In this post I link to and excerpt from “Post-Intubation Care” from Emergency Medicine Cases‘ EM Quick Hits 26 LAST, Sodium Nitrite Poisoning, Post-intubation Care, Tetracaine for Corneal Abrasion, ST Segment in Occlusion MI, Coping with COVID.
Helman, A. Swaminathan, Austin, E. M. Rosenberg, H. Rezaie, S. MacLaren, J. Maunder, R. EM Quick Hits 26 – LAST, Sodium Nitrite Poisoning, Post-intubation Care, Tetracaine for Corneal Abrasion, ST depression, Coping with COVID. Emergency Medicine Cases. February, 2021. https://emergencymedicinecases.com/em-quick-hits-february-2021/. Accessed 5-28-2021.
All that follows is from “Post-Intubation Care”:
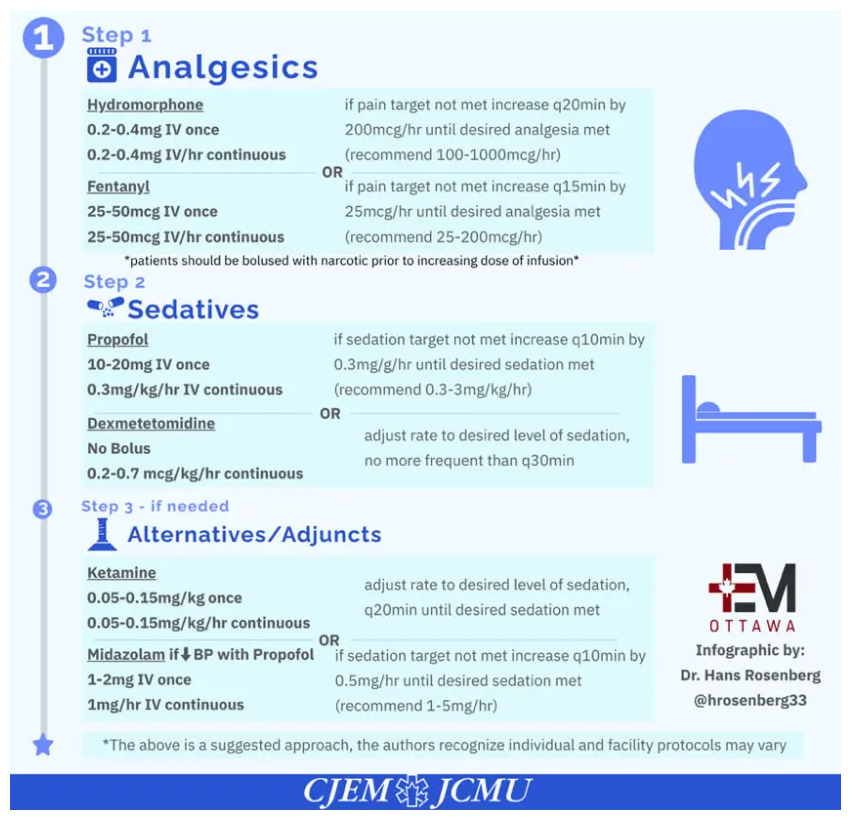
Post-intubation sedation and analgesia
- Under-treatment or over-treatment of pain and agitation of the post-intubation patient in the ED may increase the likelihood of the patient developing acute delirium, which has been associated with an increased mortality rate in ICU patients suffering from severe sepsis or septic shock and may prolong ICU stay
- For patients who are aggressively attempting to pull out their ETT and require immediate sedation and analgesia, consider Ketamine 0.7mg/kg IV (approx. 50mg IV), then 0.15-0.25mg/kg q5-10 mins prn titrated to effect.
- Benzodiazepines may increase the incidence of delirium and prolong the time on the ventilator, and so are not favored as a first line for sedation; if you choose to use benzodiazepines, be sure to control pain first with fentanyl before any benzodiazepine is administered, and use small doses (eg: 1-2mg Midazolam)
Reference:
- Rosenberg H, Hendin A, Rosenberg E. Just the Facts: Postintubation sedation in the emergency department. CJEM. 2020 Nov;22(6):764-767. [PubMed Abstract] [Full Text PDF].
Here are excerpts from the above article:
CLINICAL SCENARIO
A 67-year-old male presents to the emergency department (ED) in respiratory distress secondary to pneumonia. His
oxygen saturation is 86% on a nonrebreather, respiratory rate is 32 respirations/minute, blood pressure 147/72 mmHg,
heart rate 121 beats/minute, and temperature is 38.7° Celsius. The decision is made to intubate the patient. Fentanyl
and propofol are used for analgesia and sedation, and rocuronium is used for paralysis. Using video laryngoscopy, the
patient is successfully intubated, and now the ED team is awaiting your orders for the postintubation sedation care of
this patient.CASE RESOLUTION
The patient is started on a fentanyl infusion at a set rate, which is then titrated using the Behavioural Pain
Scale once rocuroniumhas worn off. In addition, a propofol infusion is started and titrated using the Richmond
Agitation Sedation Scale. The patient appears comfortable, can respond to commands, and remains
hemodynamically stable. The intensive care team arrives in the ED, and the patient is safely transported to
the ICU.KEY POINTS
1. Intubated patients frequently experience both pain and anxiety, which should be treated first with analgesia,
and then with sedatives if required.
2. While emergency physicians are now more cognizant of the need to provide analgesia and sedation post intubation, some patients still are under-treated in the ED.
3. Inadequate sedation as well as very deep sedation both have adverse physiologic consequences and negatively
impact patient outcomes.
4. Emergency physicians must ensure that patients receiving long-acting neuromuscular blockade are administered sedation until the paralytic is expected to have worn off.
5. Opioids should be used along with multi-modal analgesia to manage pain. Propofol is preferred for sedation
over benzodiazepines, which have been shown to prolong duration of mechanical ventilation and ICU stay.
6. Validated scales for assessing pain and degree of sedation in the intubated patient should be used to titrate
medication dosing.5. How can we measure pain and sedation in intubated patients to adjust analgesic and sedative doses?
Critically ill patients are often unable to easily communicate due to altered mental status, mechanical ventilation, and
other invasive devices that can limit mobility and speech. Analgesics and sedatives all have side effects, and so the desire
is always to use the lowest possible dose for the shortest amount of time. In keeping with the Society of Critical Care
Medicine recommendation for an assessment-driven approach to pain and sedation management, there is a clear need
for validated pain and sedation assessment tools.The gold standard for pain assessment is patient self-report using the numeric rating scale from 0 to 10; however, intubated patients are not always able to do this.
Two pain assessment tools developed for and validated in critically ill mechanically ventilated patients are the Critical Care Pain Observation Tool and the Behavioural Pain Scale.
Sedation can be assessed using either the Richmond Agitation Sedation Scale or the Sedation-Agitation Scale. A light level of sedation is the desired goal, with patients who are ideally alert and calm, or mildly sedated but easily roused. Light sedation is associated with shorter duration of mechanical ventilation and reduced rate of tracheostomy