The purpose of diagnosing transient ischemic attack is to hopefully prevent a stroke or coronary artery disease.
For links to the references and information on the prevention of stroke and coronary artery disease with patients diagnosed with transient ischemic attack, please see Resources below.
The following on transient ischemic attack is from Emergency Neurological Life Support Course: Acute Ischemic Stroke. [Pubmed Abstract] This module-protocol is available as a full text PDF as are all the other modules-protocols in the ENLS course at the same link.
TIA
The diagnosis of TIA is based on the new onset of focal neurological signs and symptoms that are explainable by a vascular disease (ie, arterial occlusion of a single or group of arteries adquately explain the patient’s signs and symptoms), and these signs and symptoms resolve within 24 h (most TIAs resolve in a much shorter period of time [typically lasting less than 20 minutes].
However, up to one-third of TIAs have demonstrable injury on MRI [6]. Although these cases are now classified as stroke, it is unlikely that emergency reperfusion therapy should be attempted. Approximately 50% of patients with a TIA will have CT findings of a prior cerebrovascular accident (CVA), even though the CVA may have been clinically silent.
ABCD2 Score
The ABCD2 score is an ordinal scale that provides risk prediction of subsequent stroke following a TIA. Table 6 demonstrates how to calculate this score.
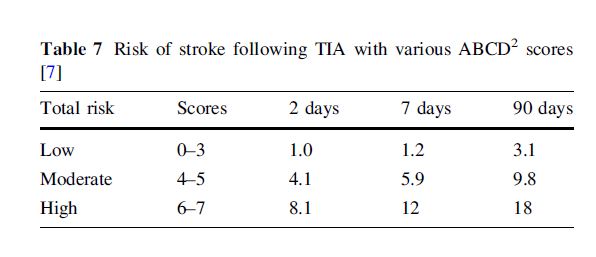
Add all of the points above for the total ABCD2 score (0-7). Table 7 lists the estimated risk (%) of a stroke occurring within various time ranges.
Table 7 Risk of stroke following TIA with various ABCD2 scores
Based on this risk stratification, some physicians choose to admit high-risk patients and discharge those at low risk. There is controversy regarding the admission of moderate risk, and this decision follows local practice.
Low Risk TIA
For low risk patients (ABCD2 scores 0-3), an outpatient workup in the 1-2 days following score calculation may be most appropriate. Alternatively, observation or admission may be an option. In either case, stroke can be prevented by the following regimen [8]:
- Begin an antithrombotic agent (ASA 325 mg, clopidogrel 75, or ASA/extended release dipyrimadole).
- Perform carotid imaging: ultrasound, CTA, or MRA
- Consider transthoracic echocardiography; if bilateral infarcts are present on CT or there is a high suspicion of cardiac embolic source, and the transhoracic echo is normal, obtain transesophageal echocardiography (TEE).
- Consider 30-day cardiac monitor to detect intermitent atrial fibrillation.
- Encourage smoking cessation.
- Initiate statin (atorvastatin 80 mg/day or equivalent).
If ECG or rhythm strip shows atrial fibrillation, consider starting anticoagulation (oral anticoagulant or low molecular weight heparin) or ASA, depending on CHADS2 score. In these cases, referral to a vascular neurologist or cardiologist is appropriate.
High Risk TIA
For patients with higher-risk TIAs (scores >3), hospital admission is advisable. Inaddition to the treatments discussed above, some physicians keep patients on bed rest for a day, with the head flat (in order to maintain brain perfusion). After 24 h, the patient should begin to get out of bed as tolerated with assistance. Permissive hypertension is encouraged (not to exceed 220/120 mmHg) and BP limits should be gradually lowered over 24–48 hours.
Resources:
Emergency neurological life support: acute ischemic stroke, [PubMed Abstract]. Neurocrit Care. 2012 Sep;17 Suppl 1:S29-36.
The Emergency Neurological Life Support Protocols, [Full Text PDFs]. Description:
Each protocol* is formatted into a hyperlinked pdf file for portability and can be viewed on most devices. The link to “All Protocols” is a single, large pdf file that has all ENLS protocols in a single file.
*Topics:
All Protocols
Acute Non-Traumatic Weakness
Acute Stroke
Airway and Ventilation and Sedation
Coma
Intracerebral Hemorrhage
Intracranial Hypertension and Herniation
Ischemic Stroke
Meningitis/Encephalitis
Resuscitation following Cardiac Arrest
Spinal Cord Compression
Status Epilepticus
Subarachnoid Hemorrhage
Traumatic Brain Injury
Traumatic Spine InjurySub-Topics:
Hunt Hess Classification of SAH
World Federation Neurological Scale
Glasgow Coma Scale
Guidelines for the Prevention of Stroke in Patients With Stroke and Transient Ischemic Attack, [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Stroke. 2014 Jul;45(7):2160-236. doi: 10.1161/STR.0000000000000024. Epub 2014 May 1.There was a correction to the article:
In the article by Kernan et al, “Guidelines for the Prevention of Stroke in Patients With Stroke and Transient Ischemic Attack: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association,” which published online May 1, 2014, and appeared in the July 2014 issue of the journal (Stroke. 2014;45:2160–2236), a correction was needed. On page 2173, second column, last paragraph, the second sentence read, “…and the dipeptidyl peptidase-4 inhibitor linagliptide.134” It now reads, “…and the dipeptidyl peptidase-4 inhibitor linagliptin.134” This correction has been made to the print version and to the current online version of the article, which is available at https://stroke.ahajournals.org/content/45/7/2160.
Definition and Evaluation of Transient Ischemic Attack, [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Stroke. 2009; 40: 2276-2293
Coronary Risk Evaluation in Patients With Transient Ischemic Attack and Ischemic Stroke, [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Circulation.
2003; 108: 1278-1290