Respir Med. 2010
Jan;104(1):1-8.
2. Taylor MJ, Hoerauf A, Bockarie M. Lymphatic filariasis and onchocerciasis. Lancet. 2010 Oct 2;376(9747):1175-85.
3. Grada AA, Phillips TJ. Lymphedema: Pathophysiology and clinical manifestations. J Am Acad Dermatol. 2017
Dec;77(6):1009-1020.
4. Vignes S, Baran R. Yellow nail syndrome: a review. Orphanet J Rare Dis. 2017 Feb 27;12(1):42.