There are a number of guidelines for the diagnosis and treatment of sinusitis.
In this post I am reviewing and excerpting from the Clinical Practice Guideline (Update): Adult Sinusitis [Full Text HTML] [Full Text PDF] 2015 from American Academy of Otolaryngology-Head and Neck Surgery Foundation (AAO-HNSF):
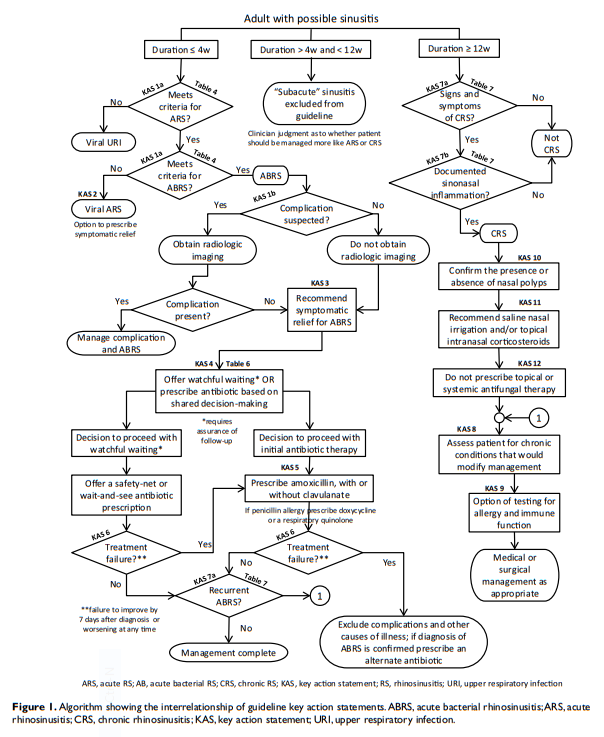
Action statements.
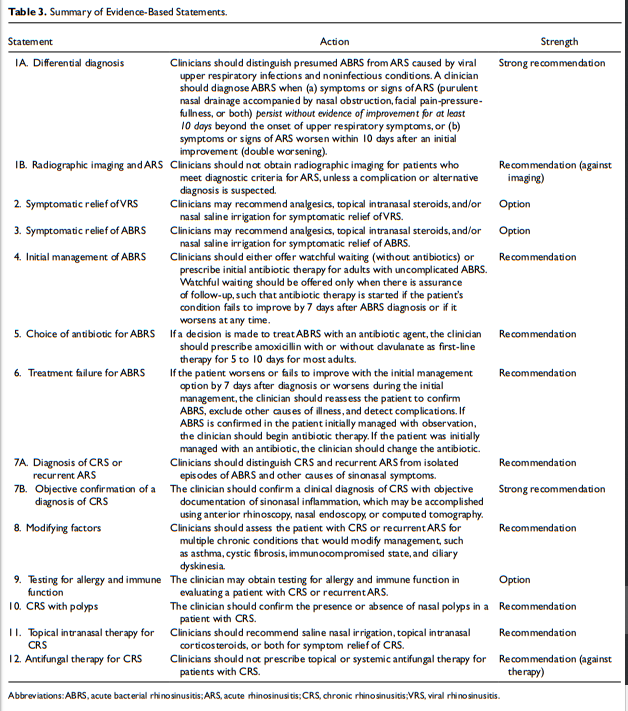
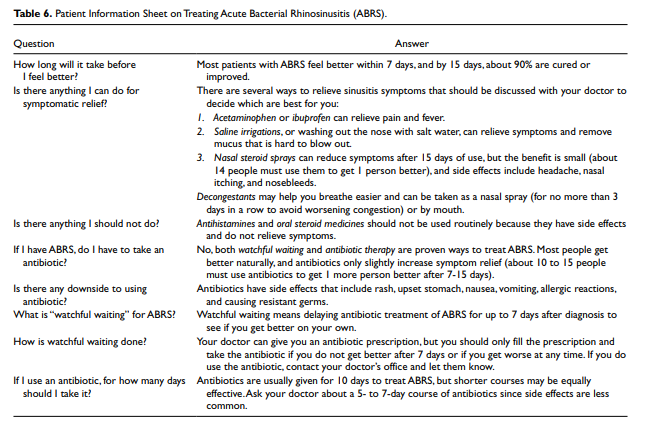
The update group made strong recommendations that clinicians (1) should distinguish presumed ABRS from acute rhinosinusitis (ARS) caused by viral upper respiratory infections and noninfectious conditions and (2) should confirm a clinical diagnosis of CRS with objective documentation of sinonasal inflammation, which may be accomplished using anterior rhinoscopy, nasal endoscopy, or computed tomography. The update group made recommendations that clinicians (1) should either offer watchful waiting (without antibiotics) or prescribe initial antibiotic therapy for adults with uncomplicated ABRS; (2) should prescribe amoxicillin with or without clavulanate as first-line therapy for 5 to 10 days (if a decision is made to treat ABRS with an antibiotic); (3) should reassess the patient to
onfirm ABRS, exclude other causes of illness, and detect complications if the patient worsens or fails to improve with the
initial management option by 7 days after diagnosis or worsens
during the initial management; (4) should distinguish CRS and recurrent ARS from isolated episodes of ABRS and other causes of sinonasal symptoms; (5) should assess the patient with CRS or recurrent ARS for multiple chronic conditions that would modify management, such as asthma, cystic fibrosis, immunocompromised state, and ciliary dyskinesia; (6) should confirm the presence or absence of nasal polyps in a patient
with CRS; and (7) should recommend saline nasal irrigation,
topical intranasal corticosteroids, or both for symptom relief of
CRS. The update group stated as options that clinicians may (1)
recommend analgesics, topical intranasal steroids, and/or nasal
saline irrigation for symptomatic relief of viral rhinosinusitis; (2) recommend analgesics, topical intranasal steroids, and/or nasal saline irrigation) for symptomatic relief of ABRS; and (3) obtain testing for allergy and immune function in evaluating a patient with CRS or recurrent ARS. The update group made recommendations that clinicians (1) should not obtain radiographic imaging for patients who meet diagnostic criteria for ARS, unless a complication or alternative diagnosis is suspected, and (2) should not prescribe topical or systemic antifungal therapy for patients with CRS.The Burden Of Rhinosinusitis
Twelve percent of the US population (nearly 1 in 8 adults)
reported being diagnosed with rhinosinusitis in the prior 12
months in a 2012 national health survey.4 Rhinosinusitis was diagnosed more frequently than hay fever (7%), bronchitis
(4%), or chronic obstructive pulmonary disease (4%), and the
individuals surveyed were almost as likely to receive a diagnosis
of rhinosinusitis as they were of asthma (13%).The broad category of rhinosinusitis in the preceding paragraph
includes ARS and CRS. Most ARS begins when a viral upper respiratory infection (URI) extends into the paranasal
sinuses, which may be followed by bacterial infection. About
20 million cases of presumed bacterial ARS (ABRS) occur
annually in the United States,5 rendering it one of the most common conditions encountered by clinicians. The importance of ABRS relates not only to prevalence but also to the potential for uncommon, but serious, complications that include meningitis, brain abscess, orbital cellulitis, and orbital abscess.17,18National ambulatory care data from 2006 to 2010 revealed
that rhinosinusitis accounted for more outpatient antibiotic prescriptions than any other diagnosis. Despite guidelines that encourage judicious antibiotic use for ARS,16,19 they are prescribed in about 82% of visits.20 From 2006 to 2010, rhinosinusitis accounted for 11% of all primary care antibiotic-related visits, with ARS accounting for 3.9% and CRS accounting for 7.1%.20 ARS and CRS combined accounted for more primary ambulatory care visits with antibiotic prescriptions than any other diagnosis or commonly grouped diagnoses.Cardinal Symptoms of Acute Rhinosinusitis
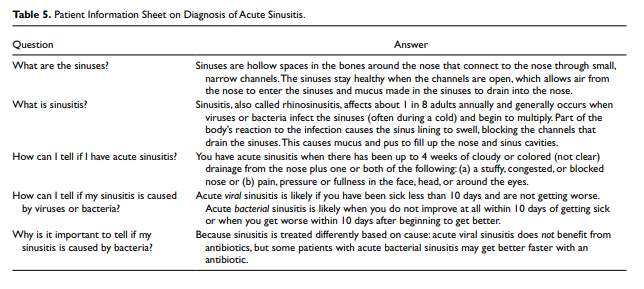
Acute rhinosinusitis is diagnosed when a patient presents with
up to 4 weeks of purulent (not clear) nasal drainage accompanied by nasal obstruction, facial pain-pressure-fullness, or both (Table 4). Nasal obstruction without purulent nasal drainage is not consistent with ARS and is beyond the scope of this guideline. Similarly, facial pain without purulent nasal drainage is not consistent with ARS, even though many patients present with a history of self-reported or physician-diagnosed “sinus” headache, which is often related to migraines and is responsive to migraine therapy.45,4When a patient meets the criteria for ARS in Table 4, the clinician should distinguish between viral rhinosinusitis (VRS) and presumed ABRS.5,13,47,48 This distinction is based on illness pattern and duration (Table 4), because purulent nasal drainage as a sole criterion cannot distinguish between viral and bacterial infection.49 Although there is no high-level evidence showing that symptom duration and purulent discharge can reliably distinguish presumed bacterial vs viral ARS,50 the GUG considered the criteria in Table 4 to be best for this purpose based on first principles, subsidiary evidence, and expert consensus, as explained in the remainder of this section.
The rationale for selecting 3 cardinal symptoms is based on
their high sensitivity and their relatively high specificity for
ABRS, especially when considering the time interval of persistence for 10 days or longer.51-53 Purulent (infected, colored, or oozing) nasal drainage predicts presence of bacteria on antral aspiration when reported as purulent rhinorrhea by the patient, when manifest as postnasal drip or purulent discharge in the posterior pharynx, or when observed in the nasal cavity or near the sinus ostium.54,55 Purulent rhinorrhea also predicts radiographic evidence of ABRS.56,57 Facial or dental pain also predicts ABRS,53,55 but the location correlates poorly with the specific sinuses involved.58 Last, patient complaints of nasal obstruction correlate with objective measures, such as rhinomanometry or nasal peak flow rate.59Transition from Viral to Bacterial Infection
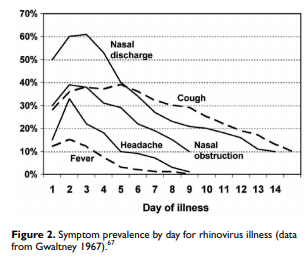
Although ABRS is often considered a transition from a preceding viral URI,51 bacterial infection can develop at any time during the course of the illness. The concept of a transition, however, is useful for management decisions,53 especially when considering the time course of VRS and which disease patterns are most likely to be associated with bacterial infection. Although ABRS is often considered a transition from a preceding viral URI,51 bacterial infection can develop at any time during the course of the illness. The concept of a transition, however, is useful for management decisions,53 especially when considering the time course of VRS and which disease patterns are most likely to be associated with bacterial infection.
In the first 3 to 4 days of illness VRS cannot be differentiated
from an early-onset ABRS; therefore, only patients with
unusually severe presentations or extra-sinus manifestations
of infection are presumed to have a bacterial illness.Fever is present in some patients with VRS in the first few days of illness (Figure 2) but does not predict bacterial infection as an isolated diagnostic criterion. Fever has a sensitivity and specificity of only about 50% for ABRS,52,53 and a systematic review concluded that evidence was lacking regarding the ability of fever and facial/dental pain to distinguish ABRS from VRS.68 For this reason, we did not include fever as a cardinal sign/symptom in diagnosing ABRS.
Although our GUG concluded that evidence was insufficient to support a “severe” presentation of ABRS, others have explicitly highlighted this subgroup of patients with ABRS. Meltzer and coworkers13 defined a special circumstance of ABRS when purulent nasal discharge for 3 to 4 days was accompanied by high fever. “High fever” was not defined, but the criterion only applied to severe disease with a shorter duration of illness.
A guideline on sinusitis in children from the American Academy of Pediatrics 69 considered 3 or more days of concurrent high fever and purulent nasal discharge as a “severe” presentation of ABRS that warrants antibiotic therapy.
Similarly, the Infectious Disease Society of America
guideline on ABRS15 recommended that the clinician consider
a diagnosis of ABRS if the patient presented with severe symptoms at the onset or has high fever (>39°C or 102°F) and
purulent discharge or facial pain lasting at least 3 to 4 consecutive days at the beginning of illness.STATEMENT 1B. RADIOGRAPHIC IMAGING AND ACUTE RHINOSINUSITIS:
Clinicians should not obtain radiographic imaging for patients who meet diagnostic criteria for acute rhinosinusitis, unless a complication or alternative diagnosis is suspected. Recommendation (against imaging) based on diagnostic studies with minor limitations and a preponderance of benefit over harm for not obtaining imaging.
[Imaging Of The Sinuses When Complications Are Suspected]
When a complication of ABRS or an alternative diagnosis
is suspected, imaging studies may be obtained.33 Complications
of ABRS include orbital, intracranial, or soft tissue involvement. Alternative diagnoses include malignancy and other noninfectious causes of facial pain. Radiographic imaging may also be obtained when the patient has modifying factors or comorbidities that predispose to complications, including diabetes, immune-compromised state, or a history of facial trauma or surgery.CT imaging of the sinuses is appropriate when a complication of ABRS is suspected based on severe headache, facial swelling, cranial nerve palsies, or forward displacement or bulging of the eye (proptosis); CT findings that correlate with ABRS include opacification, air-fluid level, and moderate to severe mucosal thickening. Complications of ABRS are best assessed using iodine contrast-enhanced CT or gadolinium based MR imaging to identify extra-sinus extension or involvement.33,75-77 Suspected complications are the only indication for MR imaging of the paranasal sinuses in the setting of ABRS.
Limitations of CT imaging include increased cost and radiation
dosage. Radiation dose is related to technique and, if appropriate technique is not used, may deliver over 10 times
the dosage compared with plain film radiography. With careful
choice of technical factors, however, CT dosage can be lowered to 2 times the dose of plain film radiography. Other limitations of CT include lack of specificity for bacterial infection, a relative lack of correlation between localizing symptoms and sinus disease on CT, and the high frequency of incidental abnormal findings in asymptomatic persons.74,78-80An alternative to traditional CT imaging is in-office conebeam
CT scanning, which offers advantages of point-of-care testing and possible decreased radiation dosage. The indications for office-based CT imaging are the same as for traditional scanners, and they should not be used for diagnosing or managing uncomplicated ABRS.[Oral Steroids]
A Cochrane review96 of systemic steroids for ABRS found no benefit over placebo when oral steroids were used as monotherapy. Limited data from 5 trials were found to suggest
that oral steroids used in combination with antibiotics may
have a modest short-term beneficial effect for symptom relief
(number needed to treat of 7), but confidence in results was
limited by a significant risk of attrition bias caused by missing
outcomes. Adverse events were mild (nausea, vomiting, gastric
complaints), but the authors conclude that additional research is needed for adequate confidence in the true effect of systemic steroids.
Resources:
(1) Clinical Practice Guideline (Update): Adult Sinusitis [PubMed Abstract] [Full Text HTML] [Full Text PDF] 2015 from American Academy of Otolaryngology-Head and Neck Surgery Foundation (AAO-HNSF)
The above article has been cited in 62 PubMed Central Articles.
(2) Diagnosis of acute rhinosinusitis in primary care: a systematic review of test accuracy [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Br J Gen Pract. 2016 Sep;66(650):e612-32. doi: 10.3399/bjgp16X686581. Epub 2016 Aug 1.
(3) Necessity of office visits for acute respiratory infections in primary care [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Fam Pract. 2016 Jun;33(3):312-7. doi: 10.1093/fampra/cmw019. Epub 2016 Apr 5.
(4) Is Rinsing Your Sinuses With Neti Pots Safe? from The U.S. Food And Drug Administration.