In this post I link to the podcast and show notes of Emergency Medicine Cases‘ EM Quick Hits 17 Adrenal Crisis, Strep Throat, Posterior MI, DKA Just the Facts, Ovarian Torsion Imaging, HINTS Exam, Canadian CT Head Rule, April 2020.
For this post I’ll review Drs Justin Yan & Hans Rosenberg‘s outstanding review of Just The Facts Approach To Diabetic Ketoacidosis, which runs from 18:24 to 23:24 [link to the complete podcast and show notes].
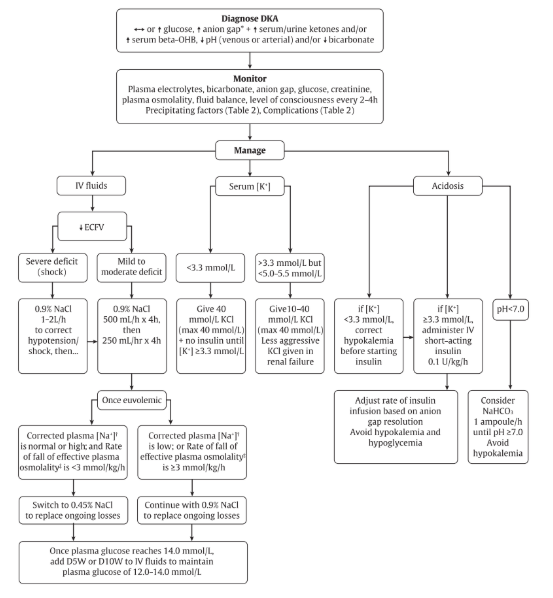
Here is the Outstanding Flow Chart:
Here are the show notes:
DKA – Just the Facts
- Diagnostic criteria for diabetic ketoacidosis are not well defined, however
- Serum pH and bicarbonate are usually low (≤7.30 and ≤15.0 mmol/L, respectively)
- Serum or urine ketones are usually positive
- Typically, the anion gap is elevated (>12 mmol/L) and serum blood glucose is high, but normal blood glucose does not preclude the diagnosis of DKA as euglycemic DKA may occur in specific instances (e.g., pregnancy, sodium-glucose co-transporter 2 inhibitor use, food restriction, and alcohol use).
- Negative urine ketones should not be used to rule out diabetic ketoacidosis, as urine tests measure the presence of acetoacetate, but not beta-hydroxybutyrate
- “5 I’s” mnemonic for DKA precipitants: infection, ischemia (e.g., myocardial, cerebral, and mesenteric), insulin omission, intoxication (e.g., alcohol and sympathomimetics), and iatrogenic (e.g., drugs or dextrose-containing infusions); additional causes include a new diabetes diagnosis, trauma, thyrotoxicosis, and other metabolic disorders
- Goals of initial DKA treatment are to:
- Correct fluid deficits (for non-shock patients, IV NS boluses of 500 mL/h should be initiated and may be repeated until euvolemic – usually for at least 4 hours – and then continued at 250 mL/h for 4 hours)
- Replace potassium (If serum K is <3.3 mmol/L, 40 mmol/L of KCl should be administered, and insulin should be withheld until levels are ≥3.3 mmol/L; if serum K is normal, 10–40 mmol/L KCl should be given in the IV fluid; if the patient is hyperkalemic, potassium should be withheld until less than 5.0–5.5 mmol/L and diuresis occurs; KCl should also be administered less aggressively to those with renal failure)
- Treat hyperglycemia (IV short-acting insulin therapy should begin at 0.1 units/kg/hour and adjusted based on the anion gap resolution while avoiding hypoglycemia or hypokalemia; insulin boluses are no longer recommended.)
- Treat acidemia (Sodium bicarbonate is not routinely recommended but may be considered for cases with severe acidemia (serum pH <7.0) or shock; insulin should be continued until acidosis and anion gap resolve)