The key to the topic of this post is understanding and accurately interpreting the urinalysis.*
*Link is to Urinalysis. Updated: Dec 15, 2015
Author: Edgar V Lerma, MD, FACP, FASN, FAHA, FASH, FNLA, FNKF from emedicine.medscape.com
What follows is an excerpt from Resource (2) below, Evaluation of Proteinuria [Podcast] [Script].
by peter.gill Jan 10, 2010 from Peds Cases*:
*Here is the complete list of the Table Of Contents of the PedsCases website. On this page the site has organized all of the contents into two groups: Clinical Presentation and Specialty Area.
When To Refer [A Patient With Proteinuria To The Pediatric Nephrologist]
You may come to a point at which you are out of your league and further assessment is required by a pediatric nephrologist. Some reasons to refer are:
- Documented presence of hematuria and proteinuria and/or persistent proteinuria.
- Nephrotic range proteinuria.
- Nephritic symptomatology.
- Signs of systemic disease such as joint pains, rash, etc. and suspect CT disease.
- Association with impaired renal function, and/or hypertension.
- Parental anxiety.
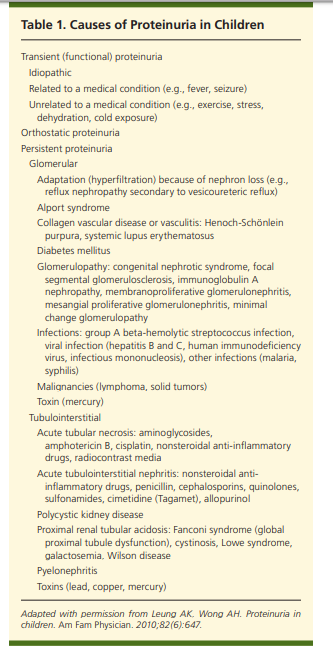
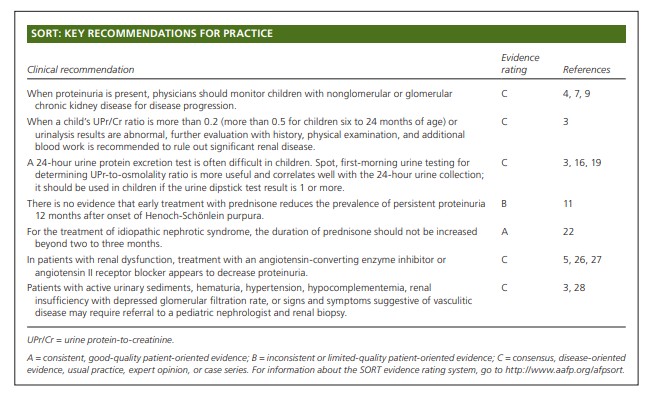
What follows are excerpts from Resource (1) below, Proteinuria in Children: Evaluation and Differential Diagnosis [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Am Fam Physician. 2017 Feb 15;95(4):248-254:
Abstract
Although proteinuria is usually benign in the form of transient or orthostatic proteinuria, persistent proteinuria may
be associated with more serious renal diseases. Proteinuria may be an independent risk factor for the progression of chronic kidney disease in children. Mechanisms of proteinuria can be categorized as glomerular, tubular, secretory, or overflow. A history, a physical examination, and laboratory tests help determine the cause. Transient (functional) proteinuria is temporary. It can occur with fever, exercise, stress, or cold exposure, and it resolves when the inciting factor is removed. Orthostatic proteinuria is the most common type in children, especially in adolescent males. It is a benign condition without clinical significance. Persistent proteinuria can be glomerular or tubulointerstitial in origin. The urine dipstick test is the most widely used screening method. Although a 24-hour urine protein excretion test is usually recommended for quantitation of the amount of protein excreted in the urine, it may be impractical in children. A spot, first-morning urine test for a protein-to creatinine or protein-to-osmolality ratio is a reliable substitute.
Treatment of proteinuria should be directed at the underlying cause. Patients with active urinary sediments, hematuria, hypertension, hypocomplementemia, renal insufficiency with depressed glomerular filtration rate, or signs and symptoms suggestive of vasculitic disease may require referral to a pediatric nephrologist and a renal biopsy. (Am Fam Physician. 2017;95(4):248-254. Copyright © 2017 American Academy of Family Physicians.)Mechanisms of Proteinuria
Mechanisms of proteinuria can be categorized as glomerular, tubular, secretory, or overflow.1,2,12,13
Glomerular proteinuria is due to increased filtration of macromolecules, particularly albumin, across the glomerular capillary wall.
Tubular proteinuria occurs when there is an increased excretion of normally filtered low-molecular-weight proteins because
of impaired reabsorption by the proximal tubules.12Secretory proteinuria results from oversecretion of certain proteins in the tubules, most notably the TammHorsfall proteins in interstitial nephritis.
Overflow proteinuria occurs when the plasma concentrations of low-molecular-weight proteins exceed the capacity of the tubules to reabsorb the filtered protein.
Clinical Evaluation
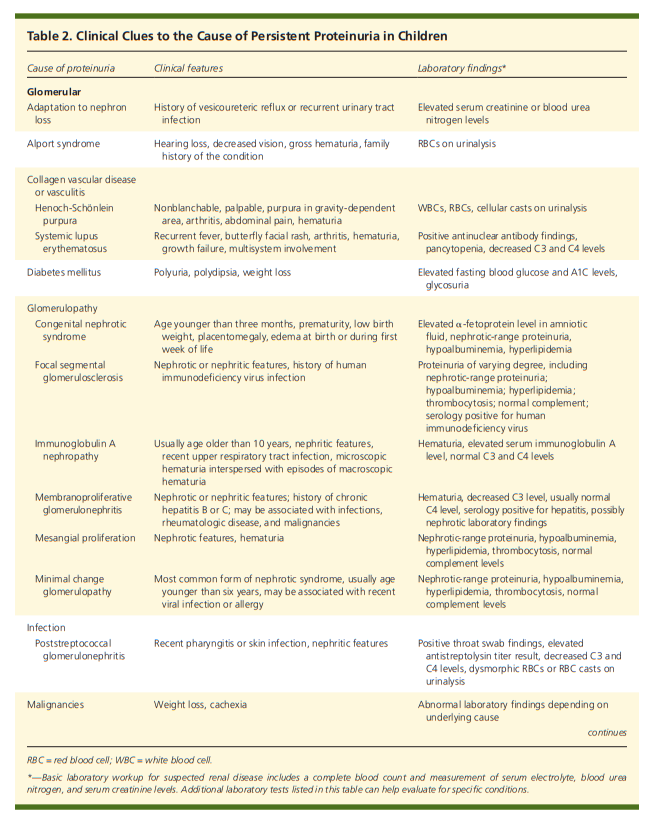
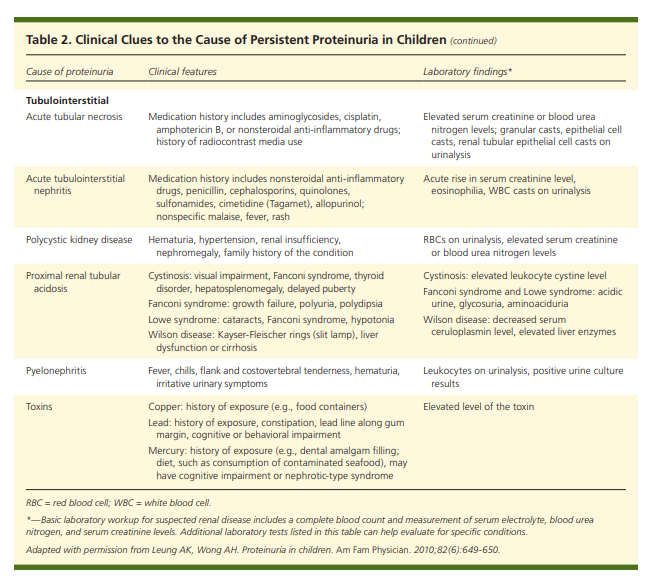
Table 2 lists clinical clues to the underlying cause of persistent proteinuria.1
Diagnostic Evaluation
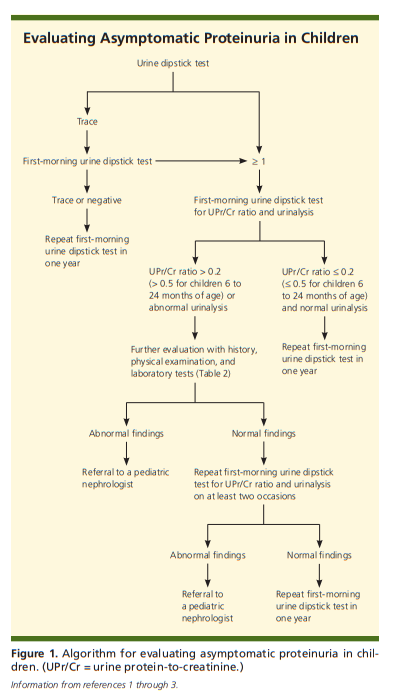
Proteinuria is often an incidental finding on urine dipstick testing or urinalysis. Children with asymptomatic proteinuria usually have the transient or orthostatic form. Figure 1 is an algorithm for the evaluation of asymptomatic proteinuria in children.1-3
Diagnostic Evaluation (continued)
If a urine dipstick test shows trace amounts of protein,
the test should be repeated with first-morning urine. If
the first-morning test shows a trace or negative amount
of protein, it should be repeated in one year to ensure that the proteinuria does not recur.1-3 In children with
a urine dipstick test showing a result of 1 or more, a
first-morning urine dipstick test for UPr/Cr ratio and
a urinalysis should be performed (urine bag collection
is acceptable in younger children). If the UPr/Cr ratio is 0.2 or less (0.5 or less for children six to 24 months of age) and urinalysis results are normal, transient or orthostatic proteinuria is likely.2 A repeat first-morning
urine dipstick test in one year should be considered. If
the UPr/Cr ratio is more than 0.2 (more than 0.5 for children six to 24 months of age) or urinalysis results are abnormal (e.g., hematuria, leukocyturia, active urinary sediments), persistent proteinuria or proteinuria of clinical significance is more likely,2 and further evaluation with history, physical examination, and additional laboratory testing is recommended to rule out significant renal disease.1-3Measurement of Proteinuria
OFFICE TESTING
The urine dipstick test uses the tetrabromophenol blue
colorimetric method and is the most widely used screening test.1,2,17 The test primarily detects albuminuria, with
a specificity and sensitivity of more than 99%, but it is
not sensitive for other proteins.18The intensity of color changes from yellow to blue correlates with the amount of protein in the urine: trace (15 mg per dL), 1+ (30 mg per dL), 2+ (100 mg per dL), 3+ (300 mg per dL), and 4+ (1,000 mg per dL or more).18
A reading of 1+ or more is considered abnormal.
A reading of 1+ or more is considered abnormal.
The dipstick urine test may yield false-positive results with alkaline urine (pH greater than 8); concentrated urine (specific gravity greater than 1.030); gross hematuria; pyuria; bacteriuria; prolonged immersion of reagent strip in the urine or placement of reagent strip directly in the urine stream; and presence of phenazopyridine (Pyridium), chlorhexidine (Peridex), benzalkonium, or an iodinated radiocontrast agent
in the urine.9,17The sulfosalicylic acid test detects all forms of protein
and is generally used as a supplementary test when the
presence of a low-molecular-weight or other protein is suspected but not detected by the dipstick urine test. In the
sulfosalicylic acid method, three drops of a sulfosalicylic
acid 20% solution are added to 5 mL of urine. Depending on the amount of protein precipitated, various grades of turbidity, from minimal (trace) to heavy flocculation (4+), are noted.9,17QUANTITATIVE LABORATORY TESTING
The first-line test is a 24-hour urine protein excretion.
In children, the normal amount of protein is less than
100 mg per m2 per day.3The spot UPr/Cr or UPr-to-osmolality ratio is a convenient and reliable method for estimating urine protein excretion without a 24-hour urine collection.16,19-21 To estimate the total amount of protein (g per m2 per day) in the urine, the UPr/Cr ratio can be
multiplied by 0.63.16OTHER LABORATORY TESTS
A complete blood count and measurements of serum electrolytes, blood urea nitrogen, and serum creatinine should be considered if renal disease is suspected. An elevation
in blood urea nitrogen or serum creatinine level suggests impaired renal function. Additional blood work should be ordered when indicated by history, physical examination,
or initial laboratory results.1-3,19IMAGING STUDIES
Ultrasonography of the urinary tract is an appropriate, noninvasive screening test for anatomic abnormalities and should be considered in patients with chronic kidney disease.1-3 A dimercaptosuccinic acid scan is the preferred study to detect renal scars.
RENAL BIOPSY
Renal biopsy is not routinely indicated in the workup of children with proteinuria.1,2 A biopsy should be considered when proteinuria is accompanied by active urinary sediments, persistent and gross hematuria, hypertension, hypocomplementemia, renal insufficiency with depressed glomerular filtration rate (less than 60 mL per minute
per 1.73 m2 for more than three months), or
signs and symptoms suggestive of vasculitic disease.3
Management
See pp 252 + 253 of the PDF.
Resources
(1) Proteinuria in Children: Evaluation and Differential Diagnosis [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Am Fam Physician. 2017 Feb 15;95(4):248-254.
(2) Evaluation of Proteinuria [Podcast] [Script].
by peter.gill Jan 10, 2010 from Peds Cases.