In addition to today’s resource, please be sure to review:
- AMAX4 website
- “A best-practice algorithm for Critical Care Clinicians in Anaphylaxis and Asthma resuscitation”
- AMAX4 Simulation
- Emergency Medicine Cases‘ Ep 187 Crashing Anaphylaxis – AMAX4 Algorithm and The Max McKenzie Case
- Helman, A. McKenzie, B. Crashing Anaphylaxis – AMAX 4 Algorithm and The Max McKenzie Case. Emergency Medicine Cases. September, 2023. https://emergencymedicinecases.com/crashing-anaphylaxis-amax4. Accessed September 28, 2023
Today, I reviewed, link to and embed excerpts from the show notes of Emergency Medicine Cases‘ Episode 78 Anaphylaxis and Anaphylactic Shock – Live from The EM Cases Course*.
*Written Summary and blog post written by Anton Helman, March 2016. This podcast was recorded live at The EM Cases Course at North York General Hospital in Toronto February 2016.
All that follows is from the show notes of the above resource.
Podcast: Play in new window | Download (Duration: 50:53 — 46.6MB)
CASE 1: A 37 year-old otherwise healthy woman comes in to your ED complaining of an itchy red rash that started soon after eating some seafood at a restaurant. She complains of a scratchy feeling in her throat, but denies any difficulty breathing, speaking or swallowing. She denies lip or tongue swelling, SOB, abdominal pain, vomiting or fever. On exam, her vitals are normal. She appears uncomfortable, scratching at her neck with an obvious raised patchy red urticarial rash all over her neck and torso. Her voice is normal, lips and tongue do not appear swollen, there’s no stridor and her chest is clear.
Q1: Is this anaphylaxis or is this simply an allergic reaction that we don’t have to treat aggressively?
Diagnostic Criteria for Anaphylaxis
Anaphylaxis is highly likely when any one of the following three criteria is fulfilled:
1. Acute onset of an illness (minutes to hours), with involvement of the skin, mucosal tissues, or both AND at least one of the following:
- Respiratory compromise
- Reduced blood pressure or associated symptoms of end‐organ dysfunction
2. Two or more of the following that occur rapidly (minutes to hours) after exposure to a likely antigen for that patient:
- Involvement of the skin‐mucosal tissue
- Respiratory compromise
- Reduced blood pressure or associated symptoms of end‐organ dysfunction d. Persistent gastrointestinal symptoms
3. Reduced blood pressure after exposure to a known allergen for that patient (minutes to hours) [Emphasis added]
- Infants and children: low systolic blood pressure (age‐specific) or >30% decreased in systolic blood pressure
- Adults: systolic blood pressure 30% decrease from that patient’s baseline
Adapted from: Sampson HA, Munoz‐Furlong A, Bock SA, et al. Symposium on the definition and management of anaphylaxis: summary report. J Allergy Clin Immunol 2005; 115:584‐91.
Note that according to this definition of anaphylaxis, isolated hypotension after an allergen exposure can be diagnostic for anaphylaxis, and that anaphylaxis can occur without any skin manifestations.
The importance of epinephrine timing, location and dose in anaphylaxis
Q2: Is epinephrine indicated for this patient?
If the “scratching feeling in her throat” is deemed by you to be a significant respiratory symptom that indicates any compromise, then according to the definition, this patient fulfills the diagnostic criteria for anaphylaxis.
All patient who fulfill the criteria for anaphylaxis require the administration of epinephrine. Epinephrine is the only drug to show a mortality benefit in the management of anaphylaxis.
Q3: How will you administer the epinephrine in the ED? What route, what location, what dose?
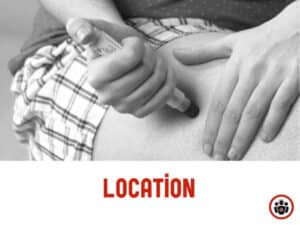
Epinephrine should be administered as soon as the diagnosis of anaphylaxis is made intramuscularly in the anterolateral thigh. Administering epinephrine IM in the deltoid muscle is not recommended.
That means, the patient needs to disrobe in order to access the thigh. Intramuscular administration of epinephrine in the anterolateral thigh reaches the maximal epinephrine serum concentration seven approximately 7 times faster compared to the arm. Subcutaneous injections should be avoided. Peak concentrations of epinephrine occurs in approximately 8 minutes when administered intramuscularly compared to approximately 34 minutes for subcutaneous injections. Q4: One of the more common causes of death in anaphylaxis is giving the wrong dose. What is the correct dose of epinephrine?
The correct dose of epinephrine for the treatment of anaphylaxis is 0.01mg/kg (to a max of 0.5mg) IM, repeated after 5 mins if there’s no clinical improvement. It is common practice to under-dose epinephrine in this setting. A 180 lb man should NOT be getting only 0.3mg IM. Any patient weighing 50Kg or more should receive 0.5mg of epinephrine IM. Take home point #1:
The most common cause of death in anaphylaxis
is not giving epinephrine at the right time at the correct dose
Second line agents for anaphylaxis
Q5: What’s the evidence for the effectiveness of the addition of H2 blockers to H1 blockers in the symptomatic relief in allergic reactions and anaphylaxis?
One study from The Annals of EM in 2000 looked at 91 adults presenting to the ED with urticaria, acute angioedema, acute unexplained stridor or acute pruritic rash within 12 hours of ingested food, drug or contact with latex. They found that the combination of 50mg of diphenhydramine plus 50mg of ranitidine compared to diphenhydramine plus placebo was significantly more likely to result in absence of urticaria at 2 hours (91.7% in the ranitidine group vs 73.8% in the placebo group).
While the addition of H2 blockers to H1 blockers may help resolve urticaria faster, the true clinical significance of this is unknown.
Certainly, there is no evidence in the literature to suggest that either H1 or H2 blockers have a mortality benefit in the treatment of anaphylaxis.
Q6: What about steroids? Which patients require steroids in the ED for anaphylaxis?
There is a paucity of evidence for the efficacy of steroids in patients with allergic reactions or anaphylaxis. Nonetheless, corticosteroids are standard care for patients with anaphylaxis. Our expert’s practice is that if the patient fulfills the diagnostic criteria for anaphylaxis, give epinephrine AND steroids. While there is no good evidence in the literature that the addition of steroids to epinephrine has a mortality benefit or prevents a biphasic reaction, it is still recommended by our expert, but only if the setting of true anaphylaxis.
If the patient does not fulfill the diagnostic criteria for anaphylaxis, then steroids are not indicated.
Remember that steroids take 4-6hrs to become effective, so (in contradistinction to epinephrine) there is no rush to administer them.
If you do give steroids, our expert recommends single dose dexamethasone in the ED, which has the advantage of a long half-life of 53hrs, thus negating the need for prescribing steroids upon discharge.