Today I review some of my past neurocritical care post resources
Links To And Excerpts From EMCrit 275 – NeuroCritical Care with Dr. Neha Dangayach
Posted on April 3, 2021 by Tom Wade MD
Here is the direct link: EMCrit 275 – NeuroCritical Care with Neha Dangayach. by
The show notes are outstanding. However, the podcast itself should be reviewed over and over. The lecture has much more than just the great show notes. Here are excerpts from the show notes:
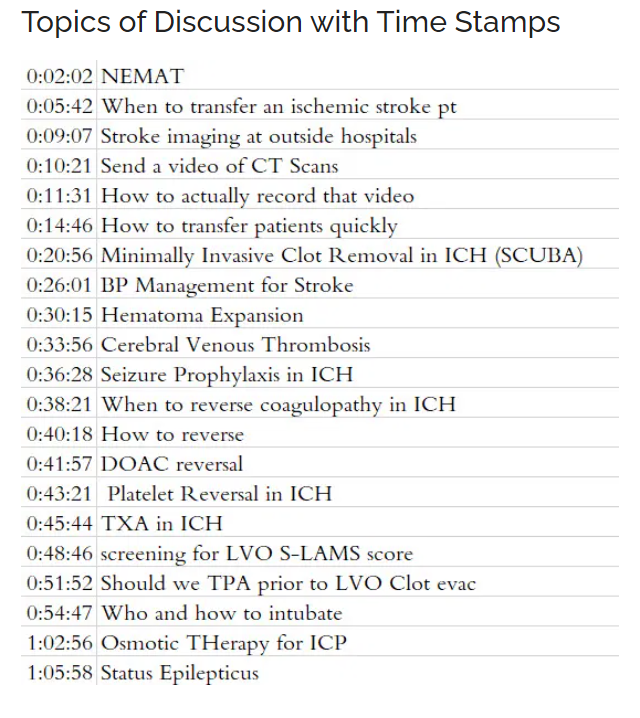
Dr. Nagayach’s Slides
Neuro-Emergency Management and Transfer (NEMAT) Service
ELVO = Emergent Large Vessel Occlusion. Often called simply LVO (Large Vessel Occlusion) in other resources.
When Do We Need Continuous EEG Monitoring in Critically Ill Adults And Children? Posted on July 8, 2018 by Tom Wade MD
Here are the references in the above resource:
(1) Management of Status Epilepticus in Children [PubMed Abstract] [Full Text HTML] [Full Text PDF]. J Clin Med. 2016 Apr; 5(4): 47
(2) Consensus statement on continuous EEG in critically ill adults and children, part I: indications [PubMed Abstract] [Full Text HTML] [Full Text PDF]. J Clin Neurophysiol. 2015 Apr;32(2):87-95. doi: 10.1097/WNP.0000000000000166.
(3) Consensus statement on continuous EEG in critically ill adults and children, part II: personnel, technical specifications, and clinical practice [PubMed Abstract] [Full Text HTML] [Full Text PDF]. J Clin Neurophysiol. 2015 Apr;32(2):96-108. doi: 10.1097/WNP.0000000000000165.
Stroke And TIA – Help From MCHD Paramedic Podcast, EMC Podcast, And emedicine.medscape.com
Posted on March 12, 2019, by Tom Wade MD
Here are direct links to the resources referenced in the above post:
MCHD Paramedic Podcast – Episode 9 – The State Of EMS Stroke Care In 2018
MCHD Paramedic Podcast – Episode 10 – Stroke Systems Of Care Featuring Dr. Peter Antevy
Hermes Collaboration: Lancet 2016
www.thelancet.com/journals/lancet/…00163-X/abstract
Dawn Trial: NEJM 2018
www.nejm.org/doi/full/10.1056/NEJMoa1706442
DEFUSE 3 Trial: NEJM 2018
www.nejm.org/doi/full/10.1056/NEJMoa1713973
TIA Diagnosis And Management, Episode 117 From Emergency Medicine Cases – With Additional Resources
Posted on November 23, 2018 by Tom Wade MD
Ep 120 ED Stroke Management in the Age of Endovascular Therapy. Podcast production, sound design & editing by Anton Helman. Written Summary and blog post by Anton Helman, January 2019
According to the Global Burden of Disease Study published in NEJM in December 2018 the estimated lifetime risk for a 25 year old during their remaining lifespan is 25% [1]. Stroke is the 3rd leading cause of death and 1st leading cause of major disability in North America. As we transition from the relatively simple era of systemic thrombolytics under 3 hours vs “ASA and admit” for over 3 hours, decision making has become much more complicated and varied, depending on where you work. Which patients need what type of scanning? Where should that scanning be done – at the stroke center or at the peripheral center? Which patients should get systemic thrombolytics? Which patients should get endovascular therapy? In this EM Cases main episode podcast, a follow up to our episode on TIA released in November 2018 with Walter Himmel and David Dushenski, we try to simplify the confusing time-based and brain tissue-based options for stroke management…
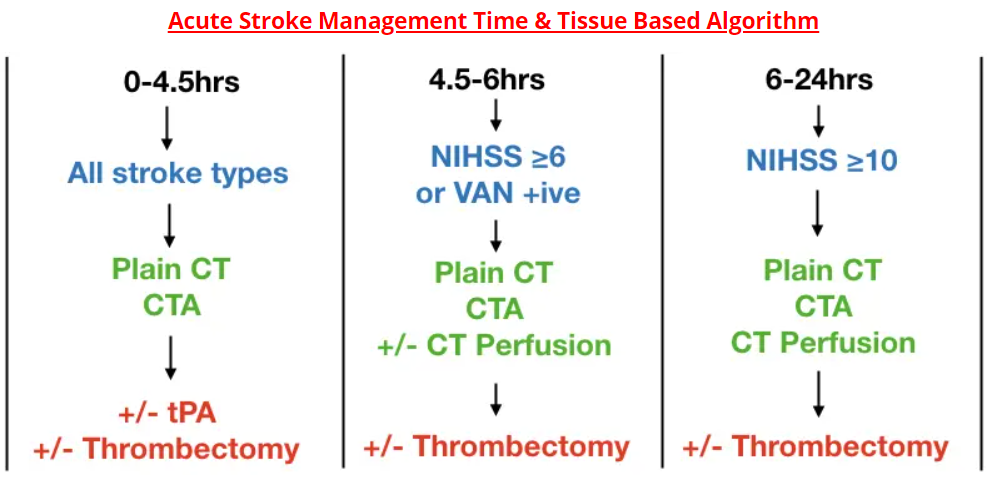
Time and image based stroke management algorithm
Activating a “code stroke” on every patient that experiences any acute neurologic event within 24hrs of symptom onset based on the DIFFUSE 3 and DAWN trials [2,3] may outstrip resources, with only a tiny minority of these patients receiving potential benefit. There is currently an effort to identify those patients clinically who might be most likely to benefit from endovascular therapy so that not all stroke patients require transport to a stroke center with multiple imaging modalities and resource-heavy acute stroke team care.
The workup and considerations for tPA and endovascular therapy (thrombectomy) depend on:
- Symptom onset to needle time
- Type of stroke, NIHSS or VAN tool (see below)
- CT, CT angiogram and CT perfusion results
- Contraindications to tPA/thrombectomy
Time is the key factor in patients with a symptom onset-to-needle time ≤ 6 hours.
Brain tissue salvageability determined by CT perfusion is the key factor in patients with a symptom onset-to-needle time of 6-24 hours.
Times are symptom onset to needle times at a stroke center. CTA= CT angiogram head and neck. NIHSS = National Institute of Health Stroke Scale. VAN = Vision, Aphasia, Neglect tool. NIHSS on MD Calc
In the 0-4.5 hours category, plain CT will rule in hemorrhagic stroke and CTA may diagnose an underlying vascular abnormality causing the bleed.
For patients in the 4.5-6 hours category, and with an NIHSS ≥6 or VAN positive, and plain CT and CTA consistent with cortical stroke, candidacy for thrombectomy is determined either by CT perfusion, or if CT perfusion is not readily available, by the ASPECTS score[6].
VAN Tool to identify large vessel cortical strokes
Patient must have weakness plus one or all of the V, A, or N to be VAN positive.
Step 1: Weakness
Weakness – ask the patient to raise both arms up for 10 seconds and assess for drift, weakness or paralysis; if any of these are present proceed to step 2
Step 2: V or A or N
Visual disturbance – field cut, diplopia or blindness
Aphasia – expressive (repeat and name 2 objects) or receptive (unable to follow commands – close eyes or make a fist)
Neglect – inability to track to one side, ignoring one side, unable to feel both sides at the same time or unable to identify own arm
Medications for stroke patients who do not fulfill criteria for tPA or endovascular therapy
There is no role for dual antiplatelet therapy in completed stroke, unless the NIHSS ≤3 and CT or MRI show a small area of hypodensity < 1-2 cm diameter (very minor stroke). Starting with the CAST trial in 1997 and based on two more recent meta-analyses in 2012 and 2013, the risk of hemorrhagic transformation outweighs any potential benefit in most patients with completed stroke [8,9,10].
There is no role for starting anticoagulant medications in the ED for patients with history of atrial fibrillation or who present with atrial fibrillation at the time of their stroke. Again, the risk of hemorrhagic transformation outweighs any potential benefit of starting anticoagulants in the acute phase.
The risk of recurrent stroke in patients with atrial fibrillation is approximately 2% per week for the first two weeks after a stroke [4].
At what time after a stroke should patients with atrial fibrillation be started on anticoagulants? Expert opinion consensus suggests that for patients with atrial fibrillation and:
- Large size stroke, anticoagulation should be considered starting on day 10.
- Medium size stroke, anticoagulation should be considered starting on day 5-7.
- Small size stroke, anticoagulation should be considered starting on day 3-5.
Note to myself: Be sure to review the rest of the show notes of the outstanding EMC Episode 120 Stroke Management In The Age Of Endovascular Therapy.
Link To The Core EM podcast Episode 175.0 – Posterior Circulation Stroke With An Additional Resource On The HINTS Exam
Posted on July 8, 2020, by Tom Wade MD
Link To And Excerpts From “Ischemic stroke” From Radiopedia
Posted on March 14, 2021, by Tom Wade MD
Emergency Medicine Cases Ep 104 Emergency Management of Intracerebral Hemorrhage – The Golden Hour. Podcast production, sound design & editing by Anton Helman. Written Summary and blog post by Anton Helman December, 2017
There exists a kind of self-fulfilling prognostic pessimism when it comes to ICH. And this pessimism sometimes leads to less than optimal care in patients who otherwise might have had a reasonably good outcome if they were managed aggressively. Despite the poor prognosis of these patients overall, there is some evidence to suggest that early aggressive medical management may improve outcomes. As such, the skill with which you manage your patient with ICH in those first few hours could be the most important determinant of their outcome. In this Golden Hour you have a chance to prevent hematoma expansion, stabilize intracerebral perfusion and give your patient the best chance of survival with neurologic recovery. In this podcast, the Weingart-Himmel Sessions Redux, we answer questions such as: Should we attempt to manage blood pressure before ICH is confirmed on CT? What are the best drugs to manage blood pressure in ICH? What is the role of POCUS in emergency management of intracerebral hemorrhage? How do we best reverse the effects of anticoagulants and lytics in ICH patients? Are prophylactic antiepileptic drugs ever indicated in ICH in the ED? How do we best risk stratify patients with ICH? What are the indications for neurosurgical intervention? How do we determine if a patient with ICH has elevated ICP and how do we best manage it in the ED? What are the key elements of a neuro-critical care intubation? What is the preferred hyperosmolar agent for elevated ICP? and many more…