This post features links to Emergency Medicine Cases‘ outstanding Episode 91 Occult Knee Injuries Pearls and Pitfalls [Link is to the podcast and show notes] Written Summary and blog post by Dr Anton Helman January, 2017.
I went ahead and excerpted the show notes for this podcast because it helps me put the episode in my memory. Also I’ve included some extras in the post.
Here is a direct link to the Episode 91 podcast.
The show notes of this podcast are outstanding and just need to be reviewed completely including the YouTube videos embedded in the show notes.
Here are some excerpts from Episode #91:
Physical exam pearls for occult knee injuries
Many patients with acute knee injuries in the ED will experience a lot of pain and often clinicians short-change their examination of the knee because they don’t want to cause more pain. However, there are several tips to help the patient relax enough to do provocative testing and the essential maneuvers:
Patient must be supine on a stretcher (not sitting in a chair) with both knees fully exposed.
Place a pillow or roll under the distal femur so that the knee is relaxed at about 20 degrees of flexion to allow for provocative knee testing.
Always perform an active straight leg raise to assess for extensor mechanism function (quadriceps or patella tendon rupture).
“The lateral joint line is the dark corner of the knee exam” – examine the lateral joint line in addition to the medial joint line to assess for the possibility of a lateral tibial plateau fracture in the setting of a valgus mechanism of injury.
Occult Knee Dislocation
About 20-50% of all knee dislocations spontaneously reduce before the patient arrives at the ED.
A significant minority of occult knee dislocations will have neurovascular injuries which if missed, may lead to ischemic complications and even limb amputation.
When to suspect an occult knee dislocation:
- Three of the 4 knee ligament disruption or ligamentous laxity in multiple directions (a “loose knee”)
- A ‘buckling’ knee with a foot drop (common peroneal nerve palsy)
- If upon lifting up the patient’s leg by their heels the knee falls into hyper-extension compared to the contralateral knee
- High energy mechanism of injury or low energy mechanism in patients with BMI>40
Clinical Pearl: Three out of four knee ligament laxity (ACL, PCL, MCL, LCL) is suspicious for an occult knee dislocation
The presence of normal distal pulses and a normal Ankle Brachial Index >0.9 (ABI) does not completely rule out occult popliteal artery injury. If you suspect an occult knee dislocation, refer immediately to orthopedics as revascularization within 6-8 hours of popliteal artery injury is recommended to prevent ischemic complications. While almost all patients with suspected knee dislocation used to get a CT angiogram to assess for vascular injury, the current thinking is that the vast majority of patients who do have a vascular injury with normal serial neurovascular exams and normal serial ABIs have intimal tears that do not require surgery and so these patients can be simply anticoagulated and admitted for observation without a CT angiogram.
Caution: Low-energy trauma can cause knee dislocations, especially in patients with a BMI>40. Obese patients with low-energy trauma were more likely to have associated neurovascular injury than high-energy trauma patients in one study.
Occult Knee Dislocation Take Home
Don’t send home patients who tell you that it felt like their knee popped out of place and they have a big swollen knee with laxity in multiple directions on exam, until you’re sure they haven’t had a vascular injury related to a self-reduced knee dislocation. Even if they have palpable peripheral pulses and a normal ABI, speak to your orthopedic surgeon, consider getting a CT angiogram to rule out a popliteal injury, admit, and consider the same in any obese person even with a low force mechanism.
Occult Knee Dislocation
About 20-50% of all knee dislocations spontaneously reduce before the patient arrives at the ED.A significant minority of occult knee dislocations will have neurovascular injuries which if missed, may lead to ischemic complications and even limb amputation.
When to suspect an occult knee dislocation:
Three of the 4 knee ligament disruption or ligamentous laxity in multiple directions (a “loose knee”)
A ‘buckling’ knee with a foot drop (common peroneal nerve palsy)
If upon lifting up the patient’s leg by their heels the knee falls into hyper-extension compared to the contralateral knee
High energy mechanism of injury or low energy mechanism in patients with BMI>40
Clinical Pearl: Three out of four knee ligament laxity (ACL, PCL, MCL, LCL) is suspicious for an occult knee dislocationThe presence of normal distal pulses and a normal Ankle Brachial Index >0.9 (ABI) does not completely rule out occult popliteal artery injury. If you suspect an occult knee dislocation, refer immediately to orthopedics as revascularization within 6-8 hours of popliteal artery injury is recommended to prevent ischemic complications. [Emphasis Added] While almost all patients with suspected knee dislocation used to get a CT angiogram to assess for vascular injury, the current thinking is that the vast majority of patients who do have a vascular injury with normal serial neurovascular exams and normal serial ABIs have intimal tears that do not require surgery and so these patients can be simply anticoagulated and admitted for observation without a CT angiogram. [I’d get a CT angiogram unless the patient was promptly admitted to the orthopedics service and they said not to–Just my personal non-expert opinion.]
Caution: Low-energy trauma can cause knee dislocations, especially in patients with a BMI>40. Obese patients with low-energy trauma were more likely to have associated neurovascular injury than high-energy trauma patients in one study.
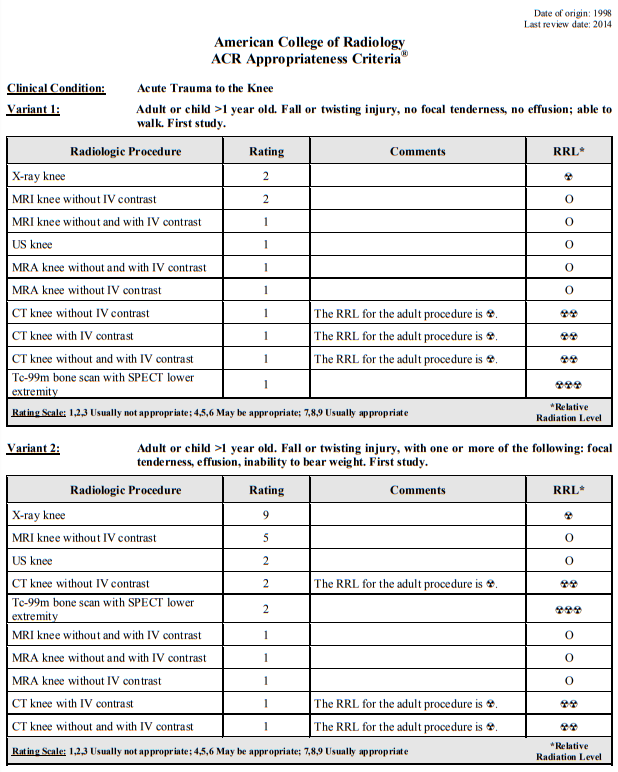
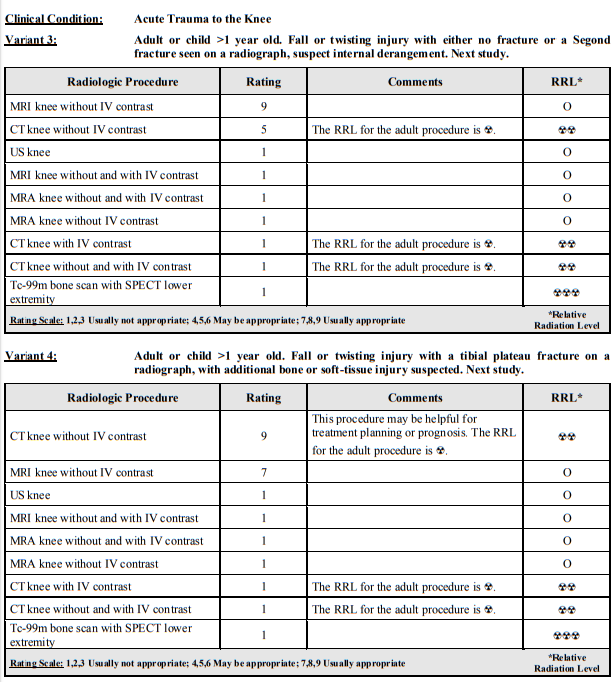
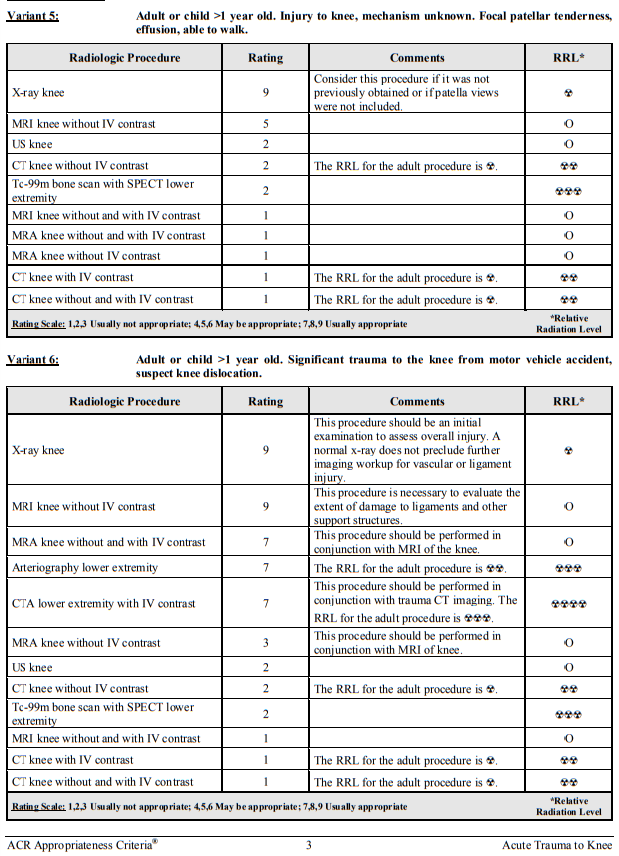
Here is an excerpt from from Resource (9) (9) American College of Radiology ACR Appropriateness Criteria® Clinical Condition: Acute Trauma to the Knee Date of origin: 1998 Last review date: 2014.
Occult Knee Dislocation Take Home
Don’t send home patients who tell you that it felt like their knee popped out of place and they have a big swollen knee with laxity in multiple directions on exam, until you’re sure they haven’t had a vascular injury related to a self-reduced knee dislocation. Even if they have palpable peripheral pulses and a normal ABI, speak to your orthopedic surgeon, consider getting a CT angiogram to rule out a popliteal injury, admit, and consider the same in any obese person even with a low force mechanism.
Reduction of Knee Dislocation
X-ray pearls for subtle lateral plateau fractures
- Normally the lateral subchondral line is higher (more proximal) than the medial one; if, on the AP or lateral x-ray, the lateral subchondral line is at a lower horizontal level compared to the medial one, assume a depressed lateral tibial plateau fracture.
- Scrutinize the oblique view for a depressed lateral tibial plateau.
Even if the x-ray doesn’t show that subtle depression of the tibial plateau, the patient should be protective weight bearing: a walker with touch weight bearing in the older person or a knee immobilizer in a younger person and very close ortho follow up, or, if you have the option, go straight to CT. And if you see a depressed tibial plateau fracture of more than a 2mm or a split displaced fracture refer directly to ortho in the ED, as these patients will usually require urgent surgery.
Extensor Mechanism Injuries, The Straight Leg Raise and The Real Indications for Knee Ultrasound and Knee Immobilizers
Quadriceps tendon ruptures are more commonly seen in patients older than 40 years of age while the less frequent patella tendon ruptures are more commonly seen in patients under the age of 40.
Quadriceps tendon rupture is often misdiagnosed as a simple “knee sprain” and missed in up to 50% of patients. It is important to pick these injuries up in the ED because surgery is required within a week or two to prevent retraction of the muscle.
The triad of 1) acute knee pain with difficulty weight bearing, 2) inability to actively straight leg raise and 3) a suprapatellar gap or infrapatellar gap suggest the diagnoses of quadriceps or patella tendon rupture respectively.
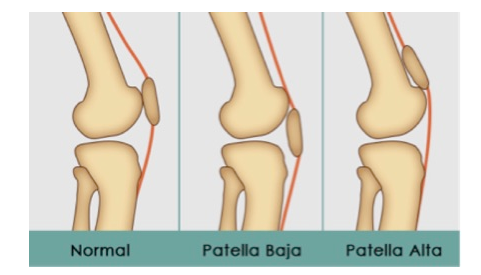
Often patients with quadraceps or patella tendon rupture will have normal x-rays. With a quadriceps tendon rupture, you may see Patella Baja (patella rides lower than usual). In a patellar tendon rupture, you may see Patella Alta (patella rides higher than usual – think alta for high altitude).
Pearl: An easy way to determine patella baja or patella alta is that the patella is normally one finger breadth above the joint line and any deviation from this may indicate a patella baja or alta. The Insall-Salvati ratiois a more exact method to determine patella baja and alta
Indications for knee immobilizer (e.g. Zimmer splint) in soft tissue injuries of the knee
The indications for a knee immobilizer are for extensor mechanism injuries
- First time patella dislocation
- Quadriceps tendon rupture
- Patella tendon rupture
These patients should be placed into a knee immobilizer and followed up with orthopedics because a complete tear usually requires surgery within one week to prevent retraction of the quadriceps.
Knee immobilizers are not indicated for suspected meniscus or ligament injuries of the knee as they do not aid in healing, may increase the rate of falls in older patients and cause atrophy of the quadraceps as well as stiffness leading to decreased range of motion.
Occult Knee Injuries: ACL Tear
The diagnosis of ACL tear is usually made on history alone, while the physical exam in the ED is usually non-contributory as the patient often can’t tolerate provocative testing. A good knee exam should be performed nonetheless to assess for the possibility of occult knee dislocation and other injuries.
History: Most ACL tears occur in the setting of sports without contact of another player and the the patient usually needs to be carried off the court or field. The ACL tears when there is sudden deceleration, the knee twists with the tibia pushed anteriorly usually with concurrent valgus stress. 70% of patients report a ‘pop’ and some report buckling or “giving out”. Significant swelling usually occurs within hours (as 0pposed to meniscus injury which is usually delayed).
Physical: Practically speaking the Lachman test is the only useful physical exam maneuver for assessment of ACL as the anterior drawer and pivot shift cause too much pain in the acute phase for that patient to be able to tolerate them.
What to look for on x-ray in a patient with suspected ACL tear
In pediatric patients with suspected ACL tear, look for tibial spine fracture on both AP and lateral x-ray which will change management in that these patient require immobilization in extension.
[See Tibial Spine Fracture With Anterior Cruciate Ligament Avulsion: Type 4 from Radiopedia.]
In adult patients with suspected ACL tear, look for a Segond fracture at the lateral tibial which will confirm the diagnosis but not change management.
[See The Excellent Article on Segond Fracture and images from Radiopedia.]
Management of suspected ACL tear
Avoid knee immobilizers!
Weight bearing as tolerated with early ROM exercises.
Trick of the trade: cut out a circle the size of the patient’s patella from an ABD pad and place the remaining ABD pad over the patient’s knee with a tensor bandage to hold it in place for improved compression of the knee.
The R in RICE stands for Restricted Activity, not Rest
For ACL, MCL and meniscus injuries instruct the patient to let pain be their guide, weight bear as tolerated with early ROM exercises to avoid knee stiffness and delay to normal activity.
How to differentiate a spontaneously reduced patella dislocation from an ACL injury
Patients with a spontaneously reduced patella dislocation will often have a history of anterior knee pain.
Usually the medial patello-femoral ligament ruptures and you will usually find tenderness in this area.
Apprehension test for spontaneously reduced patella dislocation: With the patient’s knee flexed at 20 degrees, grasp the patella and start to move it laterally. If the patient is very apprehensive when you do this, they have a positive apprehension test supporting the diagnosis of patella dislocation.
For suspected patella dislocation, order a patella skyline view and look for osteochondral fragments under the patella.
[See Sliver Sign (Patella) from Radiopedia. See article Lateral Patellar Dislocation from Radiopedia.]
Imaging of acute knee trauma is well covered in the Appropriateness Criteria For Acute Trauma To The Knee [PDF] from the American College of Radiology. What follows is from this reference:
What follows is from my post, More on Acute Knee Injuries from Evidence-Based Orthopedics Posted on January 19, 2012 by Tom Wade MD:
In the chapter “Initial Management of the Sports Injured Knee”*, the authors consider five questions regarding acute knee injury:
1. “What is the relative frequency of various injuries when patients present with a knee hemarthrosis?”
2. “What is the effectiveness of physical examination in diagnosing an ACL rupture in an acutely injured knee?”
3. “What is the role of MRI vs. arthroscopy in the diagnosis of acute knee injury?”
4. “What is the role for aspiration in the acutely injured knee with hemarthrosis?”
5. “Is there evidence in favor of surgical reconstruction of an acute (<3 weeks) ACL injury?”For the first question, “What is the relative frequency of various injuries when patients present with a knee hemarthrosis?”, the search strategy was as follows:
They queried the Cochrane database with the search term “knee injury”. They queried PubMed clinical queries search/systemic reviews with the search term “knee injury” AND “hemarthrosis”. They performed a PubMed sensitivity search using key words “knee injury AND hemarthrosis and arthroscopy OR MRI”. The exclusion search terms were “<16 years old, atruamatic injury, road traffic accidents”.
Using the above search strategy they found 13 prospective studies using arthroscopy or MRI and one retrospective study.
They pooled 12 of the studies and found that 57.5% had anterior cruciate injuries, 3.75% posterior cruciate injury, 32.5% meniscus injury, 13% osteocondral damage, and 18.8% had medial collateral injury.
They were unable to state what percentage of hemarthrosis were due to patellar dislocation because most of the studies did not report that. However, they cited a review in which patellar dislocation was said to be diagnosed in 4 to 23% of cases with hemarthrosis.
Their search strategies for the other four questions are detailed in in the book inChapter 93, pp 796-802*.
For question two, they state that Lachman test is most sensitive test for an acute ACL rupture and the pivot shift test is the most specific.
For question three, they conclude based on their search results, that early MRI rather than arthroscopy should be the next test if the physical examination is equivocal.
For question four, they conclude that there is no evidence for or against aspiration “for symptomatic relief or functional improvement in the acutely injured knee with hemarthrosis.”
And finally the fifth question is, “Is there evidence in favor of surgical reconstruction of an acute (<3 weeks) ACL injury?”
Their literature search on the fifth question leads them to conclude that “There is no difference in surgeon and patient-based outcomes when comparing early and delayed ACL reconstruction. Early structured rehabilitation and delayed optional reconstruction for the symptomatic patient is recommended for the acutely injured patient as opposed to routine early reconstruction.”
*Evidence-Based Orthopedics, First Edition. Edited by Mohit Bhandari.
© 2012 Blackwell Publishing Ltd. Published 2012 by Blackwell Publishing Ltd.
Resources:
(1) Episode 91 Occult Knee Injuries Pearls and Pitfalls [Link is to the podcast and show notes] Written Summary and blog post by Dr Anton Helman January, 2017
(2) Appropriateness Criteria For Acute Trauma To The Knee [PDF] from the American College of Radiology.
(3) More on Acute Knee Injuries from Evidence-Based Orthopedics Posted on January 19, 2012 by Tom Wade MD.