This blog and the posts on it are my study notes which I put up to help me reinforce my learning on the subjects I review.
So, I’m reviewing all of the excellent diagnostic schemas from the Clinical Problem Solvers.
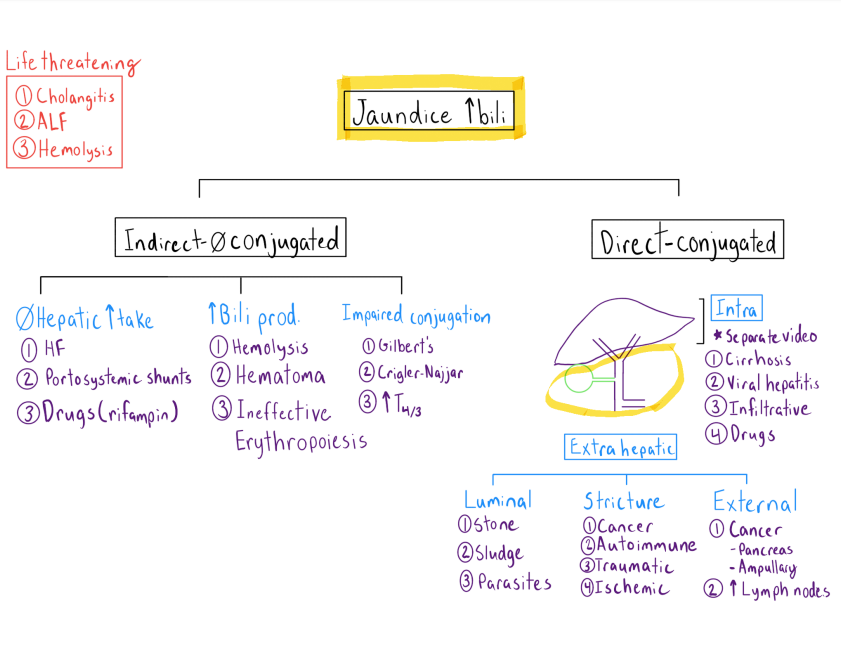
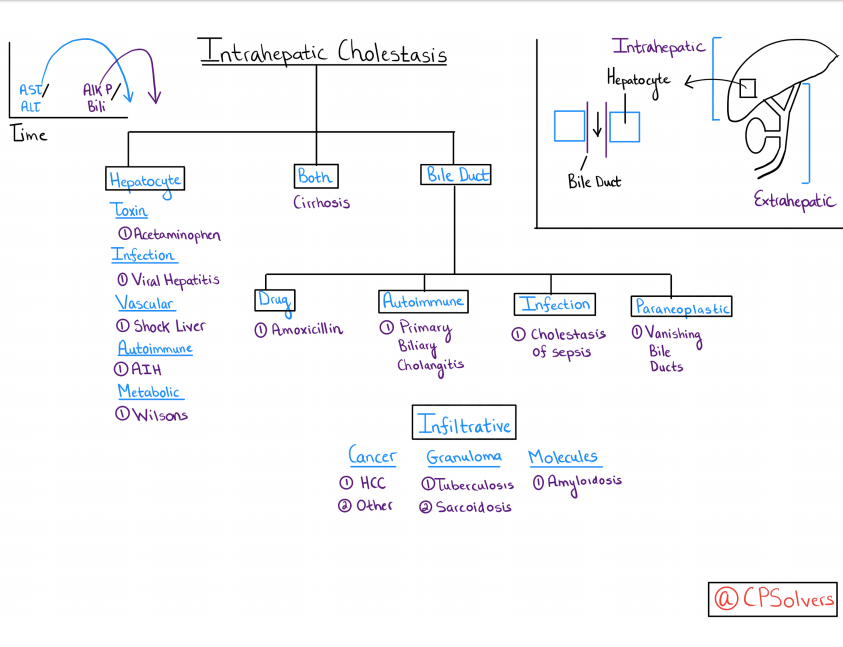
So today I review the diagnostic schemas for Jaundice [This link is to the web page where the video of the schema is discussed. Be sure to review the video].
And here is the link to the related podcast, Episode 5 – Jaundice.
The Can’t Miss Diagnoses for jaundice are:
- Cholangitis
- “Acute cholangitis can be diagnosed if the clinical manifestations of Charcot’s triad, i.e., fever and/or chills, abdominal pain (right upper quadrant or epigastric), and jaundice are present. … “Severe (grade III)” acute cholangitis is defined as acute cholangitis accompanied by at least one new-onset organ dysfunction.”
- Acute Liver Failure
- “Acute liver failure is an uncommon condition in which rapid deterioration of liver function results in coagulopathy, usually with an international normalized ratio (INR) of greater than 1.5, and alteration in the mental status (encephalopathy) of a previously healthy individual. Acute liver failure often affects young people and carries a very high mortality.”
- “The most important step in the assessment of patients with acute liver failure is to identify the cause, because certain conditions necessitate immediate and specific treatment and affect prognosis. All patients with clinical or laboratory evidence of moderate or severe acute hepatitis should have immediate measurement of prothrombin time (PT) and careful evaluation of the mental status. The presence of PT prolongation or mental status changes is grounds for hospital admission.”
- “Liver transplantation is the definitive treatment for acute liver failure.” [So immediate transfer to a liver transplant center is indicated as soon as the diagnosis of acute liver failure is made.]
- Hemolysis [Especially Thrombotic Thrombocytopenic Purpura]
- CLINICAL RECOMMENDATIONS
- “After hemolytic anemia is confirmed, a peripheral blood smear should be ordered to determine the etiology.”
- “Glucocorticoids are the first-line treatment of warm autoimmune hemolytic anemia.”
- “The PLASMIC score* can be used to assess the likelihood of thrombotic thrombocytopenic purpura when ADAMTS13 cannot be easily measured.”
- “Do not give antibiotics to children with Escherichia coli diarrhea because antibiotics increase the risk of hemolytic uremic syndrome.”
- “G6PD activity should be measured in infants with jaundice and a family history or geographic background suggestive of possible deficiency.”
- CLINICAL RECOMMENDATIONS
*Please see:
-
-
-
- Plasmic score applicability for the diagnosis of thrombotic microangiopathy associated with ADAMTS13-acquired deficiency in a developing country [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Hematol Transfus Cell Ther. 2019 Apr – Jun;41(2):119-124.
- PLASMIC Score for TTP from MDCalc
- “Predicts ADAMTS13 deficiency in suspected thrombotic thrombocytopenic purpura (TTP) with high discrimination.”
- “INSTRUCTIONS”
- “Use in hospitalized adult inpatients with suspected thrombotic thrombocytopenic purpura (TTP) who might benefit from early initiation of plasma exchange while awaiting ADAMTS-13 results. Do not use in patients who have already undergone plasma exchange (i.e., intermediate and high risk groups, in whom therapeutic plasma exchange must be initiated immediately).”
-
-
Here is the diagnostic schema: