Causes and Evaluation of Chronic Dyspnea, 2012 is an outstanding article.
The following are excerpts from Causes and Evaluation of Chronic Dyspnea, 2012, from the American Family Physician:
Abstract
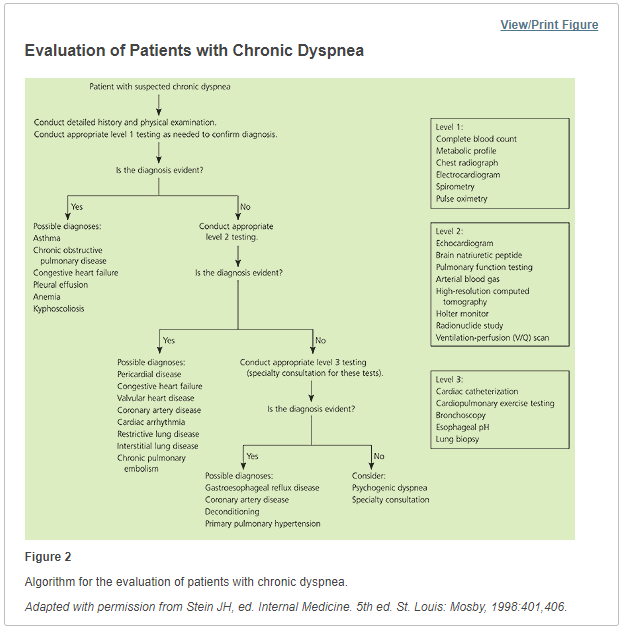
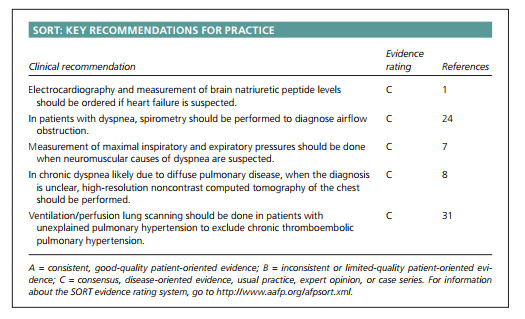
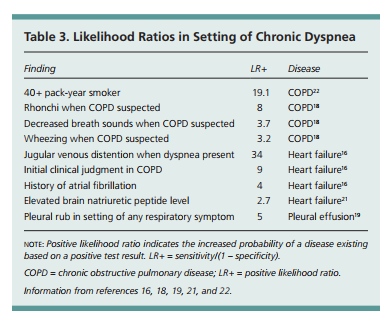
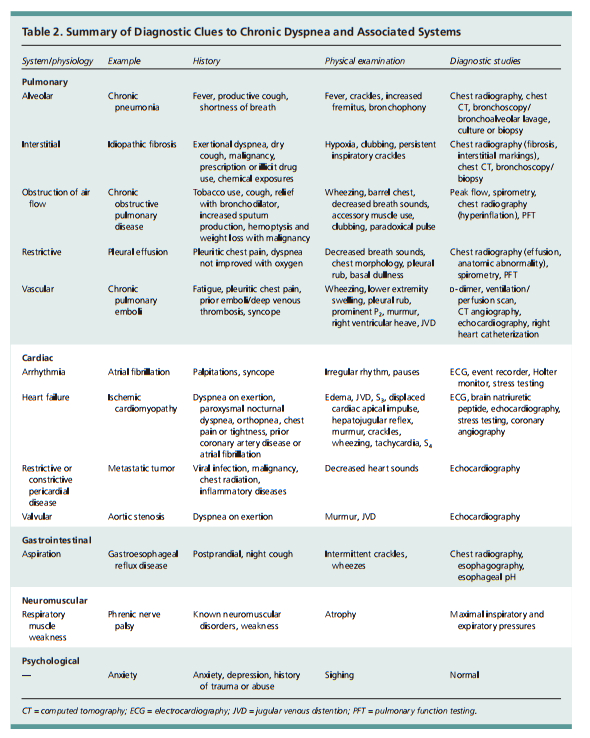
Chronic dyspnea is shortness of breath that lasts more than one month. The perception of dyspnea varies based on behavioral and physiologic responses. Dyspnea that is greater than expected with the degree of exertion is a symptom of disease. Most cases of dyspnea result from asthma, heart failure and myocardial ischemia, chronic obstructive pulmonary disease, interstitial lung disease, pneumonia, or psychogenic disorders. The etiology of dyspnea is multifactorial in about one-third of patients. The clinical presentation alone is adequate to make a diagnosis in 66 percent of patients with dyspnea. Patients’ descriptions of the sensation of dyspnea may be helpful, but associated symptoms and risk factors, such as smoking, chemical exposures, and medication use, should also be considered. Examination findings (e.g., jugular venous distention, decreased breath sounds or wheezing, pleural rub, clubbing) may be helpful in making the diagnosis. Initial testing in patients with chronic dyspnea includes chest radiography, electrocardiography, spirometry, complete blood count, and basic metabolic panel. Measurement of brain natriuretic peptide levels may help exclude heart failure, and D-dimer testing may help rule out pulmonary emboli. Pulmonary function studies can be used to identify emphysema and interstitial lung diseases. Computed tomography of the chest is the most appropriate imaging study for diagnosing suspected pulmonary causes of chronic dyspnea. To diagnose pulmonary arterial hypertension or certain interstitial lung diseases, right heart catheterization or bronchoscopy may be needed.
Causes of Dyspnea
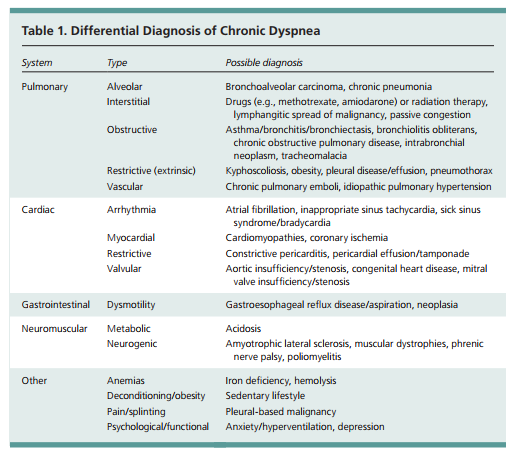
Dyspnea may be of neurogenic, respiratory,
or cardiac origin, and may be associated with
conditions such as anemia, deconditioning,
or anxiety.6 The differential diagnosis of dyspnea has been presented in various ways.1,3 Table 1 lists the differential diagnosis of chronic dyspnea by organ system.Asthma, congestive heart failure and myocardial ischemia, COPD, interstitial lung disease, pneumonia, and psychogenic disorders account for approximately 85 percent of all
cases of shortness of breath.7 Cardiac and pulmonary etiologies predominate. The etiology of chronic dyspnea is multifactorial in up toone-third of patients.8
COMPREHENSIVE PULMONARY FUNCTION TESTS
Pulmonary function tests include blood gas evaluation, lung volume measurement (i.e., residual volume, functional residual capacity, and total lung capacity) and carbon monoxide diffusion in the lung (DLCO), in addition to spirometry. Total lung capacity is reduced in persons with parenchymal restrictive disease, but is normal or increased in those who have obstructive disorders with air trapping.1 In a patient who has normal spirometry and lung volumes but a reduced DLCO, the differential diagnosis includes anemia, early interstitial lung disease, and pulmonary vascular disease. Patients with emphysema typically have low DLCO. In patients with bronchiectasis, dyspnea is more closely correlated with lung hyperinflation than with airflow obstruction parameters.29
Resources:
(1) Causes and Evaluation of Chronic Dyspnea [PubMed Abstract] [Full Text PDF]. Am Fam Physician. 2012 Jul 15;86(2):173-82.