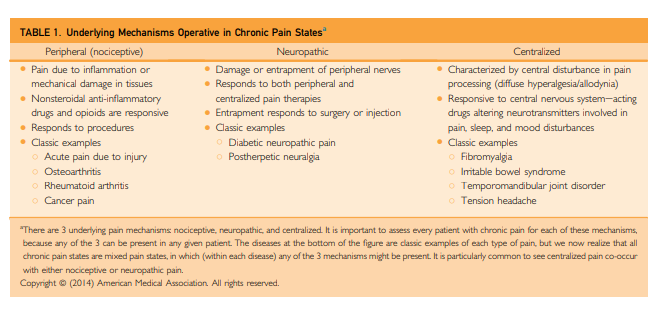
This post consists of excerpts from Fibromyalgia and Related Conditions [Full Text HTML] [Full Text PDF] by Dr. Daniel J. Clauw. n Mayo Clin Proc. 2015;90(5):680-692:
Abstract
Fibromyalgia is the currently preferred term for widespread musculoskeletal pain, typically accompanied by other symptoms such as fatigue, memory problems, and sleep and mood disturbances, for which no alternative cause can be identified. Earlier there was some doubt about whether there was an “organic basis” for these related conditions, but today there is irrefutable evidence from brain imaging and other techniques that this condition has strong biological underpinnings, even though psychological, social, and behavioral factors clearly play prominent roles in some patients. The pathophysiological hallmark is a sensitized or hyperactive central nervous system that leads to an increased volume control or gain on pain
and sensory processing. This condition can occur in isolation, but more often it co-occurs with other conditions now being shown to have a similar underlying pathophysiology (eg, irritable bowel syndrome, interstitial cystitis, and tension headache) or as a comorbidity in individuals with diseases characterized by ongoing peripheral damage or inflammation (eg, autoimmune disorders and osteoarthritis). In the latter
instance, the term centralized pain connotes the fact that in addition to the pain that might be caused by peripheral factors, there is superimposed pain augmentation occurring in the central nervous system. It is important to recognize this phenomenon (regardless of what term is used to describe it) because individuals with centralized pain do not respond nearly as well to treatments that work well for peripheral pain (surgery and opioids) and preferentially respond to centrally acting analgesics and nonpharmacologicaltherapies.[Introduction]
Fibromyalgia (FM) is the currently preferred term for widespread musculoskeletal pain for which no alternative cause can be identified. Every subspecialist sees the same individuals,
typically because these individuals present with pain in the region of the body the subspecialist specializes in.Gastroenterologists see the very same patients and focus on their gastroenterological symptoms and often use the terms
such as functional gastrointestinal disorder, irritable bowel syndrome (IBS), nonulcer dyspepsia, or esophageal dysmotility to explain the patients’ symptoms. Urologists focus on their genitourinary symptoms and use terms such as interstitial
cystitis or chronic prostatitis, and gynecologists use terms such as vulvodynia, vulvar vestibulitis, and endometriosis.Overview
Fibromyalgia is generally considered to be the second most common “rheumatic” disorder, behind osteoarthritis. Depending on the diagnostic criteria used, the prevalence in the population
ranges from 2% to 8%.1-3The new diagnostic criteria for FM published in 2010 and 2011 no longer require performing a tender point count to make the diagnosis and instead ask about the constellation of nonpain somatic symptoms that are typically present in addition
to widespread pain (eg, fatigue, sleep disturbance, memory, and mood problems).The environmental factors that are most likely to trigger the development of FM are various types of “stressors,” typically that involve acute pain for at least a few weeks. Fibromyalgia or similar illnesses can be triggered by certain types of infections16 (eg, EpsteinBarr virus, Lyme disease, Q fever, and viral hepatitis), trauma17 (motor vehicle collisions), or deployment to war.18 Psychological stress is but one such stressor that can trigger this complex symptom.
The physiological hallmark of centralized pain, central sensitization, or FM is augmented CNS pain processing. This was originally identified in FM by noting that these patients are
diffusely tender to palpation. The scientific terms for this phenomenon are diffuse hyperalgesia and allodynia. In the absence of an identifiable diffuse peripheral inflammatory process involving body tissues, diffuse hyperalgesia
and allodynia strongly suggests that the CNS (ie, spinal cord and brain) is somehow augmenting pain processing.Diagnosis Of FM
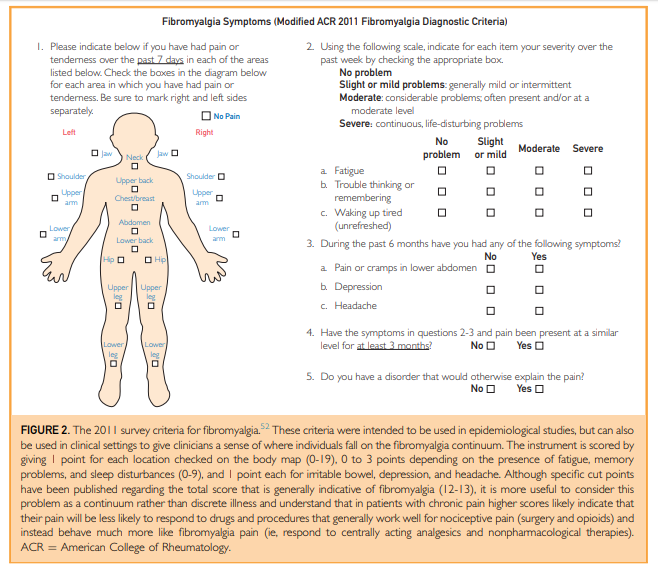
[We no longer do the tender points exam of the 1990 ACR FM criteria anymore], the alternative 2010 fibromyalgia criteria may represent a preferred manner of diagnosing, or thinking
about, FM.51-53 The survey criteria for FM are entirely self-reported by patients and can be administered on a single piece of paper. There is a body map with 19 areas (Figure 2) and a
symptom survey that asks about the presence and severity of fatigue, sleep disturbances, memory difficulties, and mood problems.In clinical practice, one should suspect centralized pain or FM in individuals with multifocal pain that cannot be fully explained
on the basis of damage or inflammation in those regions of the body. In most cases, musculoskeletal pain is the most prominent
feature, but because pain pathways throughout the body are amplified, pain can occur anywhere.[A Practical Way To Assess For Tenderness]
[One] way to assess the overall pain threshold is to
perform a rapid examination of the hands and arms by applying firm pressure over several interphalangeal joints and adjacent phalanges and then caudally to include firm palpation of the muscles of the forearm. If the individual is tender in many of these areas or just in the muscles of the forearm, the individual is likely diffusely tender (ie, have a low
central pain threshold). However, if the individual
is tender only in the interphalangeal joints and not the other regions, and especially if there is any swelling in these joints, one should be more concerned about a systemic
autoimmune disorder leading to tenderness confined to inflamed joints.[Laboratory studies are expected to be normal in FM and Central Pain Syndromes.] . . . those with acute or subacute onset of those symptoms require a much more aggressive
work-up. Simple testing should be limited to
complete blood cell count and routine serum chemistries, along with thyroid-stimulating hormone and erythrocyte sedimentation rate and/or C-reactive protein. Serological tests
such as antinuclear antibody and rheumatoid factor assays should generally be avoided unless there are features not seen in FM.Nonpharmacological therapies.
The 3 best studied nonpharmacological therapies are education, cognitive behavioral therapy, and exercise, and all these have strong evidence (level I, A) for use in FM. In fact, the effect size of these therapies often exceeds that of drug therapies, especially for improving function, which should be the therapeutic focus in treating chronic pain.59,60
Pharmacologic Therapy
Several drugs or classes of drugs have strong evidence (level I, A)for efficacy in FM,68 including tricyclic compounds69 (amitriptyline and cyclobenzaprine), gabapentinoids70 (pregabalin and gabapentin), serotonin-norepinephrine reuptake inhibitors (duloxetine71 and milnacipran72), and gamma hydroxybutyrate.35 [See WebMD article on gamma hydroxybutyrate – I would not prescribe this medication.]
Although there is a sense in clinical practice that the “FM
drugs” do not work as well for these patients as other classes of analgesics work for other types of pain, this is simply not true. All oral analgesics are at best modestly effective in
treating any type of chronic pain (ie, work well in a third of patients), including NSAIDs and opioids.77 In fact, there is emerging concern that opioids might even be in part driving the hyperalgesia seen in FM and other centralized pain states or frequently leading to opioid-induced hyperalgesia.Conclusion
Once pain centralization occurs, regardless of the underlying “disease” that might have originally led to pain, it is likely to respond tothe same types of treatments as FM. Most importantly, once centralization/FM occurs, these
individuals will be less responsive to our mainstays of treating ongoing peripheral nociceptive pain (eg, opioids, injections, and surgical procedures) and more responsive to centrally acting analgesic and nondrug therapies.