This blog is basically my study notes and my peripheral brain. Placing my notes online makes makes them available to me anywhere. And that is because the excellent built-in search function of the content management software [WordPress] makes it easy to find my notes on any topic when I want to review them.
This post consists of excerpts from Chapter 10 Head Trauma and Traumatic Brain Injury, pp 189 – 207 and from Chapter 17 Pediatric Trauma, pp 325 – 347 of The International Trauma Life Support Course For Emergency Care Providers, 8th ed, 2016. [Please note, this is not an affiliate link.]
* Here are links to:
And here are the excerpts:
Glasgow Coma Scale – Adult
Neurologic Exam
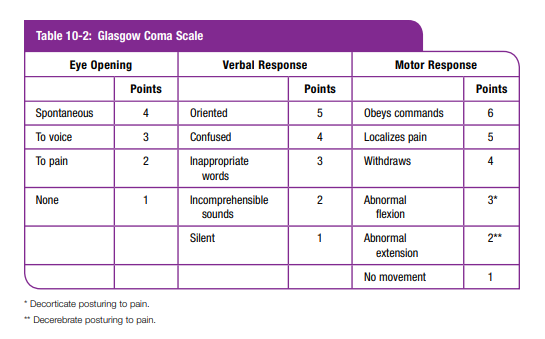
To apply the revised trauma score and other field triage scoring systems, you should be familiar with the Glasgow Coma Scale score (GCS). It is simple, is easy to use, and has good prognostic value for eventual outcome (Table 10-2). In the TBI patient, a Glasgow Coma Scale score of 8 or less is considered evidence of a severe brain injury. The GCS score determined in the field serves as the baseline for the patient; be sure to record it. You should note that early GCS assessment may not reflect the severity of the head injury itself because systemic causes (hypoxia, hypotension, hypoglycemia, alcohol, and so on) may cause altered mental status. Evaluation after the correction of those factors represents the severity of brain damage correctly. Record the score for each part of the GCS, not just the total score. You also should perform a finger-stick glucose on all patients with altered mental status. [Emphasis Added]
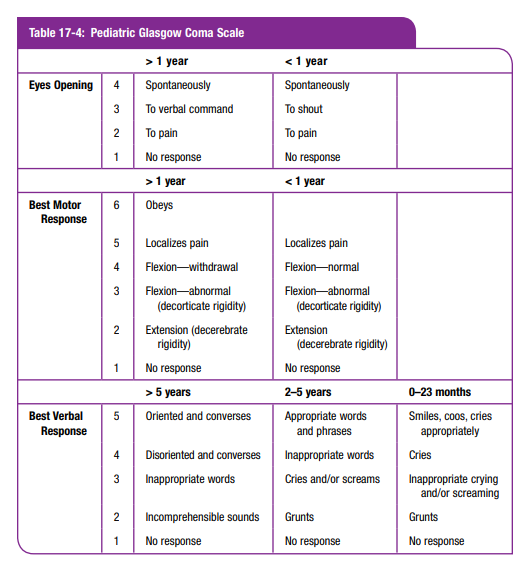
Glasgow Coma Scale – Pediatric
Initial Assessment
During the initial assessment your neurologic exam is limited to level of consciousness and any obvious paralysis. Level of consciousness is the most sensitive indicator
of brain function. Initially, the AVPU (alert, responds to verbal stimuli, responds to pain, and unresponsive) method is adequate. (See Chapter 2.) If there is a history of trauma to the head, or if the initial exam reveals an altered mental status, then the rapid trauma survey will include a more complete neurologic exam. A decrease in the level of consciousness is an early indicator of a brain injury or rising ICP.Control of the airway cannot be overemphasized. The supine, restrained, and unconscious patient is prone to airway obstruction from the tongue, blood, vomit, or other
secretions. Vomiting is very common within the first hour following a head injury. Suction should be immediately available.Pearls
Vomiting
Patients with head trauma frequently vomit. You must remain alert to prevent aspiration. If the patient is unconscious, with loss of protective reflexes, you should
insert an endotracheal tube. Otherwise, keep mechanical suction available and be prepared to log
roll the patient onto his side (maintaining motion restriction of the spine).Rapid Trauma Survey
Perform a rapid trauma survey on all patients who have an abnormal level of consciousness. (See Chapter 2.)
Pupils
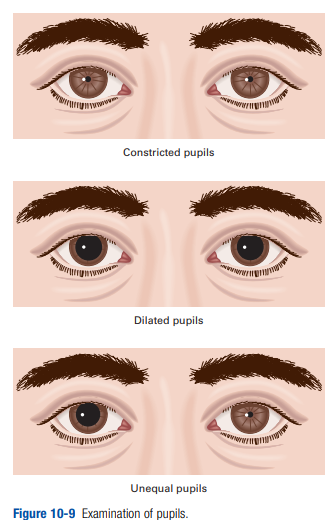
The pupils (Figure 10-9) are controlled in part by the
third cranial nerve. This nerve takes a long course through the
skull and is easily compressed by brain swelling and thus may
be affected by increasing ICP. Following a head injury, if both
pupils are dilated and do not react to light, the patient probably
has a brainstem injury, and the prognosis is grim. If the pupils
are dilated but still react to light, the injury is often still reversible, so every effort should be made to transport the patient quickly to a facility capable of treating a traumatic brain injury. A unilaterally dilated pupil that remains reactive to light may be the earliest sign of cerebral herniation. The development of a unilaterally dilated, nonreactive pupil (“blown pupil”) while you are observing the comatose patient is an extreme emergency and mandates rapid transport. Also consider initiating hyperventilation. Other causes of dilated pupils that may or may not react to light include hypothermia, lightning strike, anoxia, optic nerve injury, drug effect, or direct trauma to the eye. Fixed and dilated pupils signify increased ICP only in patients with a decreased level of consciousness. If the patient has a normal level of consciousness, the dilated pupil is not from head injury (more likely due to eye trauma or drugs such as atropine).Fluttering eyelids are often seen with emotional disorders. Slow
lid closure (like a curtain falling) is usually caused by brain
injury or effect of toxins (such as alcohol or other sedatives).
Testing for a blink response (corneal reflex) by touching the cornea with the edge of a gauze pad or cotton swab, or by applying overly noxious stimuli to a patient to test for response to pain, are techniques that are unreliable and do not contribute to prehospital assessment.Extremities
Note sensation and motor function in the extremities. Can patients feel you touch their hands and feet? Can they wiggle their fingers and toes? If patients are unconscious, note their response to pain. If they withdraw or localize to the pinching
of the fingers and toes, they have grossly intact sensation
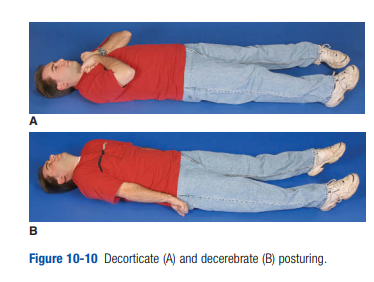
and motor function. This usually indicates that there is normal or only minimally impaired cortical function.Both decorticate posturing or rigidity (arms flexed, legs
extended) and decerebrate posturing or rigidity (arms and
legs extended) are ominous signs of deep cerebral hemispheric or upper brainstem injury (Figure 10-10). Decerebrate
posturing is worse and usually signifies cerebral herniation.
It is one of the indications for hyperventilation. Flaccid
paralysis usually denotes spinal-cord injury.
I recently completed the Advanced International Trauma Life Support Course (ITLS) at IU Health Methodist Hospital in Indianapolis. It was an excellent course and I believe that any clinician interested in trauma care will benefit from it.
This post contains excerpts from International Trauma Life Support For Emergency Care Providers Provider Manual, 2016*.
* Here are links to: