Many people eat 200 to 300 grams of carbohydrate a day (and even more sometimes).
So when a patient begins a ketogenic diet for diabetes management his or her carbohydrate intake will be less than 20 grams of carbohydrate.
The key to safely initiating and monitoring the ketogenic diet is the prevention of hypoglycemia by closely following the patient’s glucose levels and by adjusting the patient’s diabetes medicines from day one.
And I recommend that patients use a continuous glucose monitor starting on day one of their ketogenic diet. At the start of the diet, the doctor and patient should be reviewing the blood sugars and diabetic medication dosages on a daily or almost daily basis to avoid hypoglycemia.
Here is a link to The First Four Glucose Monitors, July 4, 2018, from Managed Care Magazine. The continous glucose monitor is one of the keys to safely and successfully initiating and following a ketogenic diet.
The ketogenic diet causes a very large decrease in carbohydrate intake that requires immediate (on the day of ketogenic diet initation) changes in the the patient’s diabetes medicines. The article below details the medication changes that need to be made.
Changes in the diabetic medication will continue to be required through out the patient’s ketogenic diet.
Because blood pressure can decrease with the ketogenic diet, the patient and physician must follow the patient’s blood pressure.
And because a ketogenic diet causes diuresis, following serum sodium and serum potassium initially and at regular intervals is, I believe, prudent.
See Resources (3) and (4) below for a great brief review of these potential pitfalls.
(3) Hyponatremia in Emergency Medicine Clinical Presentation
Updated: Dec 28, 2018 by Kartik Shah, MD from emedicine.medscape.com
(4) Hypokalemia
Updated: Dec 06, 2018 by Eleanor Lederer, MD, FASN from emedicine.medscape.com
For a great lecture on the use of the ketogenic diet for diabetics to improve glycemic control and to lose weight, please see “Ketogenic Diet for Diabetes with Sarah Hallberg, DO” With Additional Resources
Posted on November 4, 2019 by Tom Wade MD
Resources For This Post:
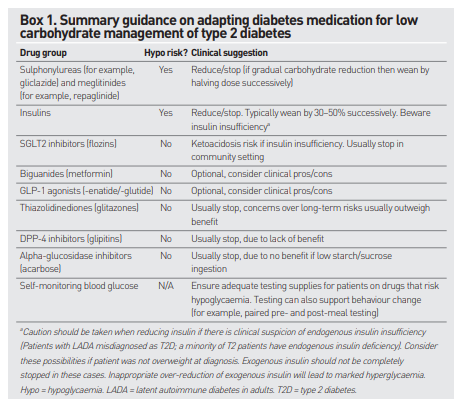
(1) Adapting diabetes medication for low carbohydrate management of type 2 diabetes: a practical guide [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Br J Gen Pract. 2019 Jul;69(684):360-361. doi: 10.3399/bjgp19X704525.
Here are excerpts from the above article:
DIABETES MEDICATIONS AND AN LCD (Low Carbohydrate Diet)
Blood glucose levels typically fall substantially when an individual adopts an LCD. This article discusses key considerations regarding hypoglycaemic medications for an LCD and provides practical suggestions to prescribers.
MEDICATIONS THAT CREATE A RISK OF
HYPOGLYCAEMIASulphonylureas and meglitinides
Sulphonylureas (for example, gliclazide) and meglitinides (for example, repaglinide) should be reduced or stopped when an LCD is commenced. An initial dosage reduction of at least 50% is typically appropriate, with further reductions according to blood glucose response. There may be a period of short term hyperglycaemia while the individual adapts to an LCD.
Insulins
Practical expertise suggests a 50% reduction of daily insulin dose at initiation of the LCD is appropriate in most cases. In individuals whose HbA1c is markedly elevated, a smaller reduction of perhaps 30% may be appropriate, with further reductions over time.
For individuals on a basal-bolus regimen it is preferential to reduce or stop bolus insulin.
In individuals on a mixed insulin or basal insulin alone each dose can be reduced by 30–50% at the start of LCD.
Some patients can expect to come off insulin completely, over days or months, as insulin resistance resolves. Improving blood glucometer readings can guide the down-titration of insulin.
It should be cautioned that some patients may have an insulin insufficiency form of diabetes, such as latent autoimmune diabetes of adults (LADA). Although the LCD enables a reduction in insulin dosage it should not be completely stopped in this cohort of patients. Endogenous insulin insufficiency is more likely in patients who were not overweight at the time of diagnosis of diabetes, and it may be present in some with longstanding T2D. Overreduction in insulin dosage in these patients would lead to significant hyperglycaemia, and thus further dosage reduction would be avoided. It is recommended that additional investigation and expert advice is sought in cases of doubt as per good medical practice.
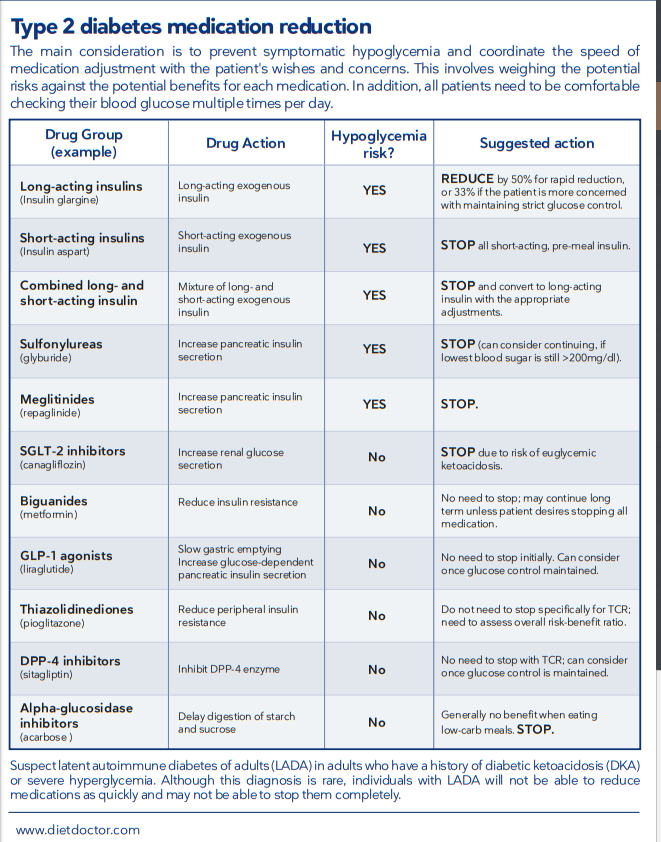
Resource (2) Adjusting medications on a low-carb diet, October 23, 2019 from Diet Doctor.
Here is the table from the above resource, summarizing diabetic medicine deprescribing while initiating and following the ketogenic diet.*
*Again, note that the deprescribing requires close monitoring, by both the patient and physician, of the changing blood sugars. These change can occur on day one of diet initiation. And the best way to follow these changes initially and through time is with the continuous blood sugar monitor.