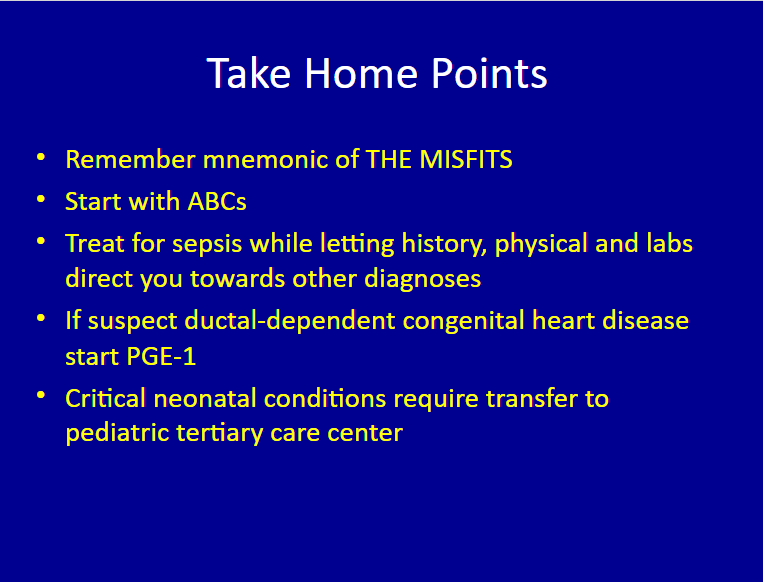
This summary, Slide 49, contains the critical take home points from this outstanding lecture:
For an outstanding free e-book on neonatology, please see The Iowa Neonatology Handbook:
The Iowa Neonatology Handbook is an ongoing effort by the Division of Neonatology at the University of Iowa Stead Family Children’s Hospital to provide physicians, nurses, and medical students who care for newborn infants a collection of protocols outlining rational approaches to the care of critically ill neonates. This document is not intended to be a comprehensive review of the field of neonatology, nor is it implied that the therapeutic approaches outlined in this book are established policies or standards of care. Rather, they represent a compilation of the experience and clinical styles of the members of our division and are intended only as a guide to therapy.
Here is a link to the outstanding Emergencies In The First Month Of Life From Children’s Hospital Of Philadelphia.
And here is the link to the outstanding clinical pathway ED Pathway for Evaluation/Treatment of Febrile Young Infants (0-56 Days Old) from CHOP.
Here is the link to The Clinical Pathways Library [a comprehensive list of the clinical pathways at Children’s Hospital of Philadelphia (CHOP)].
For a complete list of the outstanding pediatric FOAM courses from the Children’s Hospital of Philadelphia, please see CHOP Open-access Medical Education.
I’ve divided the slides of the lecture into 4 parts.
- Part 1 – Intro and Case 1: Sepsis
- Part 2 – Case 2: Intestinal Catastrophe
- Part 3 – Case 3: Congenital Adrenal Hyperplasia
- Part 4 – Summary and Case 4: Congenital Heart Disease
This post is Part 1. And here are some of the slides from Part 1 of the talk:
Slide 1
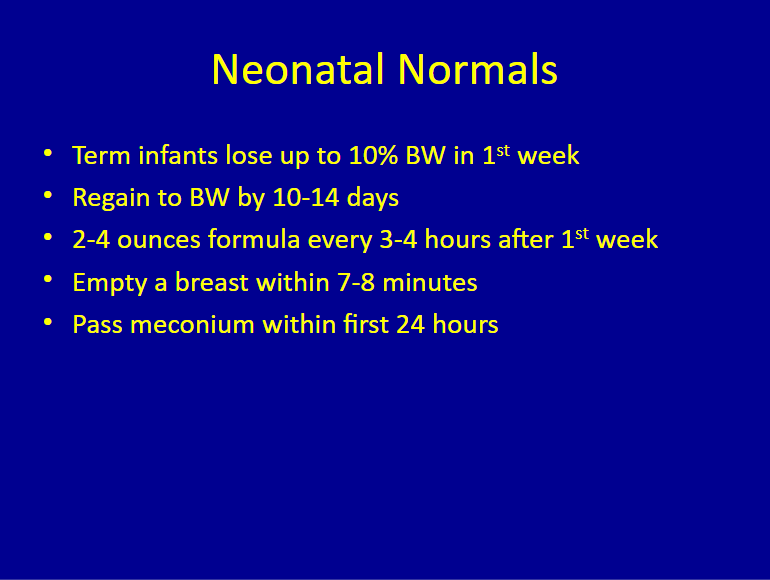
Slide 3
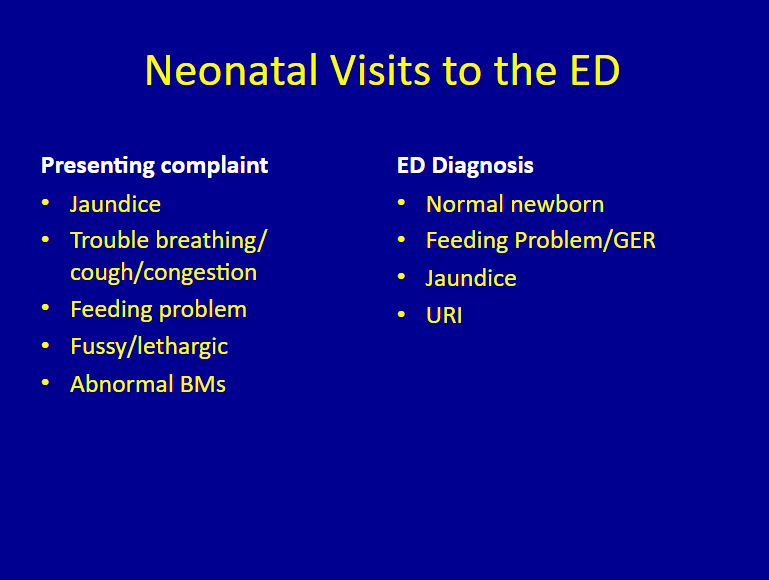
Slide 4
Slide 5
A potentially critically ill neonate is one whose breathing, crying, sleeping, feeding, peeing, or pooping is different from what the parents have learned to expect. If the parents are worried about their neonate, we (their physicians) should be too. It is not the parents job to prove the baby is ill. It is our job (as physicians) to prove that the baby is not sick.
Slide 6
Slide 7
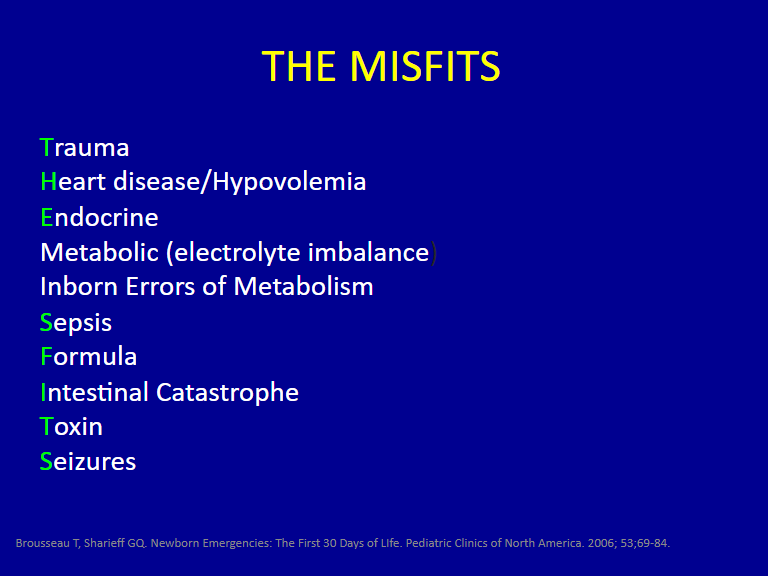
The mnemonic, THE MISFITS, is a way to remember the causes of illness in the newborn.
Slide 8
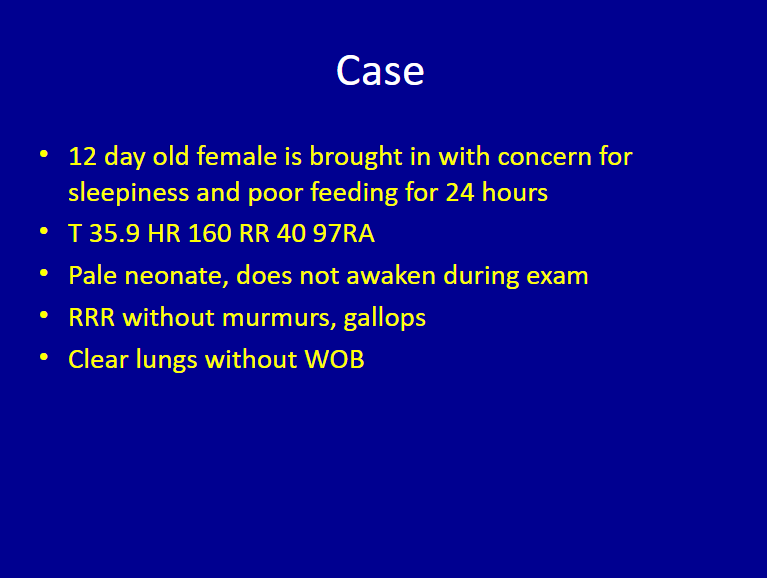
So we have a hypothermic, pale, lethargic infant.
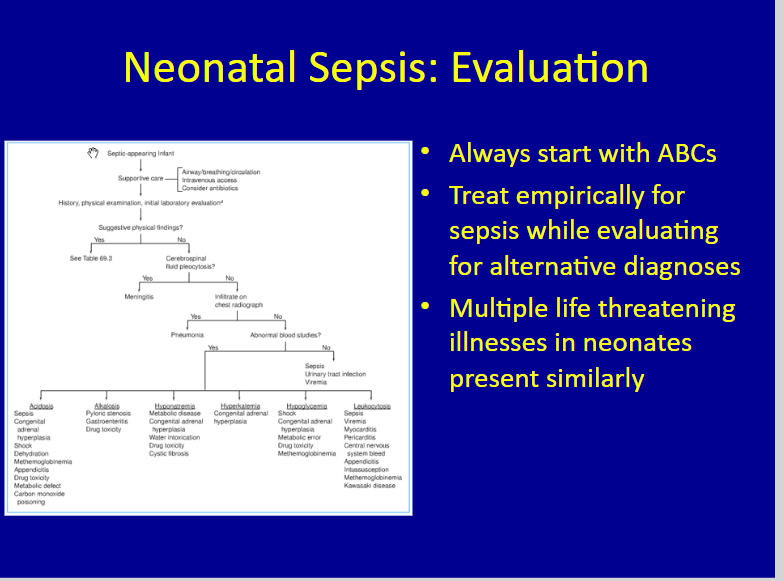
The patient above has Sepsis until proven otherwise.
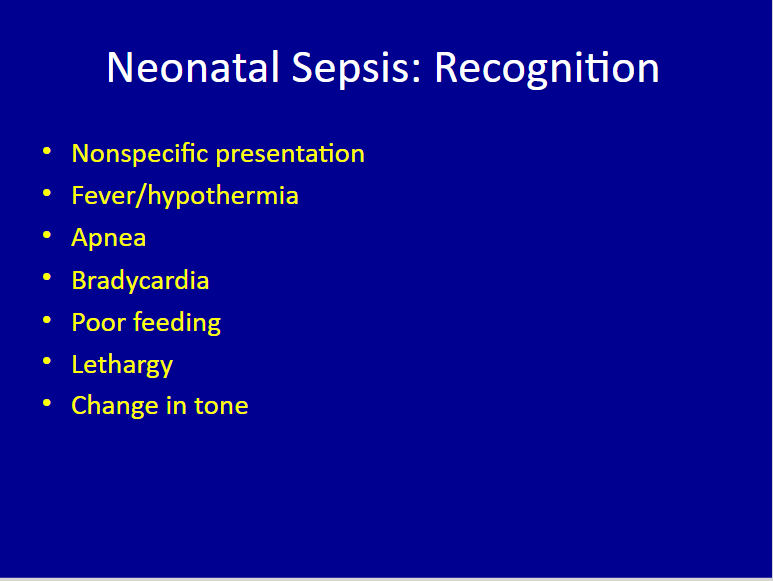
The presentation of neonatal sepsis can be very subtle in newborns. In addition to the more typical presentations that we see in older children like tachycardia, fever, increased work of breathing, vomiting, diarrhea, tachypnea; in young infants and neonates, they can have a very nonspecific presentation.
Instead of being of being febrile, they can be hypothermic as a sign of sepsis. Instead of tachypnea, they can actually have periods of apnea. Instead of being tachycardic, often times they are bradycardic.
And again, they may have very subtle signs like the mom may say, “he’s just not feeding well. “Something’s just not quite right.” “He’s not waking up to feed.” Or “his tone doesn’t . . .”
And these should all be red-flags.
Slide 11
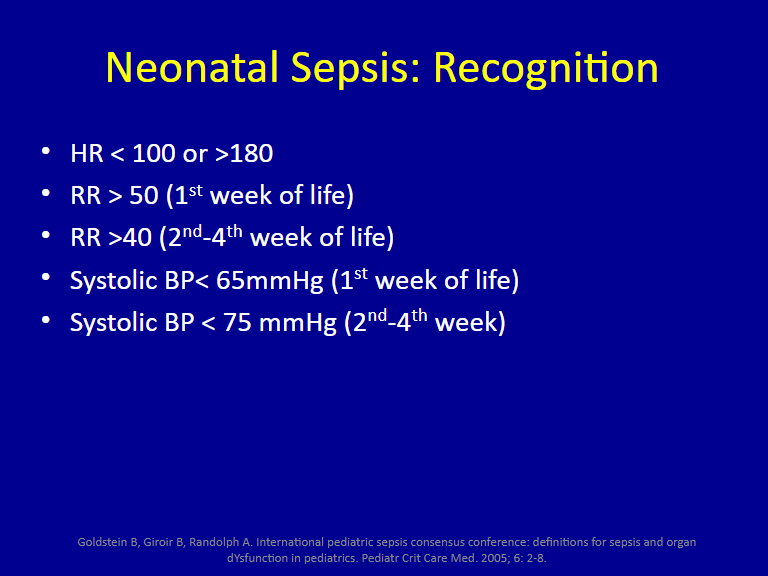
You should have a very low threshold for diagnosing sepsis.
Slide 12
Slide 13
See the CHOP Pathway for Evaluation and Treatment of Suspected Sepsis in N/IICU Patients posted September, 2018.
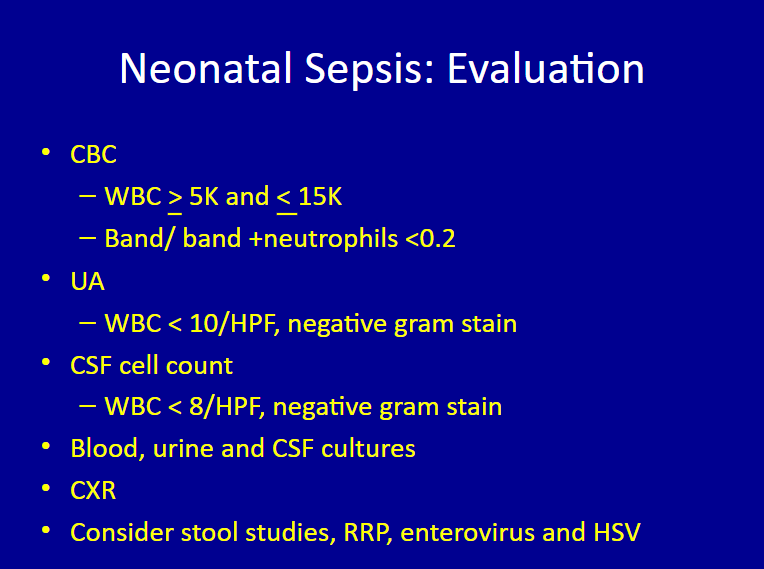
The labs listed below on slide 14:
Are not really helpful in this age population initially because these patients again are going to be treated empirically initially. [The labs may be useful later on as a baseline for trending. In addition to the labs below, a CRP and Procalcitonin can be ordered.]
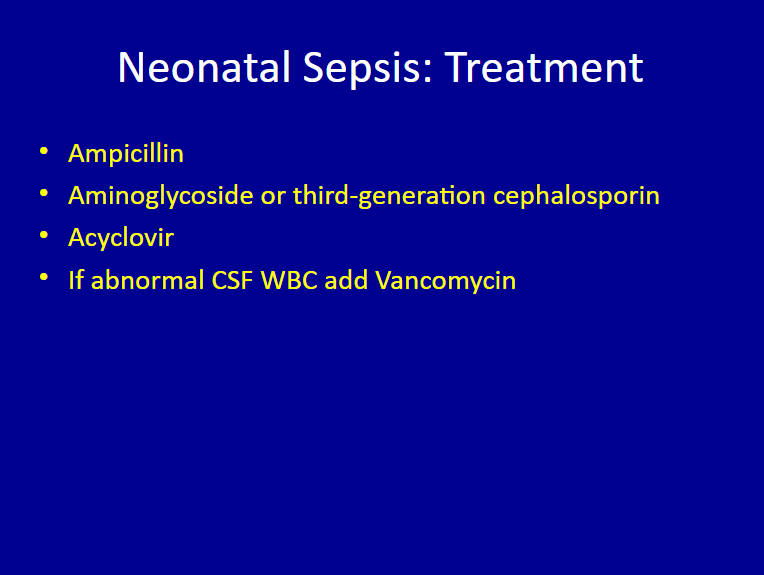
We treat empirically all patients less than 22 days with Acyclovir IV in addition to IV antibiotics.
Slide
Here is the link to “Emergencies In The First Month Of Life” – Case 2: Intestinal Catastrophe – Part 2 Of 4 – Lecture And Slides From CHOP With A Link To Newborn Fever Clinical Pathway.