Dr Kon- VA-ECMO for massive pulmonary embolism from the Maryland Critical Care Project:
Today we welcome Zachary Kon, M.D., Assistant Professor in the Department of Cardiothoracic Surgery at NYU. In addition to acting as the Surgical Director of Pulmonary Hypertension/Pulmonary Thromboendarterectomy Program, Dr. Kon also acts as the Surgical Director of the NYU Lung Transplantation Program. In addition to > 70 peer-reviewed publications, he has been invited all over the world as an expert speaker in the field pulmonary embolism therapy. We are fortunate to have him in-house to share his knowledge of what to do when the PE is starting to become overwhelming!
Clinical Pearls
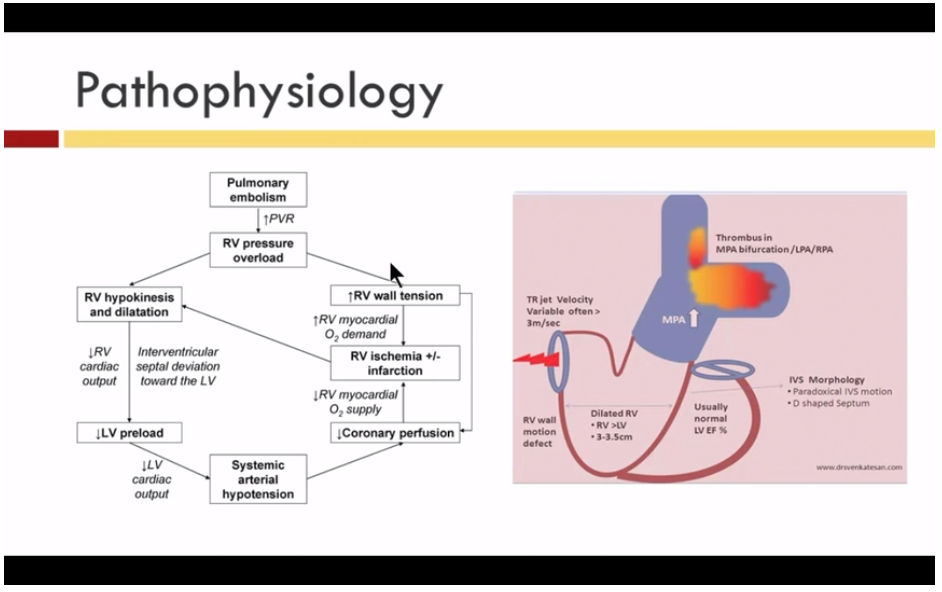
- Massive PE is defined by HD instability
- It is the HD compromise, not the hypoxia, that leads to morbidity/mortality
- Surgical embolectomy has become a mainstay of treatment (mortality as low as 5-10%)
- Intubation worsens mortality!
- Submassive PE is HD stable with RV strain/dysfunction (TTE, CT scan, troponin/BNP)
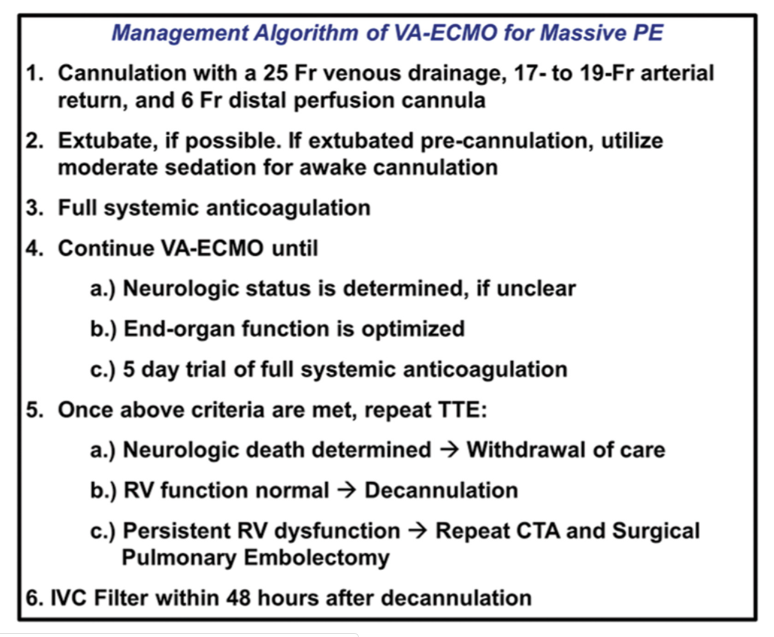
- VA-ECMO use has facilitated decompression of the right heart and improved outcomes
- Potential triage of patients who would benefit from embolectomy
- Algorithm: ECMO is initial strategy to recover organ function and either wean to survival, embolectomy, or to withdrawal of care.
- Decreased mortality (3% vs. 23%), decreased time from arrest to intervention (4 hrs vs. 11.5 hrs), and decreased need for surgical embolectomy (55% vs. 100%)
The Annals of Thoracic Surgery 2018 105, 498-504
- RV recovery on VA-ECMO dictated by:
- History of prior PE
- Chronic DVT (> 2 weeks)
- Higher BNP on presentation (not troponin!)
- Fallacies
- Too peripheral
- Distal, sub-segmental vessels can be accessed and removed
- Too invasive
- Minimally invasive approaches (5-7 cm incisions) can be used with excellent outcomes
- Hospital LOS: 4 days
- Can’t rehabilitate
- Cannulation does NOT require intubation
- All non-intubated ECMO pts can mobilize
- Random facts to know!
- Anatomic distribution or burden of clot DOES NOT correlate to clinical outcomes
- Chronic thromboembolic pulm HTN (CTEP) risk is 3%, though 5-10x the risk when presenting with pulm HTN + acute PE!
- Submassive PE + simple AC = > 50% risk for CTEP vs > 15% with thrombolysis (MOPETT)
- As PA pressure continues to increase, mortality worsens