In this post, I link to and excerpt the section on Cauda Equina Sydrome from Dr. Josh Farkas‘s outstanding Internet Book of Critical Care‘s [Link is to the TOC] chapter Spinal Cord, May 14, 2022.
All that follows is from the above chapter.
cauda equina syndrome
basics
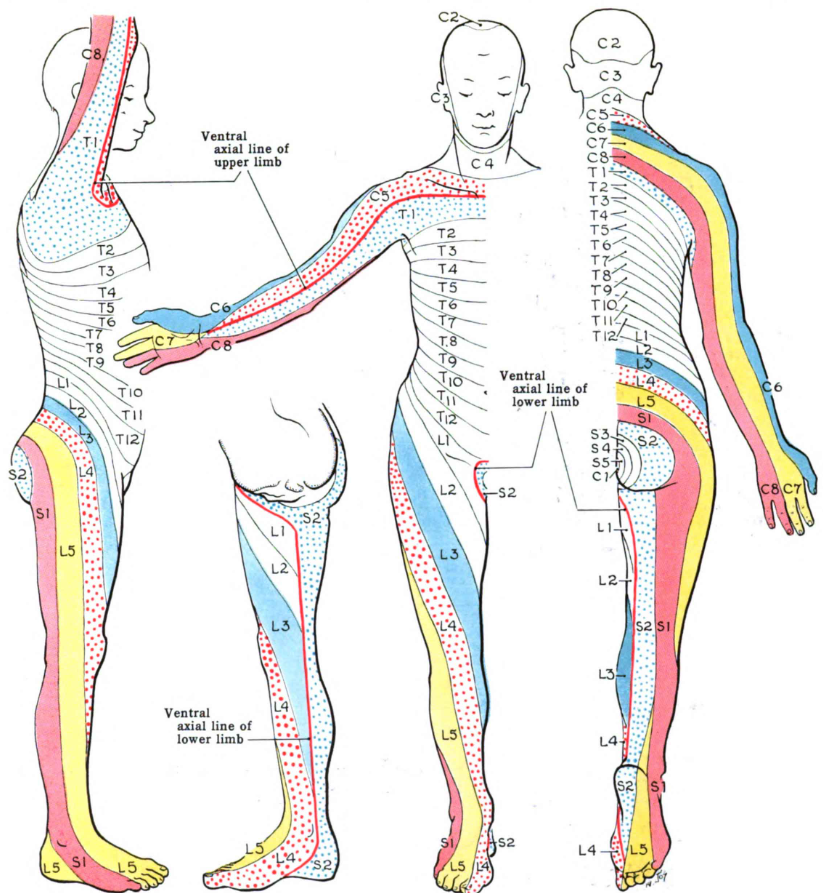
- The cauda equina is composed of nerve roots L2-L5 and S1-S5, which exit the spinal cord below the end of the spinal cord (figure below). Functions of these nerves include the following:(33522743)
- L2-S3: Leg movement and sensation.
- S2-S4: Genitalia sensation, bladder function, external anal sphincter.
- S4-S5: Sensation overlying the coccyx.
- Cauda equina syndrome lacks a precise definition. It is generally used to refer to pathologies which damage several of these nerve roots.
more common causes (33522743)
- Structural spinal disease:
- Lumbar disc herniation (~45% of cases).
- Spinal stenosis, ankylosing spondylitis.
- Trauma.
- Vascular:
- Spinal epidural hematoma.
- Dural arteriovenous fistula.
- Aortic disease causing ischemia (e.g., dissection, thrombosed aneurysm).
- Thrombosis/occlusion of the inferior vena cava causing enlargement of the epidural venous plexus.
- Neoplasm:
- Primary or metastatic tumor, including leptomeningeal carcinomatosis.
- Radiation-induced.
- Intrathecal methotrexate or cytarabine.
- Infection:
- Other rare causes:
- Sarcoidosis.
- Extramedullary hematopoiesis.
possible symptoms
- Back pain and leg pain, especially bilateral sciatica radiating down both legs.(31471075) This is the most common presenting symptom.(31471075)
- Urinary dysfunction may be the most reliably reported autonomic symptom, allowing it to help grade the severity of injury:(33522743; 31471075)
- Complete cauda equina dysfunction causes painless urinary retention and overflow incontinence.
- Incomplete cauda equina dysfunction may cause altered urinary sensation, poor urinary stream, or the need to strain during urination.
- Sensory loss may be unilateral or bilateral, most often involving the posterior thighs, buttocks, and perineum.(33522743)
- Leg weakness.
- Other signs of autonomic dysfunction:
- Sexual dysfunction (e.g., dyspareunia, impotence, priapism, urination during intercourse).(33522743)
- Bowel retention or incontinence.
constellation of symptoms
- Individual patients may have variable symptoms, due to involvement of different nerves.
- Disease course may vary in acuity, depending on the cause (e.g., gradually enlarging neoplasm vs. acute disc herniation).
examination findings
- Reduced/absent reflexes and weakness may be seen in the legs. However, cauda equina syndrome involving only the lower nerve roots (e.g., S2-S5) may spare leg strength. The following should be carefully evaluated:
- Hip flexion (L2).
- Knee extension (L3).
- Foot dorsiflexion (L4) and plantar flexion (S1).
- Great toe dorsiflexion (L5).
- Patellar and Achilles tendon reflexes.
- Loss of sensation in the legs or perineum.
- Post-void residual volume in the bladder >200 ml was reported to be 94% sensitive and 72% specific in one prospective study.(31479434)
Rectal tone is not useful, since assessments are subjective and inaccurate.(33522743, 31471075) However, a careful evaluation of skin sensation to pinprick in the perirectal area should be performed (including sensation on both sides of the anus). Unilateral or bilateral perianal numbness has a higher sensitivity and specificity than rectal tone.(31479434)
imaging
- Lumbar spine MRI with contrast is the test of choice. If this is negative, imaging of the cervical and thoracic cord should be considered (to look for a central cord syndrome at a higher level that may be masquerading as cauda equina syndrome).
- CT scan with contrast may detect bony abnormalities of the spinal canal (e.g., spinal stenosis), but is less sensitive for soft tissue disorders. CT myelogram has higher performance, but it is more invasive and may be more difficult to obtain.
lumbar puncture
- Lumbar puncture is initially contraindicated, since this could exacerbate a spinal epidural abscess or epidural hematoma.
- After performing an MRI, if the etiology remains unclear then lumbar puncture may help evaluate for leptomeningeal carcinomatosis or infection.
differential diagnoses may include:
- Spinal cord lesion in the conus medullaris (more on this below; overall significance is similar to cauda equina syndrome).
- Spinal cord lesion in the cervical or thoracic cord (especially a central cord lesion).
- Guillain-Barre syndrome (GBS).
conus medullaris syndrome
- Conus medullaris syndrome refers to pathology at the very end of the spinal cord (usually at the T12-L1 level). This is difficult to distinguish from cauda equina syndrome, but the difference often isn’t important – the clinical significance of both syndromes is similar.(Alpert 2019)
- Some differences compared to cauda equina syndrome:
- Weakness may be spastic (rather than flaccid).
- If sensory loss is dissociated (e.g., with loss of pain/temperature, put preservation of touch/vibration/proprioception), this suggests a lesion in the conus medullaris of the spinal cord.(27907952)