In addition to today’s post on ECG Cases 1 from Emergency Medicine Cases, below are two resources on the performance of and interpretation of ECGs.
Here is a link to Excerpts From “Recording a Standard 12-Lead Electrocardiogram” From The Society for Cardiological Science & Technology (SCST) 2017
Posted on June 25, 2019 by Tom Wade MD
Here are links to an outstanding YouTube minicourse: Best Minicourse On Electrocardiography From Girish Kalra MD Of Emory University School Of Medicine
Posted on June 26, 2019 by Tom Wade MD
And here is:
ECG Cases 1: Missed Ischemia – Never Trust the ECG Computer Interpretation [Link is to the post] from Emergency Medicine Cases. September, 2019. Written by Jesse McLaren; Edited by Anton Helman. September 2019 from Emergency Medicine Cases.
The following is all from ECG Cases 1:
In this ECG Cases – Missed Ischemia – Never Trust the ECG Computer Interpretation, we review ECGs from 7 patients presenting to the ED with chest pain, all of whom had a computer interpretation as “normal.” And guess what…they all show acute ischemia! Can you see what the computer couldn’t?
ECGs read as ‘normal’ by the computer
Automated interpretation has high rates of error for detecting ischemia, up to 42% for STEMI.[1] But what about those ECGs read as “normal”? A 2017 study concluded that “triage ECGs identified by the computer as normal are unlikely to have clinical significance that would change triage care. Eliminating physician review of triage ECGs with a computer interpretation of normal may be a safe way to improve patient care by decreasing physician interruptions.” [2]
But this was based on only 4 months of triage ECGs collected at a single centre with a low incidence of STEMI. A critical response explained both the shortcomings of the study, and a different approach to “normal” ECGs:
“Using non-blinded expert review rather than outcome as a reference standard precludes any meaningful conclusion about triage ECGs…A sample size of 855 has no chance of generating a meaningful conclusion about the reliability of computer ‘Normal.’…Physicians should take steps to develop their skills in detecting subtle signs of myocardial ischemia, and computerized interpretation algorithms should state ‘No abnormalities detected’ rather than ‘Normal ECG.’ ” [3]
The Cases [Note to myself: On reviewing this post, write down your own analysis and only then read the answer below the ECG]
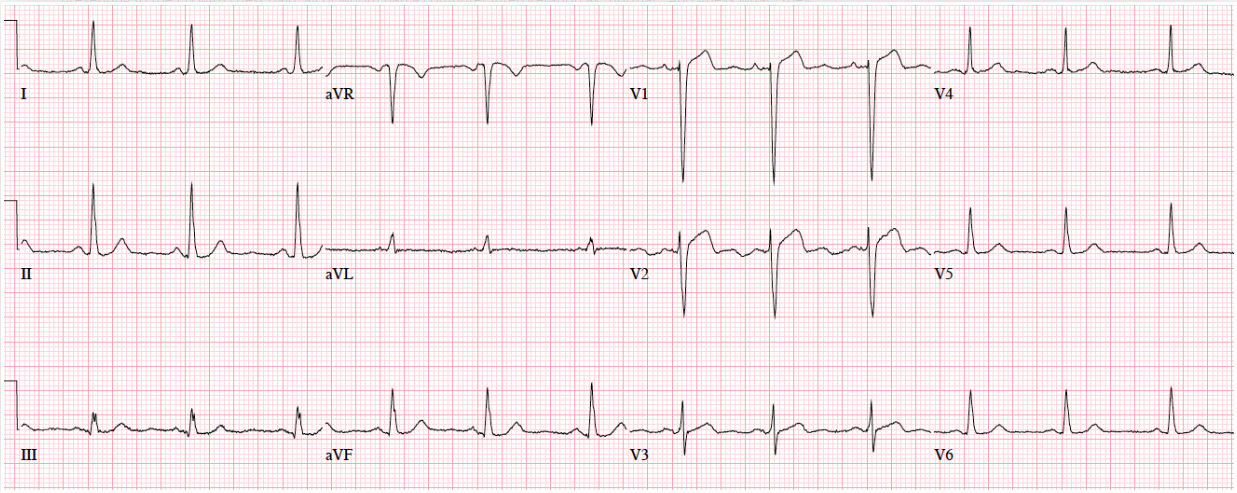
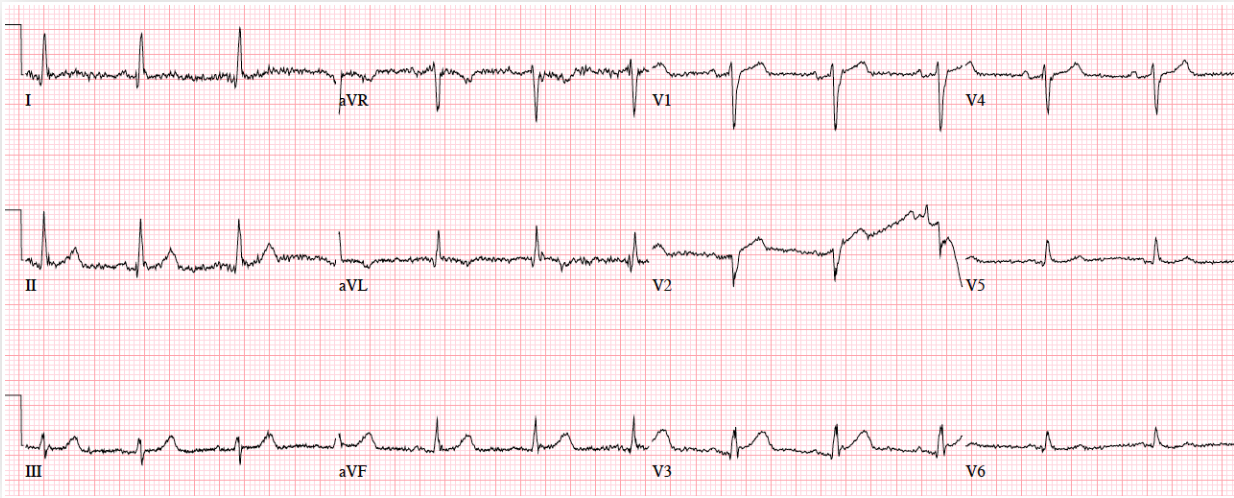
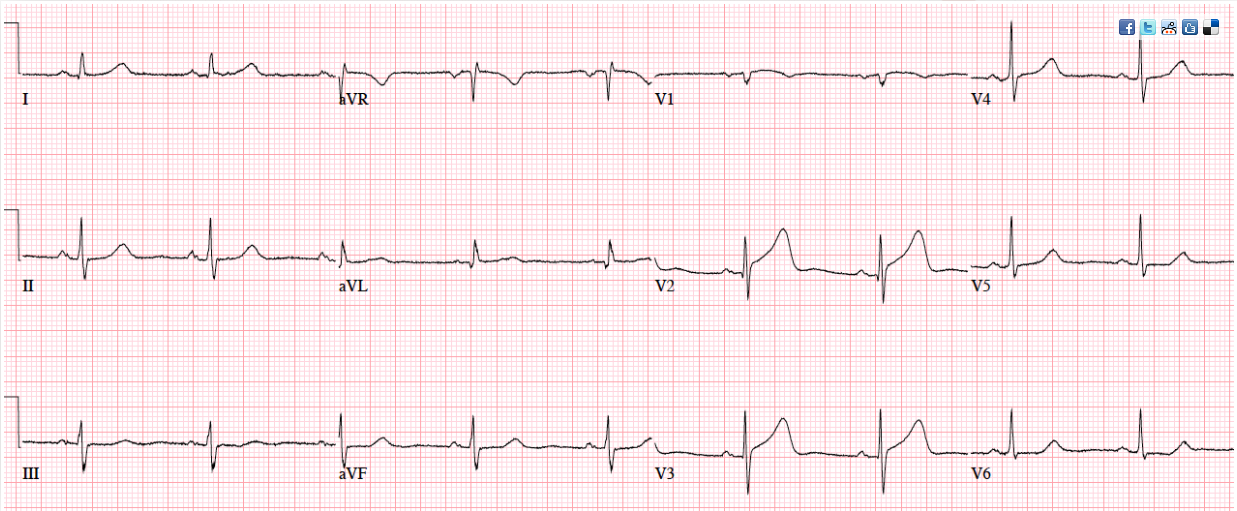
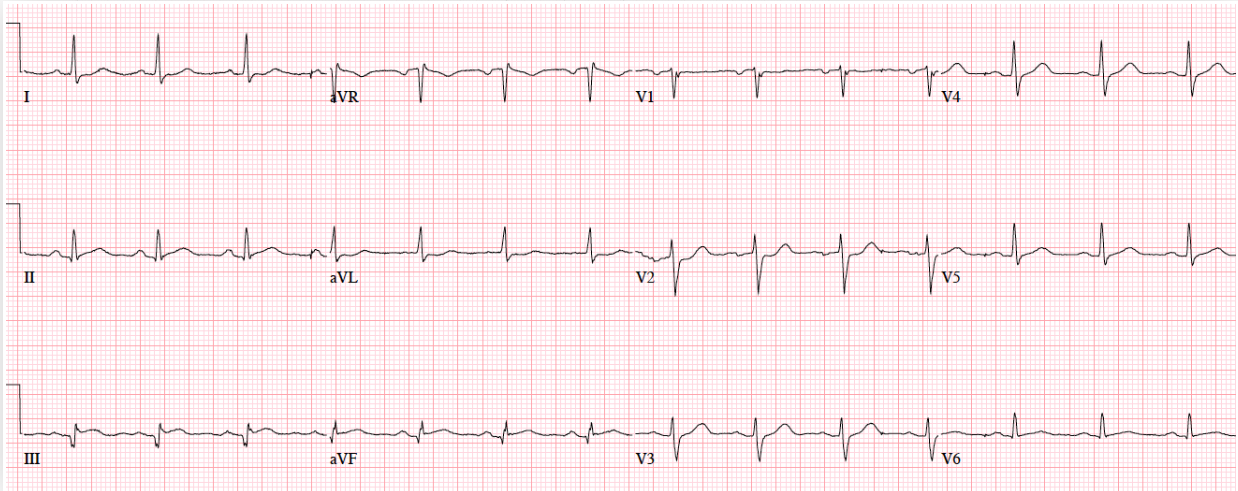
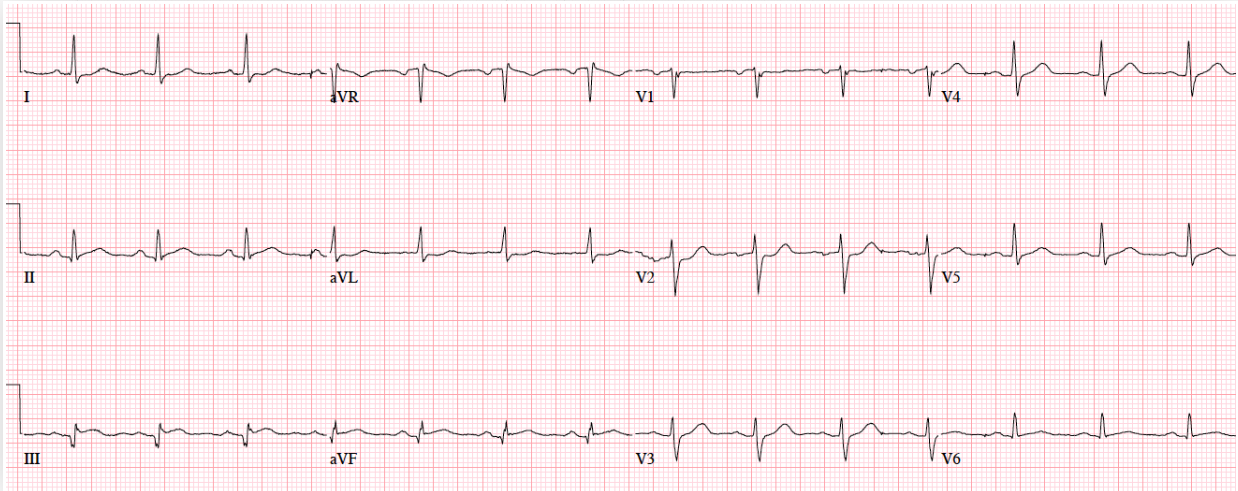
Patient 1. 65yo with hours of chest pain. No prior ECG
Answers to Patient 1. Ischemic ST morphology
My answer: ST elevation in V1 and V2
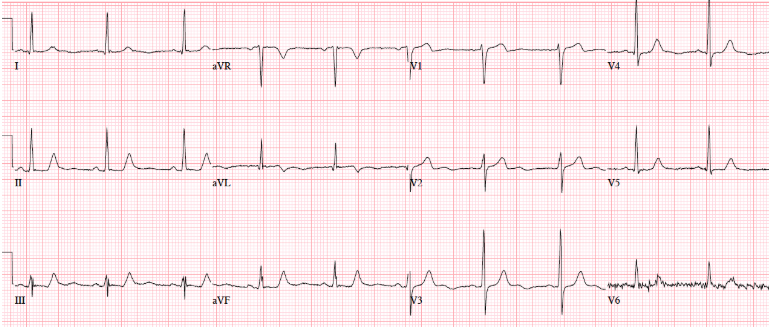
Blog Answer: NSR, normal conduction/axis/R wave, no hypertrophy. Mild ST elevation in V1-2 which could be normal, but the morphology is not: ST is convex in V2 and straight in V3. Plus there’s an inverted U wave in V2, another marker of LAD occlusion. When trop returned positive an hour later, repeat ECG below showed further convex ST in V1-2 and terminal T wave inversion, and cath lab was activated: 100% mid LAD occlusion.
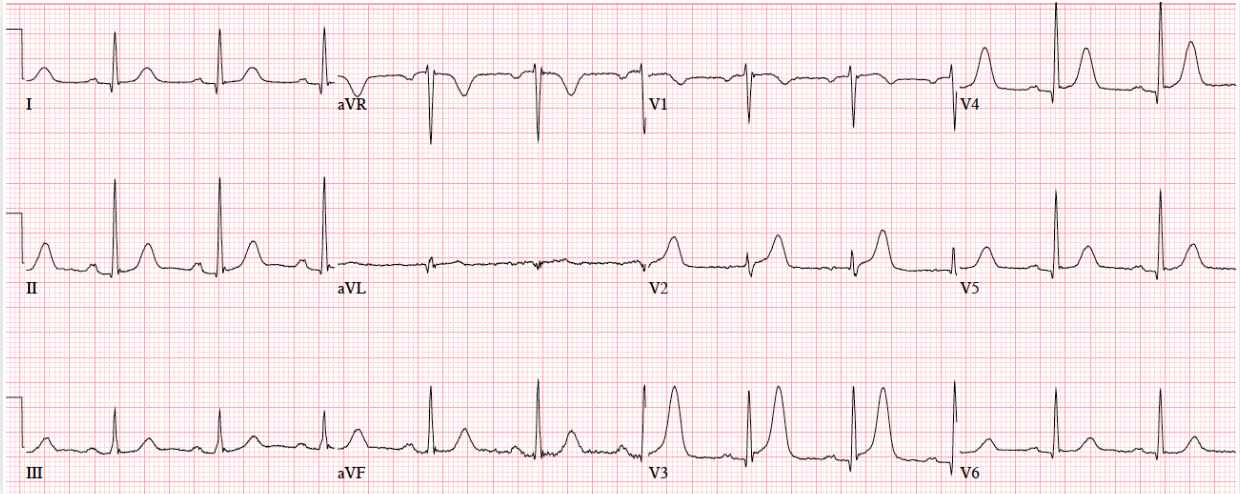
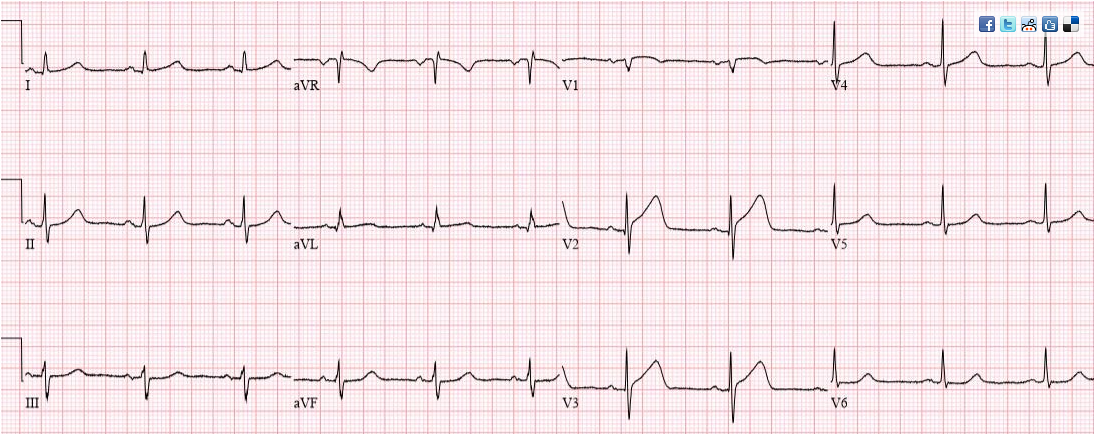
Patient 2: 50yo with 3hrs of mid-sternal squeezing chest pain with diaphoresis. No prior ECG
Answers To Patient 2: ischemic T wave morphology
My Answer: Left axis deviation. T wave inversion in aVL.
Blog Answer: Ischemic T wave morphology.
NSR, normal conduction/axis/R wave, no hypertrophy. No ST segment elevation or depression, but there is terminal T-wave inversion in aVL and reciprocal down-up T waves in III/III/aVF, and inverted U wave in V2-3. The physician was concerned about these and asked for a repeat ECG:
My Answer: Forgot to interpret this ECG before I looked at the answer.
Blog Answer: Now there is ST elevation in V1-2 and aVL, a deeper Q wave in aVL and new Q wave in V2, and ST depression inferolaterally. Code STEMI called: 95% proximal LAD occlusion
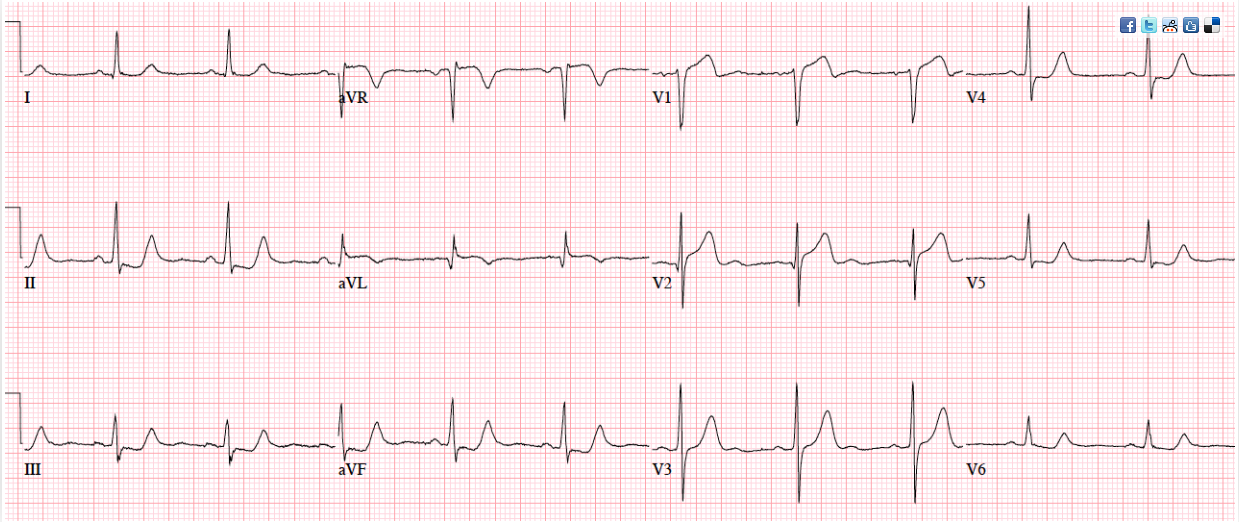
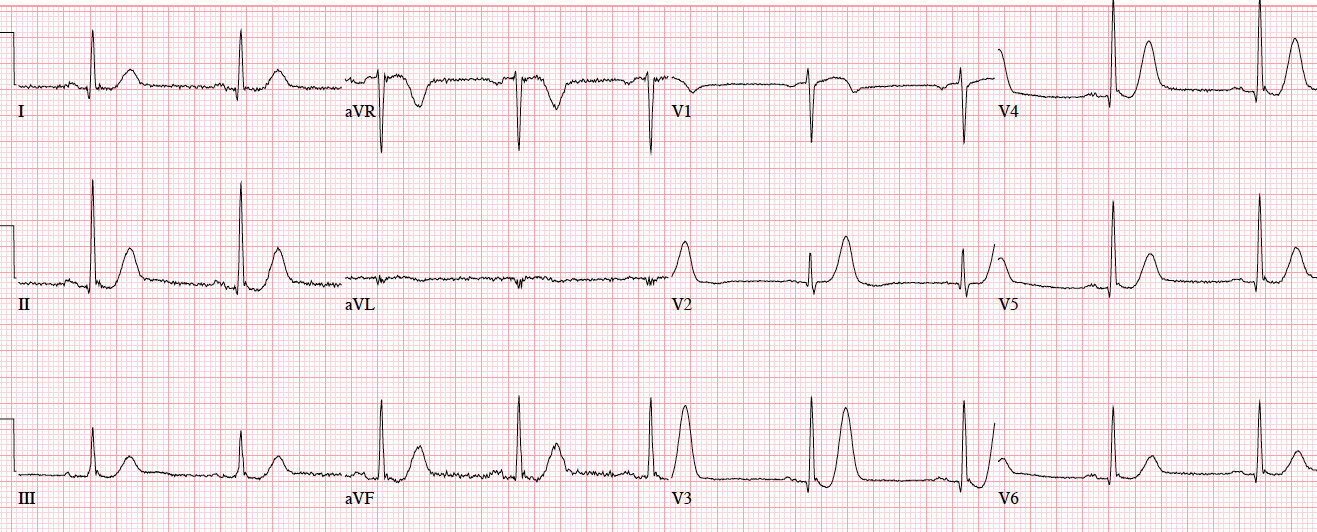
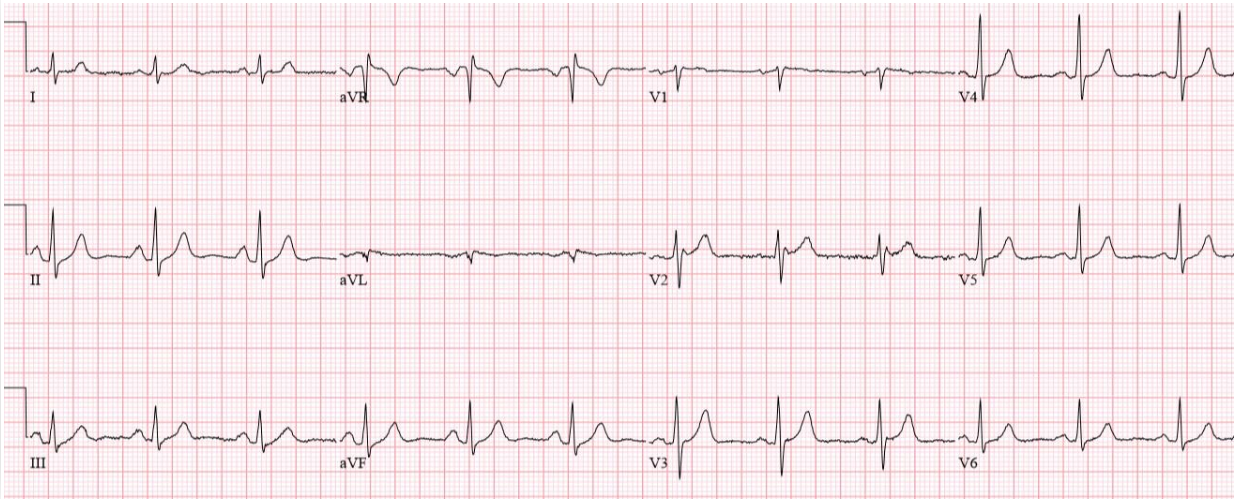
Patient 3. 70yo with 90 minutes exertional chest pain and nausea. No prior ECG
Answers To Patient 3. Subtle LAD occlusion
My Answer: ST elevation in V1-V6
Correct Answer: NSR, normal conduction/axis, no hypertrophy.There is 1-2mm concave ST elevation in V2-3 which could be normal, but there are a number ischemic changes: reverse R wave progression from V2 to V3, Q wave in V2, terminal QRS distortion (no S wave or J wave) in V2, hyperacute T waves (relative to their preceding QRS) in V2-3, and inferior reciprocal changes. When trop came back positive an hour later, a repeat ECG was done:
Now there is a full QS wave in V2. Code STEMI called: 100% mid-LAD occlusion.
Patient 4: 70yo with one hour of exertional chest pain radiating to the arm. Old then new ECG
Answers To Patient 4: Subtle LAD Occlusion
My Answer:
Old ECG: NSR/NQXR ais/No hypertrophy/No ST Abnormalities/Normal
New ECG: NSR/NQRS/Terminal T wave inversion in V1/Tall peaked T waves in V2 + V3/ST elevation in V3 – V6
I would activate the cath lab.
Blog Answer:
NSR, normal conduction/axis/R wave progression, no hypertrophy. Compared to the old ECG there is no ST elevation, but there are three other signs of occlusion: hyperacute T waves (now bigger than the R wave in V2 and as big as the R wave in V3), a deeper Q wave in V3, and terminal QRS distortion in V3. Physician asked for a repeat ECG:
Read by the machine as “nonspecific”, but the deWinter T waves in V3-4 (ST depression followed by tall symmetric T waves) are very specific for LAD occlusion. Cath lab activated: 100% mid-LAD occlusion. First trop negative, peak 50,000.
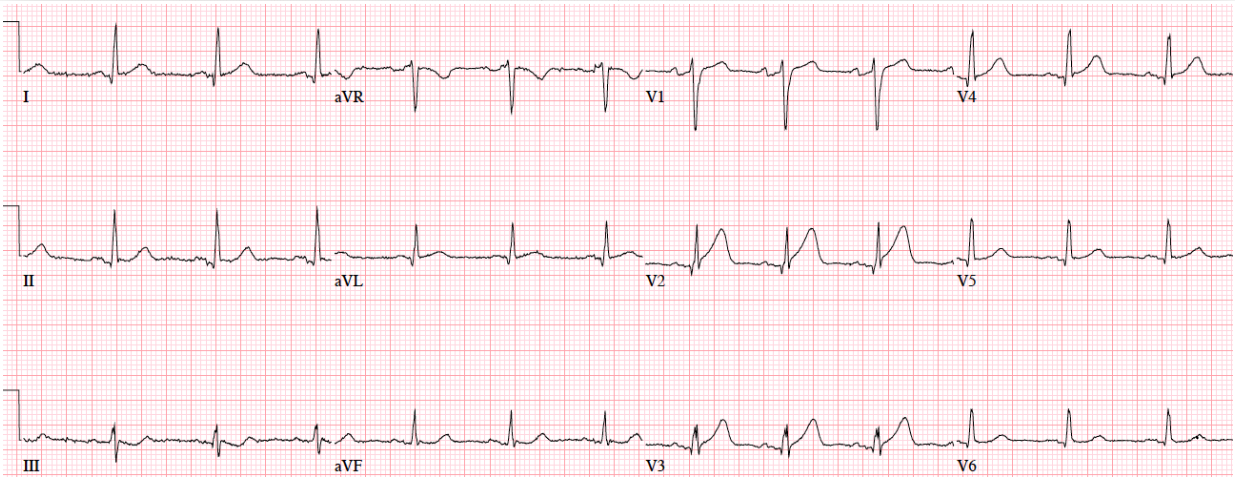
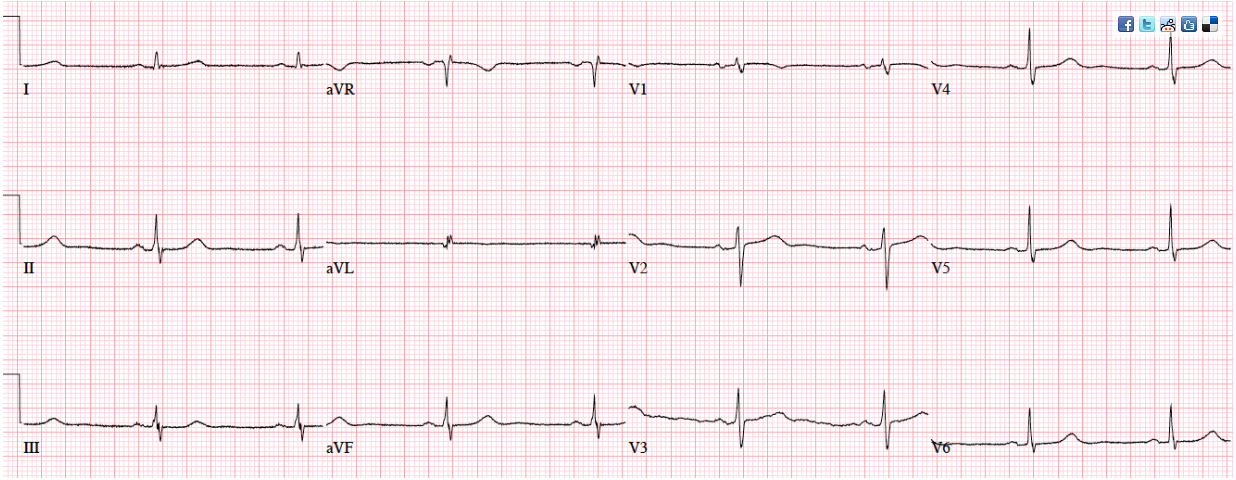
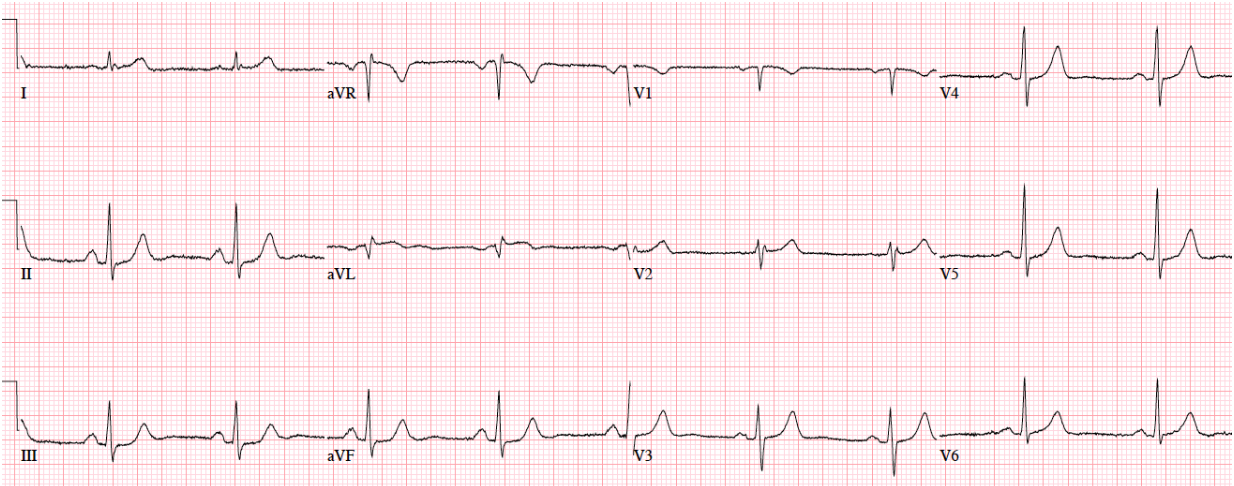
Patient 5: 70yo with 6hrs on/off chest tightness radiating to the arm now constant. Old then new ECG
Answers to Patient 5: ST/T changes compared to prior
My Answer:
Old ECG: Sinus Bradycardia/N QRS axis/No Hypertrophy/No ST-T Changes/Normal ECG
New ECG: SB/N QRS axis/ST elevation in V2 + V3/Hyperacute T waves in V2 + V3
Blog Answer:
There’s mild concave ST elevation in lead V2-3 which doesn’t meet STEMI criteria. But this is new compared to previous, along with hyperacute T waves in V2-3 and mild ST depression laterally. When trop came back positive an hour later, repeat ECG below showed straightening of the ST segments, and the cath lab was activated: 100% distal LAD occlusion.
Patient 6: 75yo one day chest pain radiating to bilateral shoulders. Old then new ECG
Answers to Patient 6:
Patient 7: 55yo history RCA stent with 30 minutes chest pain radiating to the arm. Old then new ECG