The correct technique of ECG recording is critical to the accurate interpretation of the 12 lead electrocardiogram.
This post contains excerpts from the 2017 Recording a Standard 12-Lead Electrocardiogram – An approved method by the Society for Cardiological Science & Technology (SCST):
2. Introduction
The resting 12-lead electrocardiogram (ECG) is an important first line investigation that records the electrical activity of the heart. This investigation can aid the diagnosis and help define the appropriate patient treatment pathway in a range of cardiac conditions, many of which are life threatening and require immediate action.
ECGs not performed to appropriate standards can result in incorrect diagnoses and inappropriate treatments1-7. There are many personnel recording ECGs who have not been
properly trained or assessed8 . Personnel may consider themselves competent9, 10, despite a lack of training, and yet lack essential knowledge in ECG recording technique that results in incorrect ECG recording11-14.Evidence indicates that appropriate training leads to fewer ECG recording errors15. . . . SCST recommends that all personnel who record ECGs are appropriately trained, assessed and qualified.
These guidelines provide essential information pertinent to the correct ECG recording technique in keeping with good scientific practice16. They are written by expert practitioners following critical evaluation of published evidence. Where evidence was limited a consensus decision was made.
5.1 Patient position
Many patients are uncomfortable lying flat, so for consistency and practicality, a semi-recumbent position of approximately 45 degrees is recommended. Any significant variation from this position should be documented on the ECG recording. The limbs should be supported by the bed/couch to minimise artefact due to muscle tension. The ECG appearance can be affected by the angle of incline of the torso at the time of recording. An ECG recorded from a patient in a supine position may vary significantly from one recorded with the patient in an upright position19, 20 or inclined at 60 degrees or greater to the horizontal21. There is no evidence that variation of the inclination of the patient between horizontal and 45 degrees
to the horizontal has any significant effect on the ECG.[However, despite the above, I will record my office ECGs in the supine position unless the patient is uncomfortable supine.]
Time should be taken to ensure that the patient is relaxed and comfortable. If these conditions are not satisfied the ECG may record somatic muscle potentials as well as cardiac activity and will make the ECG more difficult to interpret and potentially limit clinical value. Some patients cannot relax fully because of painful conditions such as arthritis, or they may have a condition such as Parkinson’s disease which causes a tremor. These patients should be made as comfortable as possible and the ECG trace annotated with an
explanation if it is suboptimal quality. Before recording the ECG, checks should be made to ensure the patient’s limbs are still and appear relaxed. If the patient has clenched fists or stiff arms or is moving his/her fingers, it will not be possible to obtain a high-quality ECG.5.2 Skin preparation
Skin preparation is often required to help produce an artefact-free ECG. Care must be taken with patients who have sensitive or broken skin.
6. Electrode placement
Electrodes must be positioned in accordance with AHA recommendations22-24.
If any of the electrodes are to be sited in non-standard positions the recording must be labelled with this information to avoid misinterpretation of altered ECG waveforms24-28.
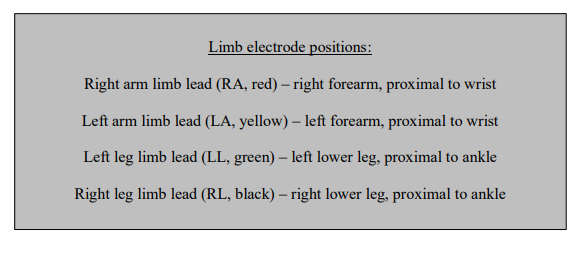
6.1 Limb electrode positions
Limb electrodes should be placed proximal the wrists and ankles whenever possible. Moving the electrodes up the limbs may alter the appearance of the ECG and should be avoided unless there is a significant tremor or a limb has been amputated.
Note: Limb electrodes must not be placed on the torso since this causes significant alteration to wave amplitudes. This can invalidate the use of the recording for many diagnostic purposes25, 29.
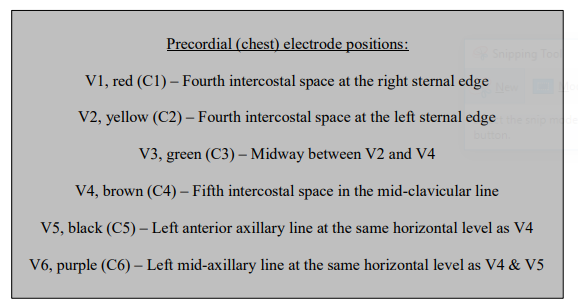
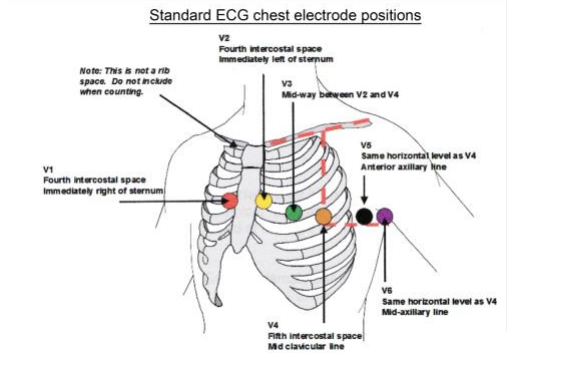
6.2 Precordial (chest) electrode positions
The correct anatomical positions for the chest electrodes have been defined22 (see figure below) and must always be used unless access is not possible. The centre of the active area of the electrode should be aligned with the relevant anatomical landmark.
Studies have demonstrated that the V1 and V2 electrodes are frequently placed too high and the V4, V5 and V6 electrodes too low13, 30, 31, 32. These errors can result in diagnostically misleading alterations to the ECG waveform33.
6.3 Technique for locating chest electrode positions
Accurate identification of the appropriate intercostal spaces should begin with location of the manubriosternal joint, also known as the angle of Louis.
• To locate the angle of Louis a finger should be run down the sternum from the top until a bony horizontal ridge is met. Sliding the finger down and to the right side will locate the second intercostal space. From here it is possible to count down to the third and fourth intercostal spaces. In the
fourth space, the finger should be slid towards the sternum until the edge is felt. This is where the centre of the V1 electrode should be placed.• This procedure should be repeated on the left side to correctly position the V2 electrode. (Note that the left and right sided rib spaces may be offset, so practitioners should avoid placing V2 adjacent to V1 without counting the rib spaces).
• Next, the V4 electrode should be placed in the 5th intercostal space in line with the mid-point of the clavicle.
• The V3 electrode should then be placed mid-way between the V2 and V4 electrodes.
• The V5 and V6 electrodes should then be positioned in horizontal alignment with the V4 electrode. The V5 electrode should be placed on the anterior axillary line; the V6 electrode should be placed on the mid-axillary line.
When recording an ECG from female patients it is convention to place the V4, V5 and V6 electrodes beneath the left breast when breast tissue overlies the correct anatomical positions. There is some evidence to suggest that the positioning of these electrodes over the breast may not significantly attenuate the signal33, 34 but further supporting evidence is needed to warrant a change in this recommendation.
When lifting the breast to place electrodes, care and sensitivity is required.
Using the back of the hand to lift the breast can be helpful in minimising contact.
To achieve accurate ECG electrode positioning, it is usually necessary for all upper torso clothing to be absent.
Note: If positioning varies from the recommended positions it is essential that this is documented on the ECG recording, including electronically stored ECGs.
7. Obtaining a good quality recording
A 12-lead ECG and simultaneous rhythm strip is most commonly recorded at 25mm/s with a gain setting of 10mm/mV. The appropriate button should be pressed to initiate a recording; this is usually labelled as ‘start’ or ‘auto’.
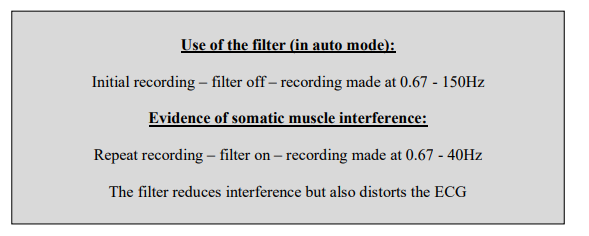
All filters should be ‘off’ for the initial attempt to record an ECG. The low-pass filter will reduce interference but it also distorts the ECG35, so should only be used when necessary and only after all attempts to eliminate the interference have failed.
If, despite efforts to relax the patient and make them comfortable, there is somatic muscle interference on the ECG, the filter may be switched on and the recording repeated. Use of the filter should be clearly identified on the final ECG.
Any features on the ECG that might indicate the need for urgent medical attention should be brought to the attention of appropriate staff. If the patient has any symptoms of possible cardiac origin, such as chest pain, palpitations or dizziness, at the time of recording, then this should be noted on the ECG.
Confirmation that an ECG of good quality has been recorded should be made by the practitioner. The recording should be assessed to ensure that all waveforms (such as P waves, QRS complexes and T waves) are clearly visible. The isoelectric line (the baseline between ECG deflections) should be stable, not wandering, and free of interference
At the end of the procedure, all the electrodes should be removed from the patient and disposed of as clinical waste.
Note: Incorrectly pressing ‘copy’ or ‘reprint’ may on some models of ECG machine initiate a printout of an ECG from a previous patient36. If patient details are not entered into the machine it may not be clear that this ECG relates to a previous patient. Practitioners must fully understand the equipment they are using and the potential consequences of mistakes. Local practice guidance must minimise the chance of an identity or recording error occurring in this way.
7.1 Variation from standard
start here