In this post I link to and excerpt The Transcutaneous Pacing Section Of The Bradycardia Chapter From The Internet Book Of Critical Care [Link is to the Table Of Contents]. I do this so I will have this resource so that I will easily be able to locate this resource through my blog’s search function.
All that follows is from The Transcutaneous Pacing Section Of The Bradycardia Chapter From The Internet Book Of Critical Care.
transcutaneous pacing
Transcutaneous pacing is often the fastest strategy to increase the heart rate. Even if it doesn’t capture, the discomfort may be enough to trigger a sympathetic response that keeps the patient alive. Either way, this is a temporary measure until more definitive stabilization is possible (e.g. transvenous pacing).
pad configuration
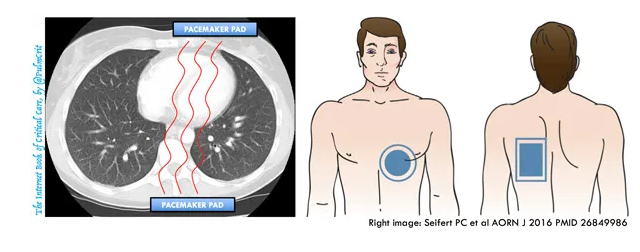
- Air is a poor conductor of electricity, so placing pads that overlie the lungs is a poor strategy.
- Anterior-posterior pad placement may be preferred (image above)12 13
- Anterior pad is on the left side of the lower part of the sternum, covering the “left parasternal window” of the heart. Based on experience with echocardiography, this is the most reliable site of contact between the heart and the soft tissue of the chest.
current
- If patient is crashing, start at maximal current and work your way down after the patient has stabilized.
- If patient is doing OK, then start low and titrate up.
- If the patient is doing OK, then you probably wouldn’t really want to do transcutaneous pacing at all. However, it may be useful to determine if the patient responds to transcutaneous pacing. Proving that transcutaneous pacing will capture the heart may help you decide whether placing a transvenous pacemaker is necessary in a borderline patient.
- Continue pacing at 10-20 mA above the minimum energy required for capture.
- Usually ~40-80 mA required to achieve capture (possibly more in obesity or obstructive lung disease).14
beware of pseudo-pacing
- Pseudo-pacing is when the pacemaker isn’t capturing the myocardium, but the monitor displays a heart rate equal to the transcutaneous pacemaker. This provides a false sense of security, because the monitor looks great.
- Always confirm that the pacemaker is capturing via one of the following methods:
- Pulse oximetry waveform shows a pulse matching the pacemaker (image above)
- Bedside echocardiogram confirms myocardial contraction with pacing
- Pulse, preferably far away from the chest (e.g. femoral pulse or dorsalis pedis, to avoid being fooled by twitching of the chest musculature)
analgesia/sedation?
- Can be limited by patient’s instability. Low-dose fentanyl and/or ketamine might be reasonable.
- Deep sedation & intubation to allow for tolerance of transcutaneous pacing is a popular approach, but probably not the best. The instability induced by sedation and intubation may out-weigh benefits from transcutaneous pacing. Also, if the patient becomes hyperinflated on the ventilator, this could theoretically lead to loss of capture by the transcutaneous pacer.