This post contains links to Dr. Josh Farkas‘ IBCC Chapter & Cast – Submassive & Massive PE, September 5, 2019. [Link To IBCC Podcast] [Link To IBCC Chapter].
Here are excerpts from the IBCC Chapter:
CONTENTS
- Preamble
- Diagnosis & risk stratification
- Physiology of the PE death spiral
- Resuscitation
- Anticoagulation (heparin)
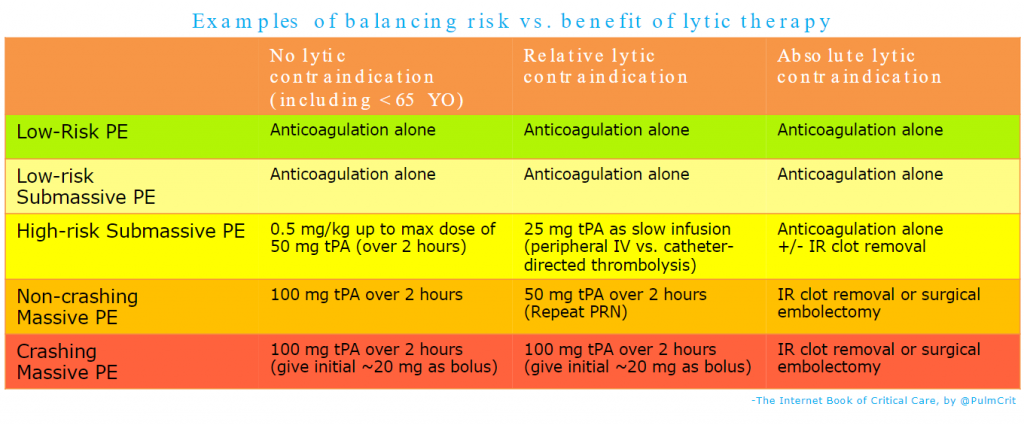
- Thrombolysis
- Other treatments
- Some unusual & confusing situations: Submassive or massive PE plus…
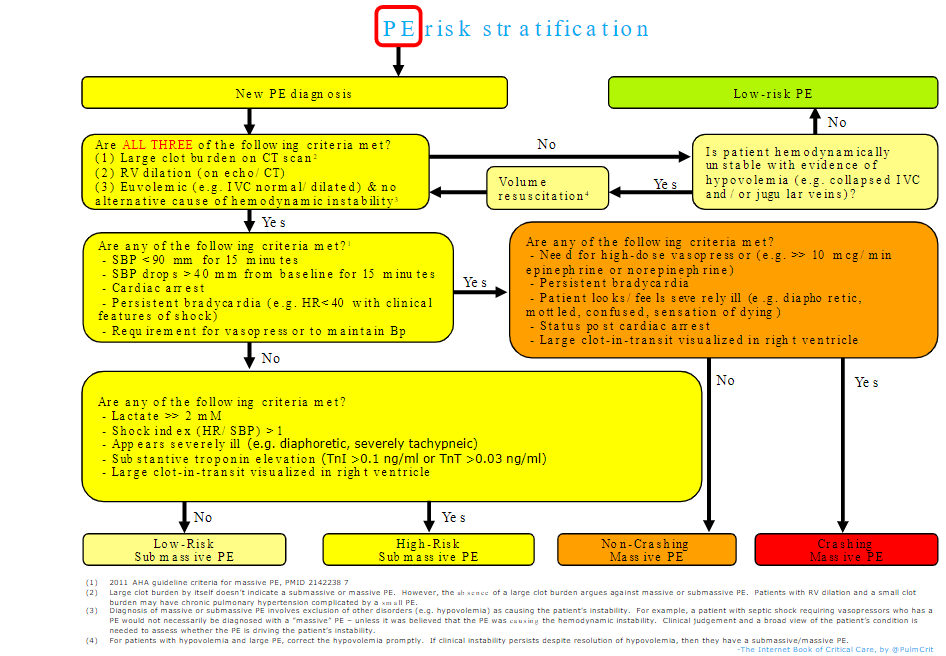
- Algorithm
- Checklist for massive PE resuscitation
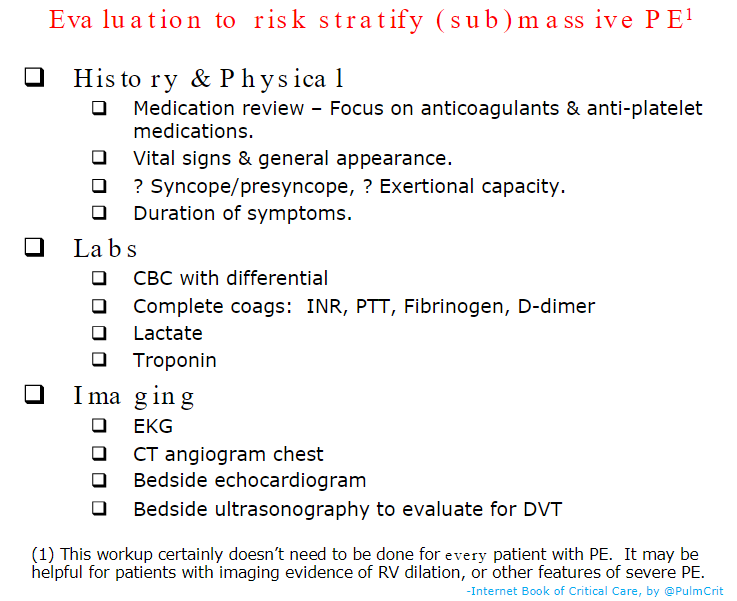
- Algorithm for risk-stratification
- Podcast
- Questions & discussion
- Pitfalls
preamble
Controversy abounds regarding pulmonary embolism, and will likely persist into the foreseeable future. This chapter includes schemas to provide direction for how these patients might be managed (and which are largely consistent with the PERT consortium consensus practices)(31185730). However, individual patients are quite heterogeneous, so these concepts need to be adapted to the specifics of each patient (including patient preferences).
is PE driving the patient’s instability?
Lots of unstable patients have PE, but in some cases they may have multifactorial instability (e.g. PE plus sepsis plus hypovolemia). Thrombolysis is beneficial only if PE is causing the patient’s instability. Factors to consider are:
- (1) Clot burden on the CT scan
- In order to blame the patient’s instability on PE, there should be a moderate to large clot burden on the CT scan.
- The precise amount of clot on the scan may not be useful (e.g. whether the patient has a “saddle” PE). However, if there is only a small amount of clot, PE probably isn’t causing the instability. For example, a patient with right ventricular dilation and small clot burden may have chronic pulmonary hypertension.
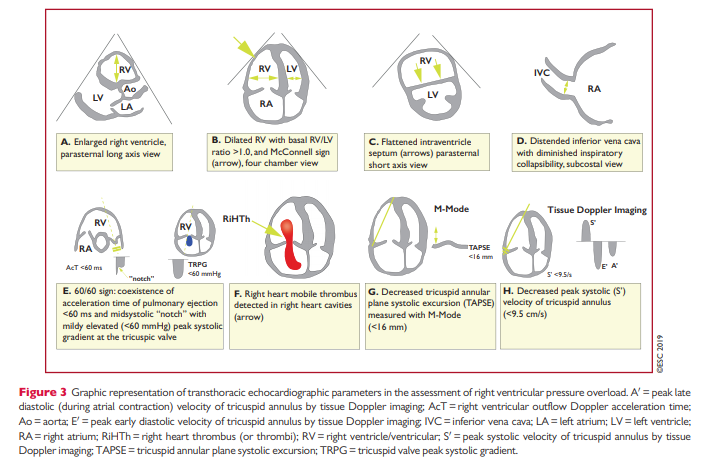
- (2) Global hemodynamic assessment with echocardiography
- Patients who are unstable due to PE should have at a minimum a dilated inferior vena cava and a dilated right ventricle.
- If the inferior vena cava and right ventricle aren’t dilated, consider whether another process is causing the patient’s instability (e.g. hypovolemic shock plus small PE).
Ultimately, clinical judgement is necessary to determine whether a patient’s instability is caused by the pulmonary embolism. For more information on the investigation of shock, see the shock chapter.