In this post I link to and excerpt from the chapter Hyperkalemia, November 2, 2018, of Dr. Farkas’ incredible Internet Book Of Critical Care [Link is to TOC]. And after reviewing the chapter, listen to the wonderful 20 minute summary podcast of the chapter.
Dr. Farkas has created this Table of Contents of the chapter and each heading is a direct link to that part of the chapter! Awesome.
CONTENTS
All that follows are excerpts from the Hyperkalemia Chapter of The Internet Book Of Critical Care [except where noted – material in brackets]:
Diagnosis of hyperkalemia
clinical presentations
- Left untreated, hyperkalemia may manifest in the following ways:
- Neuromuscular weakness (uncommonly seen).
- Bradycardia
- Ventricular tachycardia/fibrillation, sudden cardiac death.
- In practice, most patients are asymptomatic (even with severe hyperkalemia).
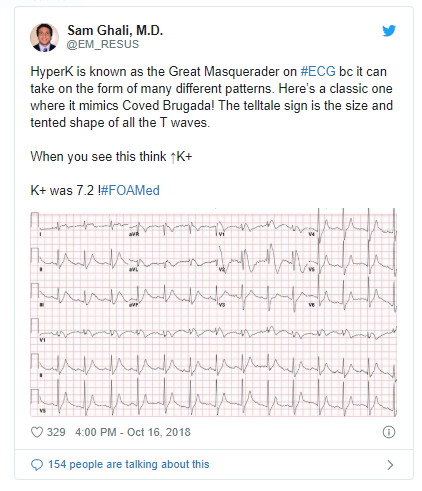
EKG diagnosis
- Hyperkalemia can cause a very wide range of EKG changes.
- The textbook sequence of changes illustrated above often doesn’t occur.1 Instead, hyperkalemia can mimic a wide variety of pathologies (including STEMI and all varieties of bundle/conduction blocks).
- Severe hyperkalemia (e.g. K>7 mM) can occur without obvious EKG changes.
- The following patterns are highly suggestive of hyperkalemia. In an unstable patient, it may be reasonable to give IV calcium based on patterns #2-4 below while awaiting a potassium level.
- (1) Peaked T-waves
- Narrow, pointy, prominent T-waves.
- Often the most notable finding on the EKG (may be visible on bedside monitor as well).
- (2) Ventricular tachycardia mimic
- QRS wave widens and P-waves may disappear. If patient is tachycardic, this will look like ventricular tachycardia.
- Useful clues: Compared to ventricular tachycardia, T-waves can be sharper than would be usual and heart rate is often slower than would be typical.
- (3) Sine-wave pattern
- Profound widening of QRS complex and peaked T-waves mimics a sine wave.
- (4) Bradycardia
- Hyperkalemia can manifest with bradycardia (often in the context of other drugs that slow down the AV node).
- There should always be a high suspicion for hyperkalemia in any bradycardic patient, especially if there are other EKG findings to suggest hyperkalemia.
Here is the Twitter Link to the tweet below: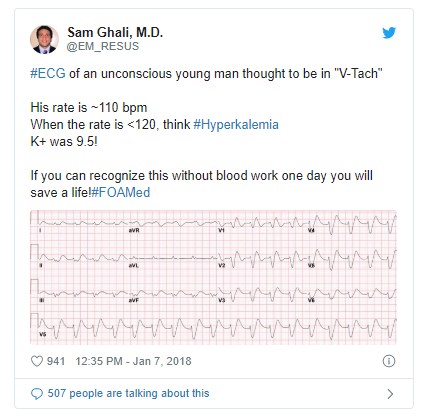
lab diagnosis
- Hyperkalemia is variably defined as potassium >5.5 mM or >5.0 mM, depending on the source.
- Pseudohyperkalemia refers to artificially elevated potassium due to:
- (a) Hemolysis
- (b) Severe polycythemias causing potassium release during clotting (e.g., platelets > 1 million or WBC count > 50,000). This can be avoided by point-of-care testing or measuring labs in a heparinized tube.
- (c) Prolonged tourniquet application.
- The first response to a lab report of hyperkalemia should be to look at the telemetry tracing and obtain an EKG.
- If the telemetry/EKG shows features of hyperkalemia, this confirms the diagnosis.
- If the lab reports severe hyperkalemia but the EKG is normal, repeat the lab.
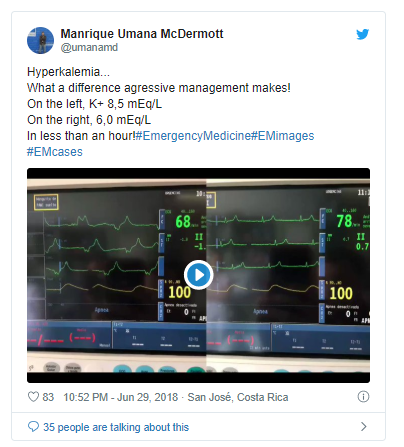
Here is the Twitter Link to the tweet below:
Causes of hyperkalemia
general concepts
- Normally the kidney will prevent hyperkalemia by increasing urinary potassium excretion. Persistent hyperkalemia implies dysfunction in renal potassium excretion.
- Critically ill patients often develop hyperkalemia due to a combination of several factors (e.g. hypovolemia plus renal dysfunction plus ACE-inhibitor). Successful treatment may require addressing many of these problems simultaneously.
investigation
- Review medication list and consider clinical context.
- Consider evaluation for cellular lysis (e.g. measure CK & LDH levels).
- Consider evaluation for adrenal insufficiency (e.g. random cortisol, ACTH stimulation test).3
Here is the Twitter Link to the tweet below: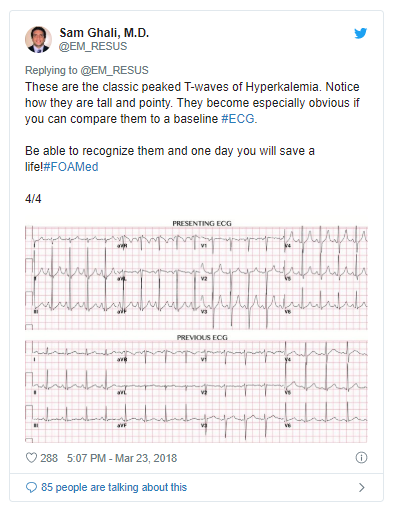
Risk stratification
The first step of treatment requires determining whether hyperkalemia is life-threatening (severe). No evidence-based definition for “severe” hyperkalemia exists (various articles use a range of semi-arbitrary definitions). Ultimately clinical judgement is needed, with attention to the following factors:
- Potassium level: above 6.5-7 mM is more worrisome.
- Chronicity:
- Chronic hyperkalemia is better tolerated (e.g. dialysis patients who frequently have hyperkalemia).
- Acute hyperkalemia is more dangerous.
- EKG changes: bradycardia, QRS widening, or junctional rhythm are particularly worrisome.4
- Ongoing potassium release (e.g. by tumor lysis syndrome or rhabdomyolysis) increases the likelihood of deterioration.
Treatment of moderate hyperkalemia
step 1: treat any definable causes
- Treat all identifiable causes of hyperkalemia.
- Discontinue any nephrotoxins and establish a state of euvolemia with adequate perfusion.
- Consider a renal diet with limited potassium intake.
step 2: gentle kaliuresis (renal excretion of potassium)
- Potassium excretion can generally be promoted using diuretic among patients able to produce urine (otherwise dialysis will be needed).
- Moderate hyperkalemia can generally be treated with a single diuretic (e.g. IV furosemide), followed by volume replacement with Lactated Ringer’s to maintain a net even fluid balance.
- If this regimen fails, more aggressive kaliuresis may be utilized with additional medications discussed below.
Rx severe hyperkalemia: Temporizing measures
Start here.