In this post, I link to and excerpt from The Curbsiders‘ #314 When the Flow Won’t Go: Constipation with Dr. Iris Wang. JANUARY 3, 2022 By DR ELENA GIBSON.
All that follows is from the above outstanding resource.
Summary
Move smoothly through constipation evaluation and management. Learn how to evaluate for the various etiologies of constipation including pelvic floor dysfunction, IBS-C and more with our esteemed guest Dr. Xiao Jing (Iris) Wang @IrisWangMD!
Show Segments (Note: time stamps are without ads)
- Intro, disclaimer, guest bio
- Guest one-liner, Picks of the Week* (6:00)
- Case from Kashlak; Definitions (11:00)
- Physiology of a bowel movement (10:00)
- Definitions (16:00)
- Bowel Habit Review of Systems (17:00)
- Rectal Exam (33:00)
- Initial Constipation Evaluation
- Common categories of constipation (43:40)
- Additional evaluation of Constipation (52:00)
- Treatment options (1:10:00)
- Outro
Constipation Pearls
- The physiology of producing a bowel movement requires 3 phases described as “Ready, Set, Go.”
- Constipation includes symptoms of decreased stool frequency, incomplete evacuation, changes in stool consistency, and difficulty with defecation.
- Straining, incomplete evacuation and manual disimpaction are signs/symptoms associated with rectal evacuation disorders.
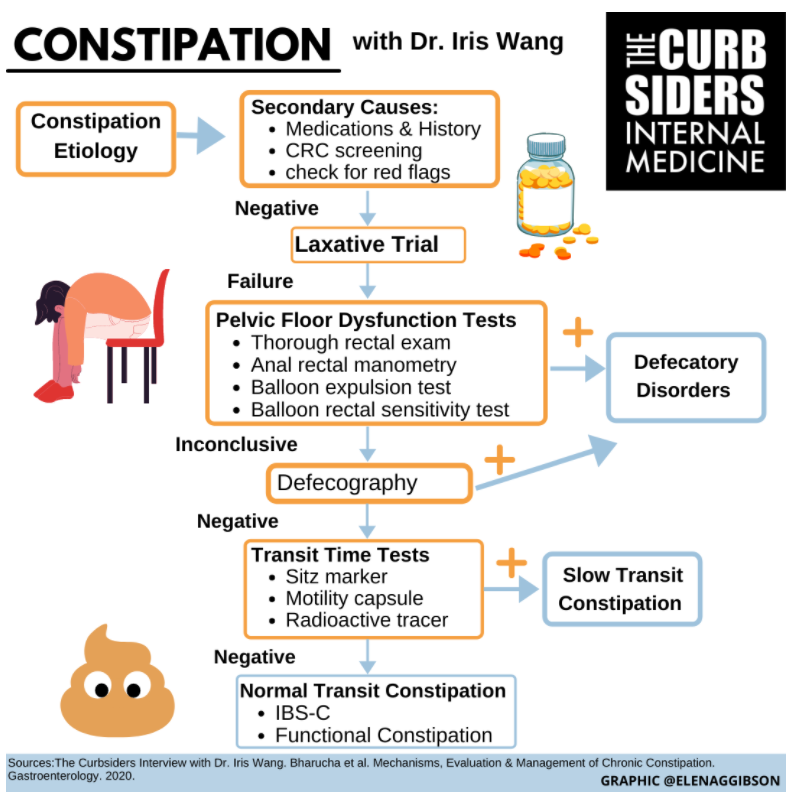
- After ruling out secondary causes of constipation, a laxative trial is indicated before pursuing further evaluation of a pelvic floor disorder or slow transit constipation.
- If a laxative trial is unsuccessful, the next evaluation step in constipation is evaluating for pelvic floor dysfunction with anal rectal manometry and a balloon expulsion test.
- If testing for pelvic floor dysfunction is inconclusive, defecography should be performed to evaluate for prolapse or obstruction.
- Evaluation for abnormal colonic transit time should only be completed after an evaluation for pelvic floor dysfunction is negative.
- Two kiwis or four prunes a day are recommended as examples of dietary insoluble fiber.
- Common enemas are similar in efficacy, and potential side effects can be used to guide selection.
- Biofeedback is the most effective treatment for pelvic floor dysfunction.
When the Flow Won’t Go
Definitions and Diagnoses
To produce a bowel movement:
- Ready (predefecatory phase): The body prepares to have a bowel movement by increasing the frequency and amplitude of colonic contractions. The gastrocolic reflex is activated and this triggering allows the colon to prepare for food coming from above.
- Set: Stool reaches the rectum. Stool stimulates receptors in the upper anal canal. This leads to the urge to defecate or resist defecation. When defecation is resisted, there is a signal sent back through your colon to increase colon transit time and delay movement.
- Go: Most people do this effortlessly. Rectal pressure is generated by contraction of the diaphragm + abdominal muscles leading to increased rectal pressure & the pelvic floor simultaneously relaxes.
Constipation
Constipation includes symptoms of decreased stool frequency, incomplete evacuation, changes in stool consistency, and difficulty with defecation. Constipation is formally diagnosed as 3 or fewer bowel movements per week and chronic constipation occurs when symptoms persist for 3 consecutive months.
Initial Evaluation: History & Physical
“Bowel Habit Review of Systems”
1. Start with baseline: Frequency of stools—what was your baseline what was normal for you and what is it now?
2. Bristol stool form: On a 1-7 scale visual idea of softness of bowel movement, 1 to 2 is a hard bowel movement by definition though changes may be relative to baseline
3. Ask about warning signs including weight loss, change in stool caliber (especially sudden onset change), severe pain & rectal bleeding.
4. Do you strain when you have a bowel movement?
5. Sensation of incomplete evacuation or feeling like you just had a bowel movement and there is still more stool present?
6. Do you need to shift positions on the toilet? Are you doing “toilet yoga”?
7. Do you ever use a finger to help the stool come out (manual evacuation)?
8. For females: Do you need to splint the back wall of the vagina? If so, concern for pelvic organ prolapse or rectocele.
**From #4 on, these questions are used to evaluate rectal evacuation disorders
Physical Exam
Full head to toe physical exam to evaluate for evidence of upper neuron disorders or systemic disease. Listen to bowel sounds to know if hypoactive or hyperactive. Palpate LLQ because sometimes you can actually feel the stool.
Rectal Exam
A thorough rectal exam has a sensitivity of 93% and a PPV of 91% compared to your anal rectal manometry and balloon expulsion studies (Bharucha 2020). Dr. Wang recommends describing the rectal exam in detail with patients prior to completing.
- Begin by evaluating around anal canal for evidence of chronic constipation (ie. skin tags, fissures, hemorrhoids, fistula).
- Ask the patient to squeeze like holding in a bowel movement and look for contraction of anal sphincter vs gluteal muscles (eval for incontinence issues)
- Ask to push out & look for sphincter relaxation or contraction (relaxation is normal). Evaluate how far the perineum descends (normal ~1-3cm).
- During the digital exam check for anal wink to make sure sacral nerves are intact and use your finger to assess rectal tone. Repeat the above maneuvers (squeeze and push out) up to 3 times each. During these maneuvers, Dr. Wang describes wrapping your finger around the puborectalis to check for tenderness and relaxation movement away from the umbilicus when asked to expel the finger.
Etiologies of Constipation
There are three categories of constipation: 1) Normal transit constipation (IBS-C & functional constipation), 2) Slow transit constipation (diminished gastrocolic reflex & neuronal or muscular tissue disorders), 3) Defecatory disorders (pelvic floor dysfunction, prolapse).
Stepwise evaluation of constipation
The evaluation of chronic constipation (usually outpatient) should be completed by first evaluating for secondary causes of constipation. If there is no secondary etiology, a trial of laxatives is recommended (Bharucha 2020).
- Evaluate for secondary causes of constipation
- Medications
- Medical history, including psychiatric and obstetric history
- Labs: electrolytes
- Red flags & age-appropriate CRC screening
- Trial of Treatment (fiber & laxative therapy)
If the treatment trial is not successful then evaluate for the underlying constipation phenotype with the following (Bharucha 2020):
Additional Testing (Lembo 2003)
- Evaluate for pelvic floor dysfunction*,**
*Please see INDIANA UNIVERSITY HEALTH GI MOTILITY LAB & GASTRIC ELECTRICAL STIMULATION PROGRAM: ANORECTAL MANOMETRY AND COMPLIANCE TESTING
**Important to look for pelvic floor dysfunction first because it can slow down bowel transit by causing rectal distention that signals slowing of small bowel and colon transit
- Anorectal manometry: Probe with sensors in rectum for measuring rectal, anal pressure, and the gradient with evacuation & squeezing to avoid evacuation.
- Balloon expulsion test: Balloon is placed in rectum & filled with 50cc of water and patients are asked to evacuate the balloon. If they are unable to evacuate the balloon within a certain amount of time that is a rectal evacuation disorder. This is the most sensitive test.
- Balloon rectal sensitivity test: A balloon is placed in the rectum to evaluate for hypersensitivity of the rectum by measuring the volumes that cause sensation of the balloon, an urge to defecate and discomfort.
**Important to look for pelvic floor dysfunction first because it can slow down bowel transit by causing rectal distention that signals slowing of small bowel and colon transit
- If evaluation for pelvic floor dysfunction is inconclusive→Defecography: Imaging studies of what occurs with evacuation of rectal content to look for prolapse or obstruction
- If inconclusive, then evaluate for abnormal colonic transit with one of the following:
- Sitz marker study: Capsules of radiopaque markers swallowed and radiographs are taken at day 0, day 1, day 5 etc to evaluate for transit of markers within the bowel and colon. The number of markers remaining and the pattern of marker location can be roughly used for diagnostics. If evenly distributed->diffuse slow transit. If all markers sitting in descending colon, sigmoid, rectum-> undiagnosed pelvic floor dysfunction.
- Motility capsule: Sends signals of location (based on metrics like pH, temperature) while moving through bowel
- Nuclear Medicine Scintigraphy (Radioactive tracer): Look at where tracer goes 0, 4, 24 and 48 hours. Can tell where stool gets stuck (similar to sitz).
Treatment
Fiber is first-line treatment and Dr. Wang recommends soluble fiber (beans, psyllium, oat bran, barley). Recommended total fiber intake is >25g for women and >35g for men per day, uptitrated over one week to improve tolerance. Dr. Wang recommends aiming for dietary fiber intake with foods such as two kiwi fruits a day or 4 prunes a day (Chey 2021). Although this is first line treatment, evidence has not supported improvement with fiber compared to placebo. If fiber is not tolerable, it is okay to stop it.
Osmotic laxatives are also a backbone treatment. Dr. Wang recommends polyethylene glycol (easily titratable) or milk of magnesia. Lactulose should be avoided particularly in patients with suspected ileus or obstruction as this can generate increased gas when metabolized and potentially induce megacolon.
Stimulant laxatives include senna and bisacodyl. Dr. Wang counsels to take it just when patients are actively constipated and then to stop once they are regular to minimize tolerance. Oral tabs can be taken at night (so peak onset can be timed closer to morning) versus rectal bisacodyl can be in the morning given fast onset.
Secretagogues include linaclotide, plecanatide, & lubiprostone that work by activating chloride receptors in the bowel (think of medicated cholera). Lubiprostone is FDA approved for opioid induced constipation, chronic constipation, and women with IBS-C. Linaclotide & plecanatide are approved for chronic constipation and IBS-C and contraindicated in children. In Dr. Wang’s experience, linaclotide can lead to ‘explosive’ diarrhea, so consider using the lowest of three doses if this occurs. These new medications are useful, but in a network meta-analysis including bisacodyl, bisacodyl performed better than these secretagogues at 4 weeks (Nelson 2017).
Promotility agents: Prucalopride is a prescription laxative that works by increasing bowel contraction. Consider using this agent in cases of slow-transit constipation instead of a secretagogue or if there is no response to secretagogues.
Suppositories/Enemas- Try a bisacodyl suppository first for ease of use. Various enemas (tap water, mineral oil, soap suds, & phosphate) were similarly effective when studied in pediatric patients (Anderson 2019). Therefore, it is important to focus on the potential side effects. For example phosphate or Fleets enemas can lead to hyperphosphatemia, particularly in patients with CKD. Milk and molasses enemas are highly effective and can be considered inpatient.
Pelvic Floor Dysfunction- Biofeedback with trained therapists is recommended and effective (Wald 2016). Positioning with flexion of the hips using something like a “squatty potty” can be recommended to aid with defecation.