In this post I link to and excerpt from the chapter Hypokalemia, December 5, 2019, of Dr. Farkas’ incredible Internet Book Of Critical Care [Link is to TOC]. And after reviewing the chapter, listen to the wonderful 25 minute summary podcast of the chapter.
Dr. Farkas has created this Table of Contents of the chapter and each heading is a direct link to that part of the chapter! Awesome.
CONTENTS
Here are excerpts from the hypokalemia chapter:
physiology: potassium pharmacokinetics
the potassium deficit is often large
- Patients with hypokalemia often have a large total-body potassium deficit. This varies depending on acid/base status, but to get a general idea: (31227226)
- K of 3 mEq/L may correlate with a potassium deficit of 100-200 mEq.
- K of 2 mEq/L may correlate with a potassium deficit of 400-600 mEq.
estimating the potassium deficit in clinical context
- This depends on two factors:
- The serum potassium level.
- The presence of any factors which may cause shifting of potassium in or out of the cells.
- For example, diabetic ketoacidosis causes potassium to shift out of the cells. Therefore, the potassium deficit may be even larger than would be estimated based on the above formula.
most of the deficit occurs intracellularly
- The vast majority of potassium in the body is located intracellularly. Thus, most of the total body potassium deficit represents deficient intracellular potassium.
- The intracellular nature of the potassium deficit means that IV potassium must be administered slowly:
- Time is required for potassium to enter the cells.
- Rapid administration may cause serum levels to be elevated (even though there is a total-body potassium deficit!). Serum hyperkalemia is dangerous. Furthermore, serum hyperkalemia may cause poor retention of potassium (as it will tend to encourage potassium excretion in the urine).
- Bedside clinical implications:
- (1) IV potassium should never be given as a bolus.
- (2) Even in severely hypokalemic patients, aggressive IV potassium administration can be dangerous (more on this below).
diagnosis
causes of spuriously low lab values (pseudo-hypokalemia)
- (1) Delayed sample analysis (cells absorb potassium while the blood tube is sitting around).
- (2) Markedly elevated cell counts.
- Leukocytes take up potassium while the blood is awaiting analysis.
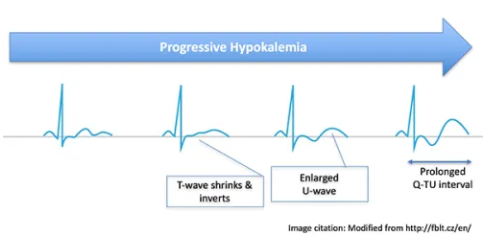
EKG changes
- T-wave abnormalities
- May flatten or invert.
- Inverted T-wave followed by prominent U-wave may create a biphasic “down-up” morphology.
- U-wave prominence
- May fuse with the T-wave to produce a prolonged QT interval (technically a Q-T-U interval).
- ST segments may appear depressed.
- QT prolongation, which may predict risk of arrhythmia.
- Arrhythmias
- Torsades de pointes may be the most classic.
- Other possibilities include atrial fibrillation, ventricular tachycardia, and ventricular fibrillation.
clinical significance
causes [For specifics please see this section of Dr. Farkas post]
reduced potassium intake (rarely the sole cause)
potassium shifts into the cells
extra-renal potassium loss
renal potassium loss
- Secondary to another electrolyte abnormality
- Hypomagnesemia
- Metabolic alkalosis
- Polyuria with increased distal delivery of sodium and water to the tubule
- Non-potassium-sparing diuretics (e.g. thiazides, loop diuretics, acetazolamide, mannitol)
- Sodium-wasting nephropathy (e.g. post-ATN or post-obstructive)
- High-dose penicillins
- Mineralocorticoid excess
- Cushing’s syndrome
- Primary hyperaldosteronism
- Exogenous steroid
- Licorice ingestion
- Renal tubular acidosis types I or II (see table below)
workup
(1) check additional electrolytes
- The magnesium level is the most important contributing factor, for several reasons:
- (a) Hypomagnesemia is common (most patients with hypokalemia have hypomagnesemia as well).(29540487)
- (b) Treatment of hypomagnesemia may be required to effectively treat hypokalemia.
- (c) Expedient treatment of hypomagnesemia may reduce the risk of Torsade de pointes.
- May consider checking a full electrolyte panel (including Calcium, Magnesium, and Phosphate):
- Electrolyte abnormalities often occur in pairs and triplets (“electrolytic disarray”).
(2) review the medication list, focusing on:
- Diuretics
- Insulin
- Beta-agonists
- Steroid
- Antibiotics
- High-dose penicillins
- Amphotericin
- Aminoglycosides
- Tenofovir, anti-retrovirals
- Foscarnet
- Chemotherapeutics
- Platinum agents
- Ifosfamide
- Miscellaneous
- Mafenide acetate
- NSAIDs
- Lithium
- Topiramate
- Valproic acid
(3) review recent history & data
- Historical clues:
- Diarrhea
- Polyuria
- Profound sweating
- Vomiting or gastric suction
- Lab clues:
- Nonanion-gap metabolic acidosis (look for RTA-1 or RTA-2)*
- [*See Metabolic Acidosis Etiology from emedicine.medscape.com.
- [*See Anion Gap for information on calculation and interpretation of the Anion Gap from emedicine.medscape.com.]
- Metabolic alkalosis (may cause hypokalemia, but can also result from hypokalemia!)
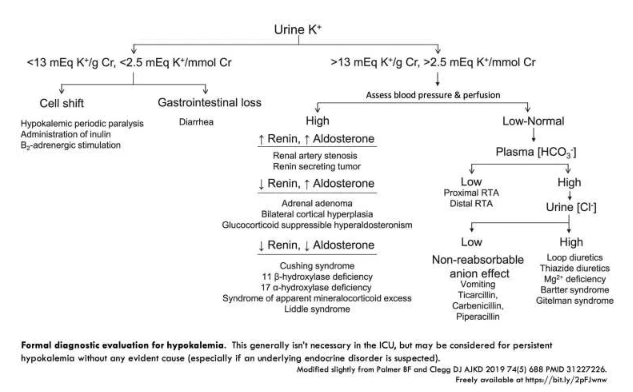
(4) additional diagnostic tests?
- Fancy evaluations usually aren’t needed.
- Careful consideration of the above etiologies combined with the clinical context will usually provide an explanation for the hypokalemia.
- Urine potassium measurement may be more helpful for outpatients (who may have surreptitious vomiting or laxative abuse).
- Persistent hypokalemia despite repletion usually implies renal potassium-wasting (in an ICU patient with no evidence of extra-renal potassium loss).
- Among patients with hypertension, metabolic alkalosis, and ongoing potassium wasting, evaluation of the renin-angiotensin-aldosterone system may be considered. This may be accomplished by checking renin and aldosterone levels.
- An approach to further evaluation of hypokalemia is shown below:
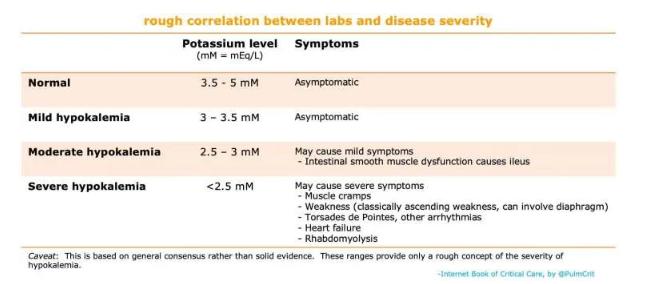
risk stratification
risk factors for complications from hypokalemia
- Severe hypokalemia (potassium <2.5 mM).
- Clinical context where potassium is likely to fall further (e.g. DKA or re-feeding syndrome)
- EKG changes due to hypokalemia (e.g. QT prolongation).
- Increased risk of arrhythmia:
- Patients on digoxin
- Myocardial ischemia or scarring
- Concomitant deficiency of magnesium
hypokalemia is generally well tolerated
- Overall, hyperkalemia is much more dangerous than hypokalemia.
- In the absence of the above factors, hypokalemia is well tolerated (and can be treated gradually).
- For patients with hypokalemia plus hypomagnesemia, a reasonable strategy is often to treat the hypomagnesemia fairly aggressively (because this is safe), but to be a bit more conservative with treatment of hypokalemia.
- 🔑 For patients with hypokalemia and hypomagnesemia, rapid correction of hypomagnesemia is safe and may quickly decrease the risk of arrhythmia.
target potassium level? [See Chapter section for details]
most patients: target >3.5 mM ?
renal failure: target >3 mM ?
diabetic ketoacidosis: target >5.3 mM ?