This post contains excerpts from and links to Resource (1) below from the 2011 AHA/ASA Scientific Statement On Cerebral Venous Thrombosis.
Epidemiology and Risk Factors for CVT
CVT is an uncommon and frequently unrecognized type of stroke that affects approximately 5 people per million annually and accounts for 0.5% to 1% of all strokes.1 CVT is more commonly seen in young individuals. According to the largest cohort study (the International Study on Cerebral Venous and Dural Sinuses Thrombosis [ISCVT]), 487 (78%) of 624 cases occurred in patients <50 years of age (Figure 1).1,6 Clinical features are diverse, and for this reason, cases should be sought among diverse clinical index conditions.
Clinical Diagnosis of CVT
Principal Clinical Findings
The diagnosis of CVT is typically based on clinical suspicion
and imaging confirmation. Clinical findings in CVT usually
fall into 2 major categories, depending on the mechanism of
neurological dysfunction: (1) Those that are related to increased intracranial pressure attributable to impaired venous drainage and (2) those related to focal brain injury from venous ischemia/infarction or hemorrhage. In practice, many patients have clinical findings due to both mechanisms, either at presentation or with progression of the underlying disease.
Headache, generally indicative of an increase in intracranial
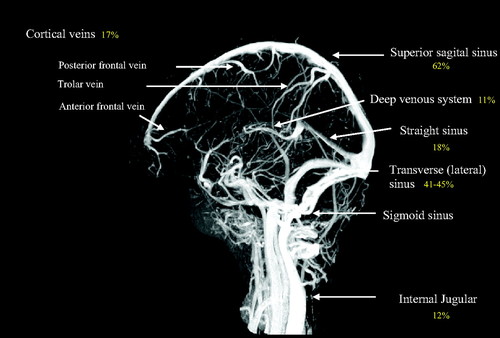
pressure, is the most common symptom in CVT and was present in nearly 90% of patients in the ISCVT.10 Similar headache frequency has been reported in other populations studied.63 The headache of CVT is typically described as diffuse and often progresses in severity over days to weeks. A minority of patients may present with thunderclap headache, suggestive of subarachnoid hemorrhage, and a migrainous type of headache has been described.64 Isolated headache without focal neurological findings or papilledema occurs in up to 25% of patients with CVT and presents a significant diagnostic challenge.65 CVT is an important diagnostic consideration in patients with headache and papilledema or diplopia (caused by sixth nerve palsy) even without other neurological focal signs suggestive of idiopathic intracranial hypertension. When focal brain injury occurs because of venous ischemia or hemorrhage, neurological signs and symptoms referable to the affected region are often present; most common are hemiparesis and aphasia, but other cortical signs and sensory symptoms may occur. Psychosis, in conjunction with focal neurological signs, has also been reported.66Clinical manifestations of CVT may also depend on the location of the thrombosis (Figure 2). The superior sagittal sinus is most commonly involved, which may lead to headache, increased intracranial pressure, and papilledema.67 . . .
Several important clinical features distinguish CVT from other mechanisms of cerebrovascular disease. First, focal or generalized seizures are frequent, occurring in 40% of patients. Second, an important clinical correlate to the anatomy of cerebral venous drainage is that bilateral brain involvement is
not infrequent. . . . CVT often present with slowly progressive symptoms. Delays in diagnosis of CVT are common and significant. In the ISCVT, symptom onset was acute (< 48 hours) in 37% of patients, subacute (>48 hours to 30 days) in 56% of patients, and chronic (>30 days) in 7% of patients. The median delay from onset of symptoms to hospital admission was 4 days, and from symptom onset to diagnosis, it was 7 days.10
Figure 2. Magnetic resonance venogram showing the cerebral venous system and most frequent (%) location of cerebral
venous and sinus thrombosis, as reported in the International Study on Cerebral Venous and Dural Sinuses Thrombosis
(n=624).44
Resources:
(1) Diagnosis and Management of Cerebral Venous Thrombosis: A Statement for Healthcare Professionals From the American Heart Association/American Stroke Association [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Stroke. 2011 Apr;42(4):1158-92. doi: 10.1161/STR.0b013e31820a8364. Epub 2011 Feb 3.
The above article has been cited by over 100 PubMed Central articles.