Reference (1), Evaluation and Treatment of Functional Constipation in
Infants and Children, is a good resource to start with.
When you’re thinking about diagnosing constipation as the cause of an infant or child’s abdominal pain, the key is to make sure that the abdominal pain is due to something much more serious (chart on p 264):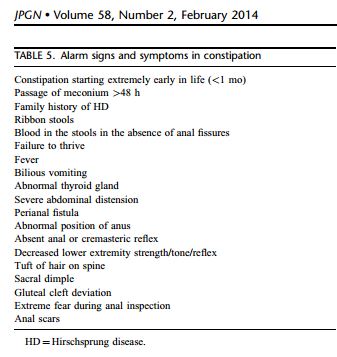
Reference (1), Evaluation and Treatment of Functional Constipation in
Infants and Children, also contains the following excellent charts:
There are two excellent flow charts for evaluation on pages 260 and 261. Both algorithms (< 6 mo and >/= 6 mo) are for children presenting with constipation of at least two weeks duration.
Table 3 on p 263 has the differential diagnosis of pediatric constipation.
Table 4 on p 264 has “Key points of history and physical examination to guide in the evaluation of constipation in infants/toddlers and children/adolescents.”
______________________________________________________________
The source of the all the information below is Dr Anton Helman‘s outstanding Emergency Medicine Cases podcast Episode 19 Part 2: Pediatric Gastroenteritis, Constipation and Bowel Obstruction Reference (1):
Constipation is a common discharge diagnosis in the emergency department for pediatric abdominal pain.
And in many cases this is a chronic problem with an acute exacerbtion.
However, acute pediatric abdominal pain can be caused by other more serious problems masquerading as simple constipation.
- The first thing to consider carefully is: Is this an acute problem in a patient who happens to have chronic constipation? Like appendicitis [unexplained tachycardia or an unexplained tachypnea, or is it toxic megacolon in a patient who appears septic with abdominal pain [a lateral decubitus, left side down might reveal this (and also could be due to bowel obstruction or pneumoperitonium – which might also show up on the lateral decub).
- Hirschsprung’s Disease
- Missed cystic fibrosis
- Next, consider Hirschsprung’s Disease.
- Consider a dietary change, for example, from breast milk to bottle feeding.
- Is It Celiac Disease?
- High fever – Remeber that typhoid fever can present as constipation [and with international travel so common, it could occur anywhere]
- Does the child really meet the Rome criteria for chronic constipation?
- Is the patient short or have coarse features? Missed congenital or newly developed hypothyroidism.
- Does the patient have Down’s syndrome or another cause of muscle weakness. Dr Jarvis says: I have seen constipation as the first sign of muscle weakness. [botulism, for example?]
- Does the patient have an occult cord problem? Was the patient late in walking?
- [Has the child fallen off his/her growth chart curves indicating the development of a chronic problem]
So look carefully at the child and do a complete head to toe exam.
Resources:
(1) Evaluation and treatment of functional constipation in infants and children: evidence-based recommendations from ESPGHAN and NASPGHAN [PubMed Abstract] [Full Text PDF]. J Pediatr Gastroenterol Nutr. 2014 Feb;58(2):258-74. doi: 10.1097/MPG.0000000000000266.
(2) Episode 19 Part 2: Pediatric Gastroenteritis, Constipation and Bowel Obstruction podcast from Emergency Medicine Cases.
(3) Constipation as cause of acute abdominal pain in children [PubMed Abstract]. J Pediatr. 2007 Dec;151(6):666-9. Epub 2007 Jul 30.




