Here is the link to the outstanding IBCC: COVID-19 podcast* of
March 2, 2020 by Dr Josh Farkas from the Internet Book Of Critical Care [Link is to the Table of Contents].
* It is on the above page that has all of the thoughtful comments from readers are posted. As of today there are 72 comments. I just reviewed all of the comments and all of Dr. Farkas’ excellent responses. Note to myself: I need to revisit the page every few days or so as new comments are always coming in.
And here is the link to the IBCC COVID-19 Chapter [The chapter has a great outline that links to every topic covered in the chapter.The chapter as well as the comments page needs to be reviewed as Dr. Farkas is revising it almost daily as new information becomes available]:
Here are excerpts I made as I reviewed the chapter just to help my retention
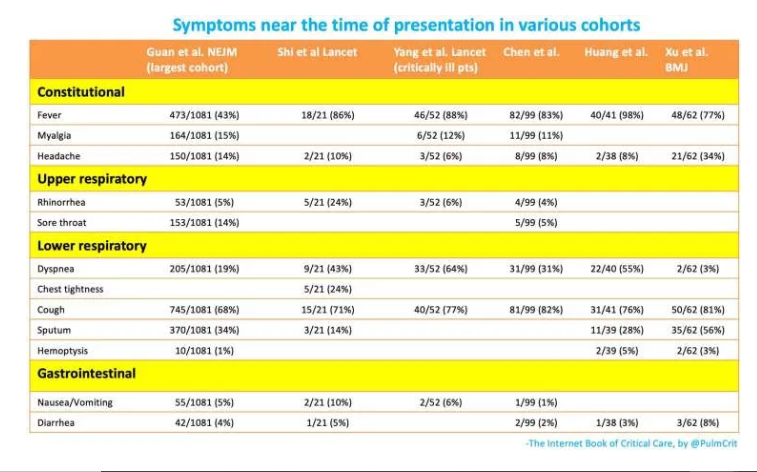
Signs & symptoms
- COVID-19 may cause constitutional symptoms, upper respiratory symptoms, lower respiratory symptoms, and, less commonly, gastrointestinal symptoms. Most patients will present with constitutional symptoms and lower respiratory symptoms (e.g. fever and cough).
- Fever:
- The frequency of fever is variable between studies (ranging from 43% to 98% as shown in the table above). This may relate to exact methodology used in various studies, different levels of illness severity between various cohorts, or different strains of the virus present in various locations. Additionally, some studies defined fever as a temperature >37.3 C (Zhou et al. 3/9/20).
- Regardless of the exact numbers – absence of a fever does not exclude COVID-19.
- Gastrointestinal presentations: up to 10% of patients can present initially with gastrointestinal symptoms (e.g. diarrhea, nausea), which precede the development of fever and dyspnea (Wang et al. 2/7/20).
- “Silent hypoxemia” – some patients may develop hypoxemia and respiratory failure without dyspnea (especially elderly)(Xie et al. 2020).
- Physical examination is generally nonspecific. About 2% of patients may have pharyngitis or tonsil enlargement (Guan et al 2/28).
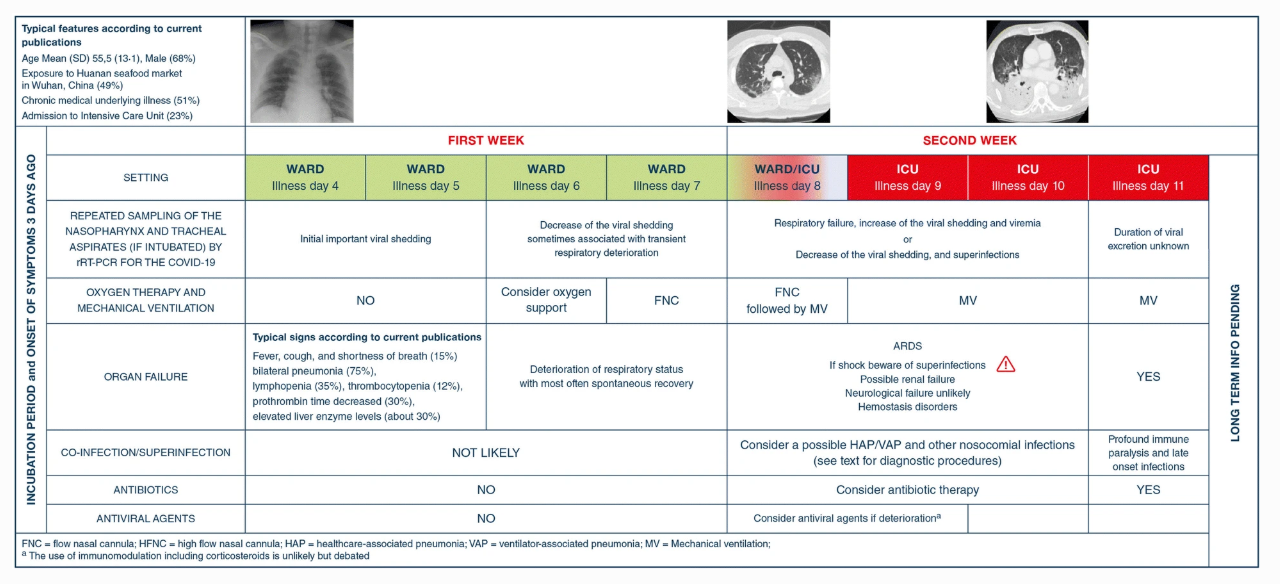
Typical Disease Course:
Here is a link to the figure below that is clearer than the one below from: Severe SARS-CoV-2 infections: practical considerations and management strategy for intensivists
- Incubation is a median of ~4 days (interquartile range of 2-7 days), with a range up to 14 days (Carlos del Rio 2/28).
- Typical evolution of severe disease (based on analysis of multiple studies by Arnold Forest)
- Dyspnea ~ 6 days post exposure.
- Admission after ~8 days post exposure.
- ICU admission/intubation after ~10 days post exposure. However, this timing may be variable (some patients are stable for several days after admission, but subsequently deteriorate rapidly).
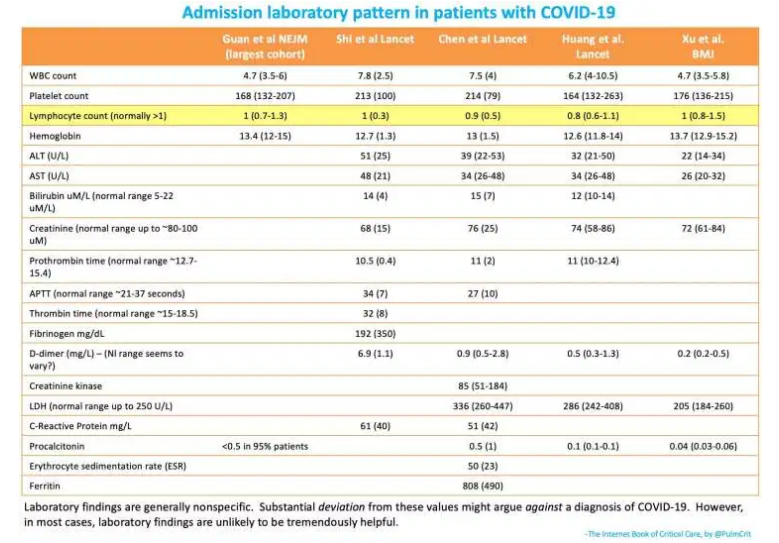
The most important point of Dr. Farkas labs table below is at the very bottom of the chart:
Laboratory findings are generally non-specific. Substantial deviation from these values might argue against of COVID-19. However, in most cases laboratory findings are unlikely to be tremendously helpful.
Note to myself: As always review the complete IBCC chapter COVID-19.