In this post, I link to and embed the YouTube video, Management of Gastrointestinal Symptoms in Dysautonomia – Laura Pace, MD, PhD. Jul 20, 2020. Dysautonomia International.
I also place slides from her talk in this post for rapid review.
Dr. Pace states that the above definition is not helpful and does not explain anything.And so when I see a patient in clinic, I just sort of want to remind you that not everyone I see initially knows that they have a disorder of the autonomic nervous systemSometimes this is me picking it up and sending them for confirmatory diagnosis. But many of you that come to see me actually already have this diagnosis. But what I do is I start with a detailed history and physical examination, so well beyond justgastrointestinal symptoms, usually I want to start when youfirst got sick.The vast majority of my patients are female, and they’ve already been seen by usually a huge number of physicians in a bunch of different specialties.
They typically report a constellation of symptoms, and I’m sure none of these are unusual for you we can start at the top with brain fog, headache, dry mouth, dry eyes, palpitations, shortness of breath, and numerous gastrointestinal symptoms that usually range from difficulty swallowing to even just what we call globus sensation–that’s that persistent feeling that something’s stuck in your throat and you kind of keep swallowing to try and clear it, but you don’t have like a true impaction within the esophagus–all the way to abdominal pain, nausea, vomiting, constipation, diarrhea, or some alteration in between.And so, historically, within the realm of gastroenterology, and even when I came through training, the inclination has been to diagnose people who come in with this constellation of symptoms with a functional disorder such as irritable bowel syndrome.
And this is completely incorrect. So that terminology describes a cluster of symptoms but does not give you a diagnosis and does not impart any understanding to what the underlying pathophysiology of your symptoms are.
Dr. Pace is going to show us, in the rest of her talk, how to diagnose these GI symptoms in a more helpful way.
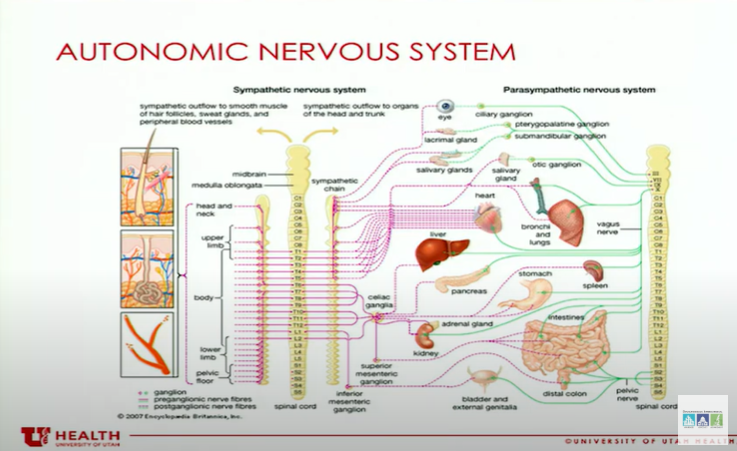
The reason I’m showing this slide is I actually find it’s helpful when I talk to other physicians who think that the patients that I’m seeing have a psychiatric illness.And so the point that I make with this, if we look at the innervation of the autonomic nervous system, it innervates just about everything. And so when something with the autonomic nervous system goes awry, it’s not surprising thatyou have all these symptoms.
And so if you look at the sympathetic branches and then the parasympathetic branches, these two systems have different functions. And I know many of you are probably familiar with this.But the sympathetic nervous system is your fight-or-flight. So when this system is overactive, it shuts down digestion. And so what we see in individuals with an overactive component of the sympathetic nervous system, we see a lot of delay in different regions of the gastrointestinal tract, a lot of difficulty with eating.And then with the parasympathetic nervous system, you can see the opposite, so you can see a lot of really persistent diarrhea that we have a difficult time managing.But, again, the autonomic nervous system is innervating everything. It’s not unusual for you to have all these symptoms. It’s not unusual if your symptoms are exacerbated by stress.That, again, does not mean that you have a psychiatric illness, no matter what your physicians tell you.
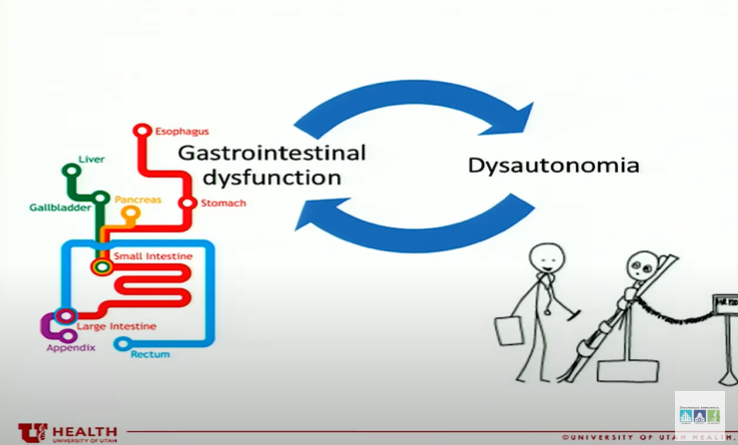
What I don’t understand, when I am seeing you guys in clinic, is does the gastrointestinal dysfunction come first or does the dysautonomia come first? It’s essentially a chicken or egg problem.
And so the thing that I struggle with is in order to make your gastrointestinal symptoms better, do I have to treat your dysautonomia? And if your dysautonomia gets better, can I expect your gastrointestinal symptoms to get better? And I think that is the case.
And so I think there are specific things that I can do as a gastroenterologist, but then there are other things where we actually really have to address the underlying dysautonomia.One of the other problems is I feel like it’s really important to understand what comorbid conditions you actually have.
But I think it’s [also] important to know whether you have an underlying connective tissue disorder, whether it be EDS or some other, whether you have presence of mast cell activation syndrome, or a metabolic disorder, or an autoimmune disorder, because all of this is going to change how I approach the symptoms that we have to address for you.So I typically recommend a thorough evaluation so that I can put together an entire clinical picture and sort of make better recommendations.
So I typically recommend a thorough evaluation so that I can put together an entire clinical picture and sort of make better recommendations.And so what I’m going to go through here is the evaluation that I have most of my patients undertake.
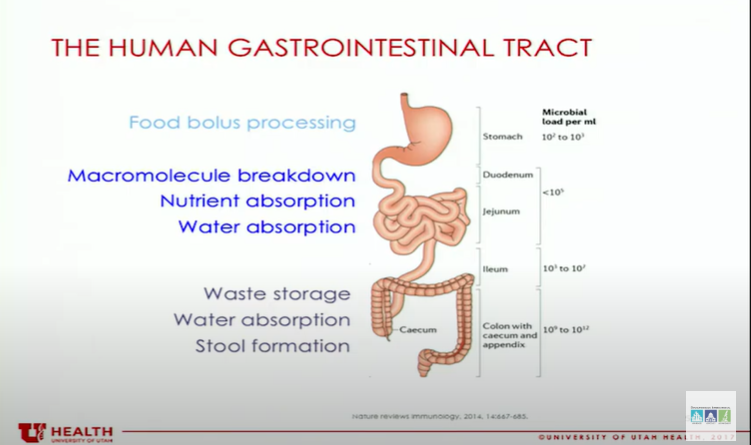
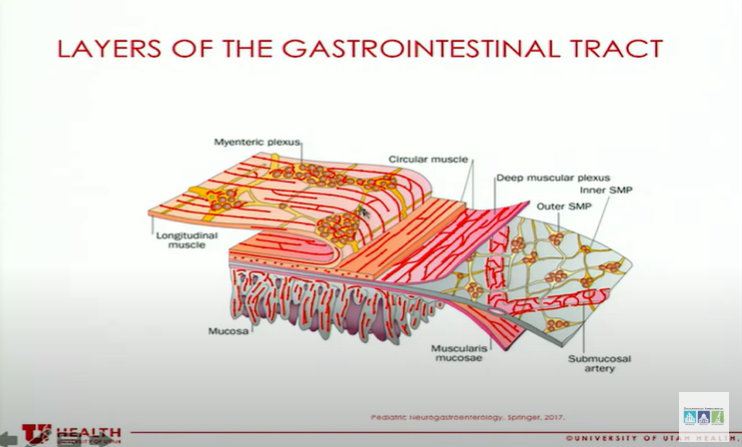
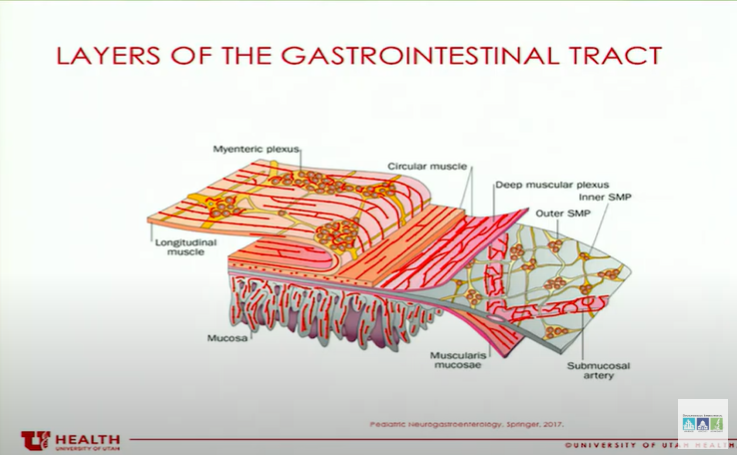
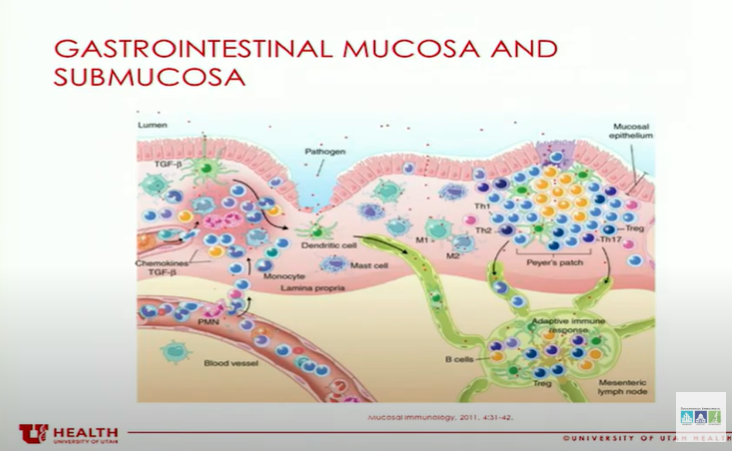
. . . when we look at the entire gastrointestinal tract and all its layers, there are lots of layers of muscles and there’s lots of nerves there. So there’s lots of opportunity for things to go wrong.
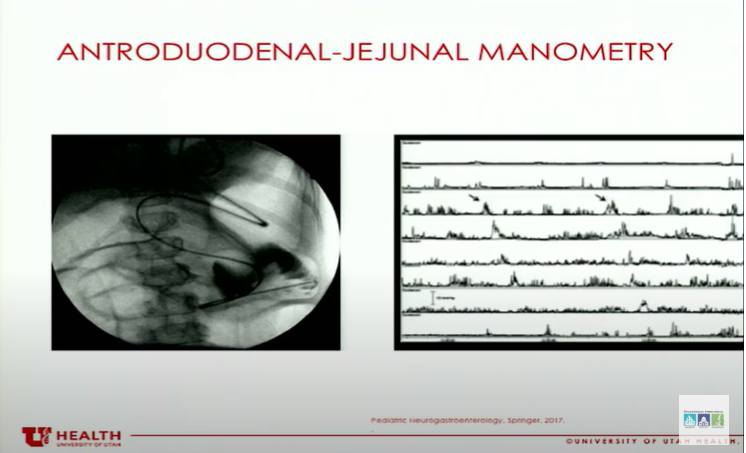
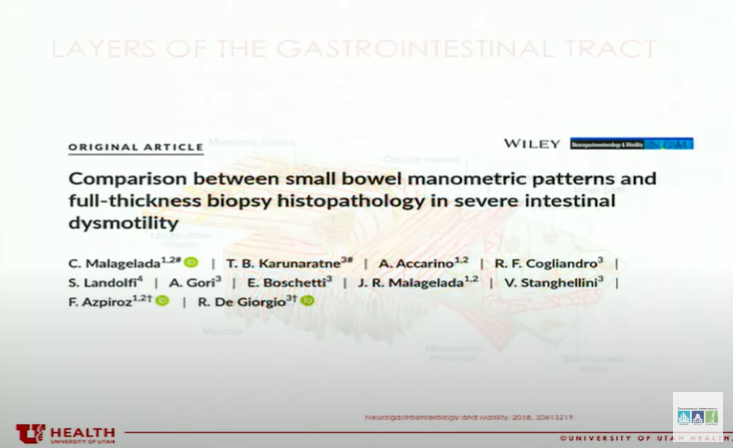
This article that was published in 2017 on neurogastroenterology and motility compared these findings from antroduodenal manometry to full-thickness biopsies of the small intestine.So that means they actually sampled all the muscle layers. And so these are layers, when I do routine endoscopy, I’m just sampling the very inside of that luminal tissue, I’m not sampling the muscles. So I’m not able to get this information with standard mucosal biopsies, which most of you have probably had and been told they’re normal anyway. So this is a full-thickness biopsy, so it’s actually really quite interesting.
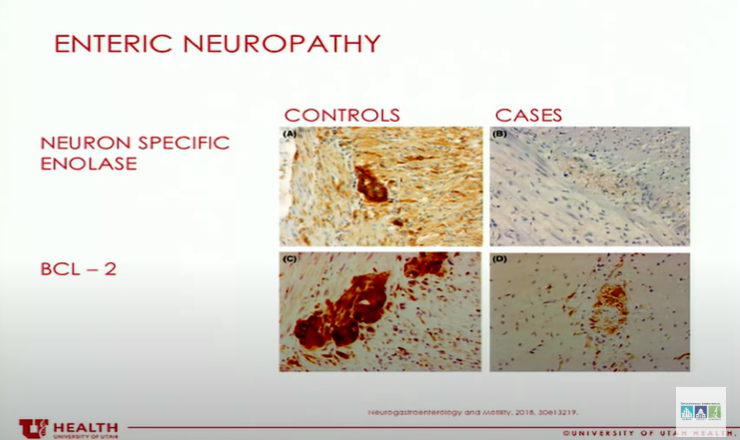
So then if we actually go and look at what the results of the full-thickness biopsy are, so these are looking under a microscope with special stains to look at different components of the tissue, and I’m gonna draw your attention to kind of the upper right box [speaker meanstosay left upper box] where you havethat kind of dark brown blob. So those are the control samples. So that’s what the tissue is supposed to look like.But if you look in the cases [on the upper right], what you can see is that cluster of neurons there is essentially absent. So this is what we would consider an actual neuropathy because the nervous system that is innervating the gastrointestinal tract is injured. That’s not what they saw on the manometry testing.
And then just to look at what a myopathy looks like, so this is a special stain from a muscle. And what you can see is the staining is very different in the controls versus the cases. And so this is a direct injury to the muscle.
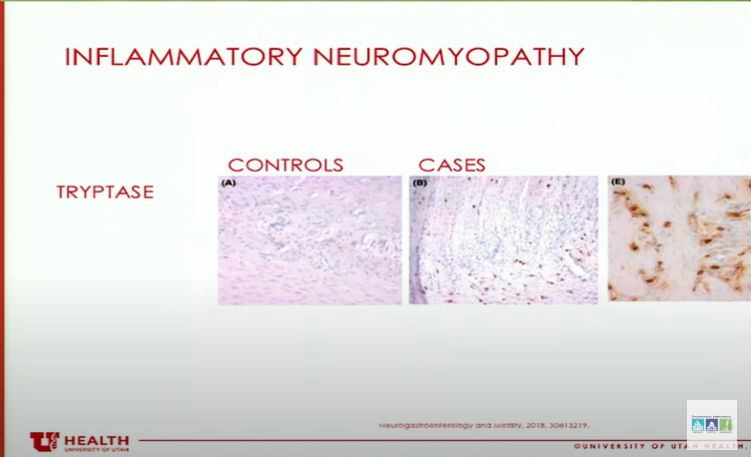
This one [ above] I thought was particularly interesting. So this is an inflammatory neuromyopathy.
So you have an injury to both the nerves and the muscle. And what they found is that, in this particular case, they actually stained for tryptase,
so they were staining for mast cells. And what they could see, if you look at all the little brown dots that are present in
the cases and not the controls, is there’s a dense mass cell infiltration within the
muscle and nerve layers. But what they found in the population that they looked at was that this could be mast
cell-mediated, this could be eosinophils that are there, or it could be lymphocytes. So, either way, this is an immune attack on the muscles and nerves that’s occurring.
And, again, I just want to remind you that this is not a diagnosis you could get from
routine endoscopy. So the take-home point from that section really is that the pathology does not correlate with
the manometry. So maybe all we need is to identify that there actually is an anomaly.
And then actually consider pursuing a full-thickness biopsy to actually get the true diagnosis,
because that would really change the direction of our therapy. And this is why, I think, the SmartPill could actually offer this, a number of centers,
rather than these specialized centers that can perform the antroduodenal-jejunal manometry.
I think that, potentially, the SmartPill could actually replace the need for antroduodenal-jejunal
manometry if it’s only available at specialized centers and provide us with an opportunity to investigate some of these diagnoses at more institutions.
Now I’m going to switch gears, and we’re going to talk about breath testing. A lot of you are always sent for these repeated courses of antibiotics.
*European guideline on indications, performance, and clinical impact of hydrogen and methane breath tests in adult and pediatric patients: European Association for Gastroenterology, Endoscopy and Nutrition, European Society of Neurogastroenterology and Motility, and European Society for Paediatric Gastroenterology Hepatology and Nutrition consensus [PubMed Abstract] [Full-Text HTML] [Full-Text PDF]. United European Gastroenterol J. 2022 Feb;10(1):15-40.
*Hydrogen and Methane-Based Breath Testing in Gastrointestinal Disorders: The North American Consensus [PubMed Abstract] [Full-Text HTML] Am J Gastroenterol. 2017 May; 112(5): 775–784.
I’m not going to show you any data from it, but I’ll just tell you what they did. So they looked at gastrointestinal motility in individuals with normal baseline who they
exposed to elevated hydrogen or elevated methane. And what they found was the elevated methane levels slowed gastrointestinal motility significantly.
And the reason that I think that this designation is actually important is that the organisms
that produce methane are not bacteria. They are single-cell organisms.
They look like bacteria to the layperson, but they are very different.
They actually represent the third domain of life. So you have eukaryotes, bacteria, and archaea.
And the reason that this distinction is important is that their cell membrane is different than bacteria, which means that they do not respond to antibiotics that were designed to target
bacteria. And so when you take an antibiotic to treat an elevated methane level, all you’re doing
is causing more microbial disturbance by going after the bacteria that are there, which then
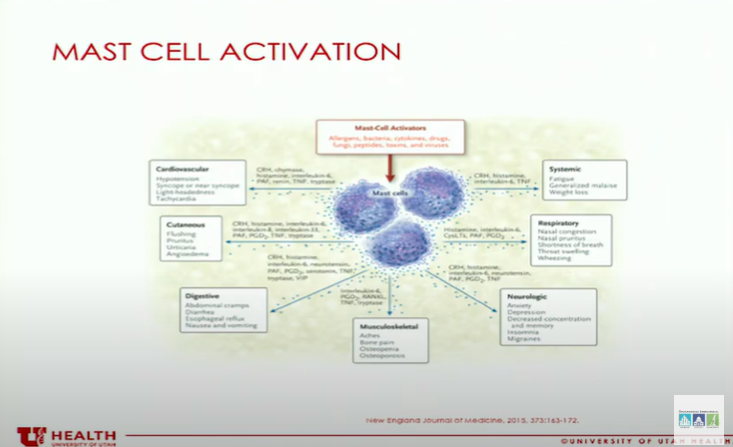
So, just to [give] you some pictures of some mast cells. You can see all the granules on the right over there, and then when it degranulates,
it releases a ton of mediators.
Mast cells, if we look at a cross-section of the gastrointestinal tract wall, they canbe just about anywhere. We usually think about them in that first layer, the mucosal layer.
They’re in close proximity to other immune cells, they’re in close proximity to blood vessels and small nerve fibers.
So when they release their mediators, they can have local effects and systemic effects.
And then this is a great paper published in the New England Journal in 2015.* This talks about all the mediators that these mast cells can release.
The diagnosis, I think, is often overlooked because people are just looking for tryptase.
I find that most of my patients actually don’t have an elevated tryptase. And so what I’ve started doing is [formalize] mast cell counts.
I understand this is not widely accepted, but I am seeing a correlation–when we have a little bit more data, we’ll eventually publish the findings–compared to true, healthy controls.
What’s been published in the literature are called healthy controls, but many of them actually had irritable bowel syndrome which actually could have mast cell activation syndrome
Never be satisfied with a diagnosis of irritable bowel syndrome. It’s not a diagnosis, it’s a descriptor of symptoms, and that means that person is not
willing to get to the bottom of what is actually causing your symptoms. Remember, this is complicated, and no one intervention will make you better, and not
all tests are for everyone. And sometimes this is a process of trial and error with our treatment modalities.
And so I always ask my patients to bear with me. I do think, as the research progresses in this area, we’ll have a better idea about
which interventions are appropriate for which populations as we move forward. Well, we don’t currently have that information right now.