Today I’ve reviewed the resources I’ve linked to in this post.
First, I reviewed my post, Toxidrome Summary Graphics From Drs. Faidal And Farkas
Posted on April 18, 2021 by Tom Wade MD.
Then I reviewed and linked to Dr. Farkas’ IBCC chapter on Sodium Channel Blocker Toxicity.
And finally, I reviewed and link to Dr. Weingart’s outstanding EMCrit Podcast 98 – Cyclic (Tricyclic) Antidepressant Overdose. May 14, 2013. The podcast and show notes are a great practical review of what is discussed in Dr. Farkas’ chapter.
Here are the links and excerpts from Dr. Josh Farkas’ outstanding IBCC chapter, Sodium Channel Blocker Toxicity (including tricyclic antidepressants), April 26, 2021. Dr. Farkas introduces the topic:
Blockade of the fast cardiac sodium channels is an important component of cardiotoxicity due to many intoxicants. Historically the most common cause of sodium channel blockade has been tricyclic antidepressant poisoning, but a wide variety of xenobiotics can affect the sodium channels. Fortunately, close attention to the EKG may be sufficient to reach an accurate diagnosis of sodium channel blockade (regardless of the agent involved).
Here are direct links to Dr. Farkas’ chapter on Sodium Channel Blocker Toxicity:
Contents:
- Overview – sodium channel blockers & tricyclic antidepressants
- Diagnosis
- Management – three antidotes
- Management – clinical approach
- Podcast
- Questions & discussion
- Pitfalls
- PDF of this chapter (or create customized PDF)
Here are some excerpts from the chapter:
defining “sodium channel blockers”
- The term “sodium channel blocker” is used here solely to refer to agents with either class Ia or class Ic antiarrhythmic activity, which causes a slowing of phase-zero depolarization in cardiomyocytes (purple arrows above). Slowing phase-zero depolarization on a cellular level causes QRS prolongation, leading to characteristic EKG changes described further below.
- When people say “sodium channel blocker,” what they generally mean is “drug that delays phase zero depolarization of the myocardial fast sodium channels.”
- The term “sodium channel blocker” in this chapter doesn’t include class Ib antiarrhythmics (e.g., lidocaine), despite the fact that lidocaine does inhibit sodium channels.
- Lidocaine doesn’t affect phase zero depolarization, nor does it prolong the QRS complex.
- Lidocaine can actually reduce the action potential duration, making it useful in the treatment of arrhythmias caused by class Ia or class Ic intoxication (more on this below). Lidocaine’s ability to tighten up the QTc interval likewise makes it useful in the management of torsade de pointes.
physiology of TCA intoxication
- TCAs have several physiologic effects:
- Sodium channel blockade.
- Anticholinergic activity, potentially causing an anticholinergic toxidrome.
- Blockade of peripheral alpha-1 adrenergic receptors, causing vasodilation.
- Central antihistamine activity, causing somnolence.
- Antagonism of central GABA-A receptors, promoting seizure.
- Inhibition of presynaptic reuptake of dopamine, norepinephrine, and serotonin.
- Among these effects, inhibition of cardiac sodium channels is often the greatest life threat. Other toxic effects will generally respond to the usual supportive measures applied to critically ill patients.
Agents That Inhibit Cardiac Sodium Channels
agents with the potential to inhibit sodium channels
- Tricyclic antidepressants: amitriptyline, clomipramine, desipramine, imipramine, nortriptyline, protriptyline, trimipramine.
- Some other antidepressants: bupropion, citalopram, fluoxetine, maprotiline, paroxetine, venlafaxine.
- Type Ia antiarrhythmics: disopyramide, procainamide, quinidine.
- Type Ic antiarrhythmics: flecainide, propafenone.
- Beta-blockers: acebutolol, betaxolol, oxprenolol, propranolol.
- Antipsychotics: thioridazine, loxapine.
- Antihistamines: chlorpheniramine, diphenhydramine, dimenhydrinate, doxepin.
- Antiepileptics: carbamazepine, oxcarbazepine, lacosamide, lamotrigine, phenytoin.
- Antimalarials: chloroquine, hydroxychloroquine, quinine.
- Muscle relaxants: orphenadrine, cyclobenzaprine.
- Miscellaneous: Amantadine, cocaine, tramadol, topiramate, some insecticides.
variation between agents
- The above xenobiotics are obviously quite variable, with distinctive toxicities.
- In some cases, intoxication is often dominated by sodium channel blocking effects (e.g., TCAs and antiarrhythmics). In other cases, clinical intoxication is usually dominated by effects on other receptors (e.g., cocaine or antihistamines).
- Combinations of multiple different xenobiotics which block sodium channels may potentiate this blockade (e.g., combined overdose with diphenhydramine plus cyclobenzaprine).
EKG findings in sodium channel blockade
EKG is test of choice
- EKG is the most direct reflection of cardiac sodium channel blockade.
- EKG is the only test capable of suggesting sodium channel blockade in a patient with an unreliable or unobtainable history.
- If EKG abnormalities are suspected to be due to sodium channel blocker toxicity, two ampules (100 mEq total) of hypertonic bicarbonate should be given with a repeat EKG subsequently. Improvement in EKG findings following administration of bicarbonate supports the presence of sodium channel blockade.
- In a patient who overdosed on a medication known to block sodium channels (e.g., TCA), the EKG should be repeated frequently to allow for early detection of sodium channel toxicity.
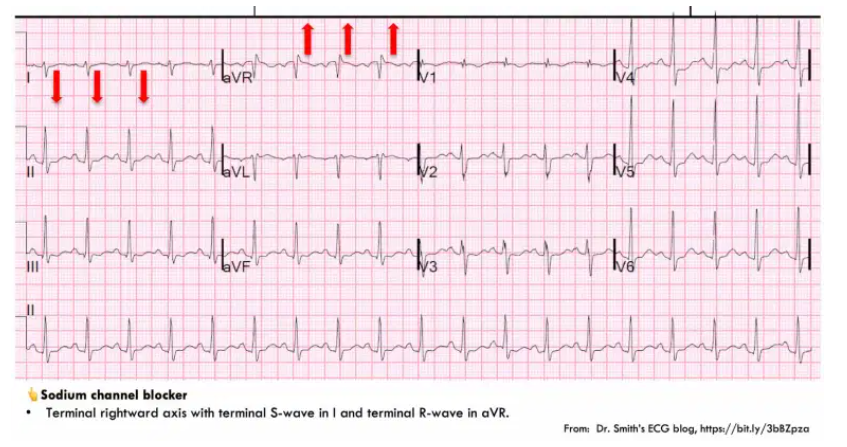
terminal right-axis deviation (RAD) with tall R-aVR
- The key to diagnosing sodium channel blockade is recognition of terminal rightward axis deviation. Electrophysiologically, this is caused by slow conduction through the myocardium, leading to delayed depolarization of the right ventricle (such that the last bit of the QRS complex points in a rightward direction). This creates the following pattern:
- (1) Deep, terminal S-wave in Lead I (which may be broad or slurred).
- (2) Terminal tall R-wave in aVR.
- The differential diagnosis of this pattern focuses on three entities: sodium channel blockade, hyperkalemia, or Brugada syndrome.
- Hyperkalemia can generally be excluded rapidly based on other features of the EKG, or laboratory studies.
- Brugada syndrome is discussed further below (but as a rule of thumb, a true Brugada Syndrome patient is extremely rare – so Brugada syndrome is a bit of a diagnosis of exclusion).*
*Here are the results of a search on Brugada Syndrome from Dr. Smith’s ECG blog.
- Among patients with TCA intoxication, a tall R-wave in aVR (R-wave >3 mm or an R/S ratio >0.7) predicts seizure or arrhythmia.(7618783)
[There is much more detail on ECG patterns to review in this section.]
clinical manifestations
clinical manifestations of cardiac toxicity
- Hypotension.
- Sinus tachycardia.
- Monomorphic ventricular tachycardia.
CNS effects
- Sodium channel blockers can often also penetrate the brain, with a variety of effects:
- TCAs can inhibit central GABA receptors.
- CNS sodium channels may also be affected.
- Common manifestations are delirium, agitation, sedation, coma, and especially seizures.
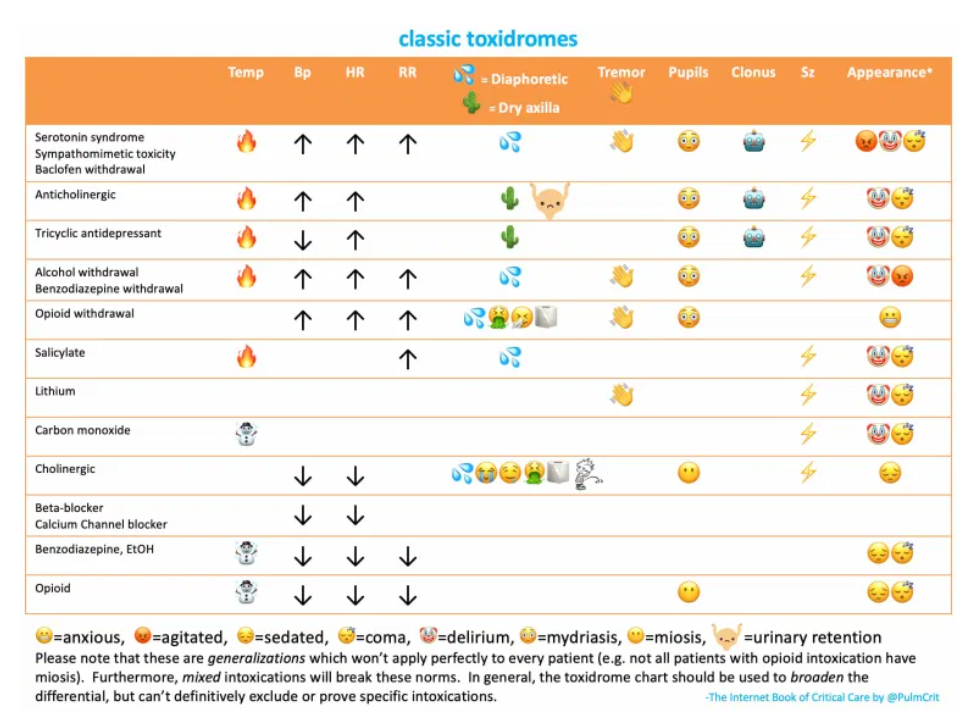
simultaneous anticholinergic toxidrome
- Many agents that block sodium channels also have anticholinergic effects (e.g., antihistamines, TCAs). These may simultaneously cause an anticholinergic toxidrome, with the following features:
- Dry, flushed skin, sometimes with hyperthermia.
- Pupillary dilation.
- Delirium, coma.
- Urinary retention.
- More on the anticholinergic toxidrome here.
And finally, I reviewed and link to Dr. Weingart’s outstanding EMCrit Podcast 98 – Cyclic (Tricyclic) Antidepressant Overdose. May 14, 2013. The podcast and show notes are a great practical review of what is discussed in Dr. Farkas’ chapter.