In this post I link to and excerpt from Dr. Josh Farkas‘ Internet Book Of Critical Care [Link is to the Table of Contents] chapter, Anticholinergic intoxication, April 12, 2021.
All that follows is excerpted from Dr. Farkas’ chapter [I do this because it helps me remember the material].
Here are the excerpts:
CONTENTS
- Anticholinergic agents
- Epidemiology
- Clinical presentation
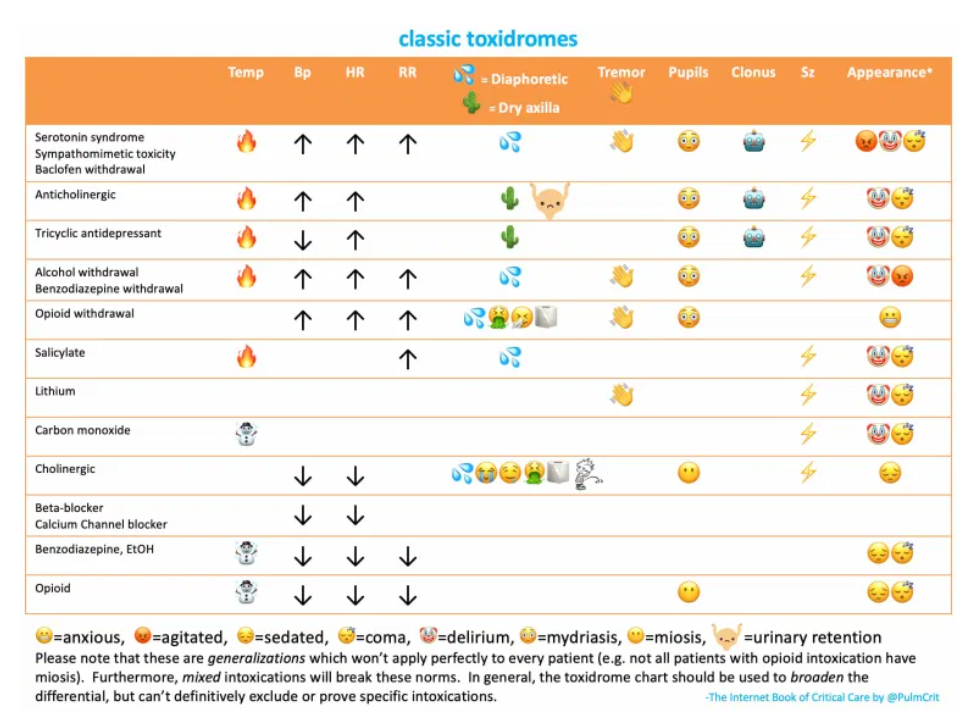
- Differential diagnosis
- Evaluation
- Management
- Podcast
- Questions & discussion
- Pitfalls
- PDF of this chapter (or create customized PDF)
anticholinergic agents
clinical presentation
Mad as a hatter, blind as a bat, red as a beet, hot as a hare, dry as a bone, full as a flask.
anticholinergic toxidrome
- CNS effects:
- Most often causes agitated delirium (often with hallucinations, incoherent speech, picking at the air or objects).
- More severe cases may present with seizure and/or coma.
- CNS effects may persist after peripheral features have resolved.
- Pupillary dilation, causing blurry vision and photophobia.
- Tachycardia.
- Hyperthermia with dry, flushed skin (examination may reveal no sweat in the armpits).
- Urinary retention.
- Ileus.
core elements of the anticholinergic toxidrome
- Key elements in the toxidrome are:
- 😳 Dilated pupils
- 🤡 Delirium
- 💕 Tachycardia
- 🌵 Dry skin – This is an essential element, which helps separate anticholinergic toxidromes from sympathomimetic toxidromes.
- These four elements suggest an anticholinergic toxidrome.
- Anticholinergic toxicity is often one component of tricyclic intoxication. An EKG may be helpful in sorting out a pure anticholinergic syndrome versus the combination of an antiholinergic syndrome plus sodium channel blockade.
Opsoclonus is rapid involuntary eye movements in all directions. It has a broad differential including infection, infarction, stroke, or intoxication (lithium, phenytoin, anticholinergics, organophosphates)(8879053)
differential diagnosis
differential diagnosis
- Sympathomimetic intoxication.
- Combined anticholinergic plus sodium channel blocker poisoning (e.g., tricyclic antidepressants).
- Combined antihistamine plus acetaminophen ingestion (many combination tablets contain both, such as Tylenol PM and NyQuil)
- Salicylate intoxication.
- Septic shock.
- CNS infections (e.g., meningitis).
- Other causes of delirium (more in the delirium chapter here).
evaluation
laboratory studies
This will vary depending on the context, with common considerations including:
- STAT fingerstick glucose, if mental status alteration.
- Electrolytes, Ca/Mg/Phos, complete blood count.
- Creatinine kinase level (with a repeat value if concern for the evolution of rhabdomyolysis).
- Serum acetaminophen and salicylate levels.
- Pregnancy testing as appropriate.
EKG
- This is essential to evaluate, especially for any evidence of sodium channel blocker activity (e.g., QRS widening and tall R-wave in aVR).
further investigation of altered mental status
- Depending on the clinical context, additional studies may be considered (e.g., head CT scan and potentially lumbar puncture).
- If anticholinergic intoxication is strongly suspected, then a physostigmine challenge may be used diagnostically (more on this below). If physostigmine causes a resolution of delirium, this establishes the presence of an anticholinergic toxidrome and removes the need for further neurodiagnostic testing.
physostigmine
- Physostigmine is an acetylcholinesterase inhibitor. It inhibits degradation of acetylcholine within the synapse, thereby increasing acetylcholine signaling levels.
- Physostigmine is extremely similar to neostigmine, which is commonly used in intensive care units for management of colonic pseudo-obstruction (more on neostigmine here). The difference between the two agents is that physostigmine penetrates the brain, whereas neostigmine doesn’t. Administration of the two agents is similar.
controversy surrounding physostigmine
[See chapter for details on the controversy]
- Currently, physostigmine is experiencing a resurgence of popularity. It’s a safe and effective medication when used properly (i.e., low-and-slow dosing) for the right patient (i.e., not patients with life-threatening tricyclic intoxication).
indications for physostigmine
- Physostigmine may be utilized for patients in whom an anticholinergic toxidrome is known or strongly suspected.
- Diagnostic benefit:
- Delirium resolution following physostigmine establishes the diagnosis of an anticholinergic toxidrome. This may allow the patient to be spared further diagnostic evaluation (e.g., CT scan and lumbar puncture).
- Note that improvement following physostigmine doesn’t necessarily exclude all possible coingestions (e.g., acetaminophen). However, this explains the etiology of the patient’s delirium, obviating the need for a delirium workup.
- Therapeutic benefit:
- Physostigmine may reduce the need for intubation among patients with marked agitation.
- Physostigmine may help some patients avoid potentially deliriogenic medications (e.g., high-dose benzodiazepines).
potential contraindications
- 💡 The precise contraindications remain controversial. When in doubt, call a local toxicologist or poison control.
- (1) EKG demonstrating sodium channel blockade (e.g., wide QRS plus terminal right-axis deviation, with a deep S-wave in lead I and a tall R-wave in aVR).
- (2) Abnormally low heart rate within the context of anticholinergic toxicity (e.g., heart rate below ~60-80 b/m), or known cardiac conduction disease (e.g., AV block on EKG).
- (3) Anatomic obstruction of the urinary or gastrointestinal tract.
- (4) Frank coma with inability to protect the airway (physostigmine may rarely cause vomiting).
- (5) Epilepsy, recent seizure, or known coingestion with a proconvulsant substance.
- (6) Active asthma exacerbation or severe asthma.
initial dosing
- Physostigmine can cause bradycardia, so this should be done with telemetry monitoring and atropine available.
- (1) Start with 1 mg IV slowly over 5-10 minutes.(12902007)
- 🔑 Administering the physostigmine too rapidly will amplify side effects. One key to giving physostigmine safely and effectively is to give it s-l-o-w-l-y.
- 🛑 Observe for clinical signs of cholinergic excess (e.g., salivation, lacrimation, urination, defecation, emesis, bradycardia, diaphoresis). If any of these occur, they argue against an underlying anticholinergic toxidrome – so perhaps you have the wrong diagnosis. If cholinergic toxicity were to occur, atropine could be used to reverse it (the atropine dose is half of the amount of physostigmine which has been administered). Alternatively, glycopyrrolate could be used to selectively reverse physostigmine’s peripheral cholinergic effects, without affecting CNS acetylcholine activity.
- Observe for any clinical improvement. 1 mg should usually be a sufficient dose to see some improvement among patients with anticholinergic intoxication.
- (2) If no side effects are noted, an additional 1 mg IV may be given slowly, after 10-15 minutes.
treatment of agitation
[See chapter for details]
other management issues
hemodynamics
- Hypertension and tachycardia are generally mild and well tolerated. Before treating hypertension, the first step is to manage any agitation:
- If agitation is driving the tachycardia, the best approach is to treat the agitation.
- Avoid giving a beta-blocker up front, as this may impede the subsequent use of dexmedetomidine and/or physostigmine.
- Hypotension may occur, which may respond to fluid resuscitation.
hyperthermia & rhabdomyolysis
- Hyperthermia is occasionally severe and may require treatment:
- Physical cooling (more in the chapter on hyperthermia).
- Management of agitation as described above.
- Avoid physical restraints, as this only worsens exertion and hyperthermia.
- Measure creatinine kinase and treat rhabdomyolysis as appropriate (more in the chapter on rhabdomyolysis).
urinary retention
- A Foley catheter may be required.
- Consider serial bladder scans to ensure that the patient doesn’t develop urinary retention (if the patient is unable to communicate clearly).
QT management
- Some antihistamines (e.g., diphenhydramine) can prolong the QT interval and cause torsade de pointes.(21171853)
- The QT interval should be monitored.
- Among patients with QT prolongation, maintaining Mg >3 mg/dL and K >4 mEq/L may reduce the risk of arrhythmia.
- If patients develop torsade de pointes, this should be treated as explored in the chapter on torsade de pointes.
seizures
- Initial therapy is a benzodiazepine, for example:
- Lorazepam 0.1 mg/kg IV.
- Midazolam 10 mg IV/IM.
- Recurrent seizures may be managed by intubation and sedation with propofol.
- For recurrent seizures or status epilepticus, addition of levetiracetam may be reasonable. (Note that phenytoin is contraindicated, due to its potential to worsen sodium channel blockade.)
- More on the treatment of status epilepticus here.
management of combined anticholinergic plus sodium channel blocker toxicity
The above link is a direct link to that section of the IBCC chapter.
I’ve excerpted the entire section in a seperate post to reinforce my learning.