This post is in progress. As I reviewed this outstanding podcast and show notes, a number of additional topics came up for me to review (which I will be doing soon):
- Entresto (sacubitril-valsartin) – neprilisine inhibitor
- can cause elevated BNP. In patients on this medication, you need to order a pro-BNP
- Google search: Using POCUS to determine Jugular Venous Distention
- For a list of Twitter resources on heart failure: Type “heart failure” in the search box for a list.
- For a list of Twitter resources on Advanced Heart Failure: Type “advanced heart failure” in the search box for a list
- Review Cardiorenal syndrome article: See Cardiorenal Syndrome: Classification, Pathophysiology, Diagnosis, and Treatment Strategies: A Scientific Statement From the American Heart Association. Originally published11 Mar 2019 Circulation. 2019;139:e840–e878
In this post I link to and excerpt from 5 Pearls On Inpatient Heart Failure From CoreIM Posted: June 24, 2020
By: Dr. Michael Dunleavy, Dr. Shreya P. Trivedi, Dr. Greg Katz, Dr. Swapnil Heremeth, Dr. Ayesha Hasan, Dr. Zaven Sargsyan, Dr. Michelle Kittleson and Dr. Martin Fried
Graphic: Dr. Cathy Cichon
Audio: Solon Kellaher
Peer Review: Dr. Eugene Yurditsky, Dr. Stephan Pan
Here are direct links to different parts of the show notes:
Here are excerpts:
Time Stamps
See Cardiorenal Syndrome: Classification, Pathophysiology, Diagnosis, and Treatment Strategies: A Scientific Statement From the American Heart Association. Originally published 11 Mar 2019 Circulation. 2019;139:e840–e878
More excerpts from show notes:
Show Notes
Heart Failure (HF) exacerbation is a clinical syndrome (collection of signs and symptoms) due to elevated intracardiac filling pressures leading to vasoconstriction and/or volume retention.
Pearl 1: Initial clinical assessment
- Blood pressure:
- Hypotension is more common among HFrEF patients, and can be a sign of poor perfusion and even shock
- Hypertension can cause someone to go into a heart failure exacerbation
- Improve BP control with vasodilation/afterload reduction
- Pulse pressure* is the difference between systolic and diastolic blood pressure
- A narrow pulse pressure is a sign of a low output state
- Lower pulse pressure is associated with increased mortality in HFrEF patients
- *What is pulse pressure? How important is pulse pressure to your overall health? [Link is to the Mayo Clinic article]
- Heart Rate:
- Tachycardia could be a sign of shock, but if beta-blockers are on board, they can prevent this physiologic response. A normal heart rate does not rule out shock in a heart failure patient.
- Jugular venous distention/pulsation*
- *I have great difficulty using the physical exam methods detailed in the articles on determining JVD by physical exam. I will be investigating the use of POCUS as this method seems like it might be better than physical exam.
- Used to determine the intracardiac filling pressure, which is a marker for LV preload
- 2 ways to check:
- One way is to sit them upright at 90 degrees and check if you can see their JVD above the clavicle
- If you see it, they have elevated intracardiac pressures
- Sit the side of the bed at 45 degrees and assess how high the JVD is (Don’t forget to look at the ear and bilaterally!)
- Tricuspid regurgitation can cause JVD elevation in the absence of elevated cardiac filling pressures
- Need to differentiate between atrial and venous when assessing JVD
- Check the radial pulse. Venous pulsation should result in two upstrokes for every pulsation in the wrist. If it correlates 1:1, it may be arterial.
- JVP should have increased fullness of the pulsation when applying abdominal pressure
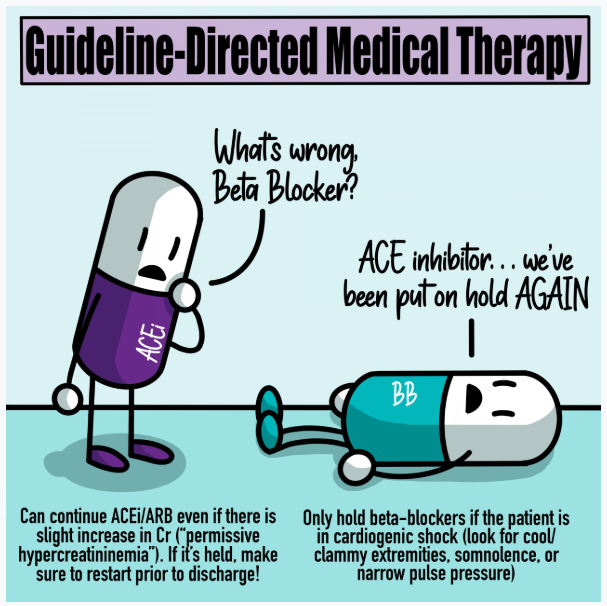
Pearl 2: Initial lab workup
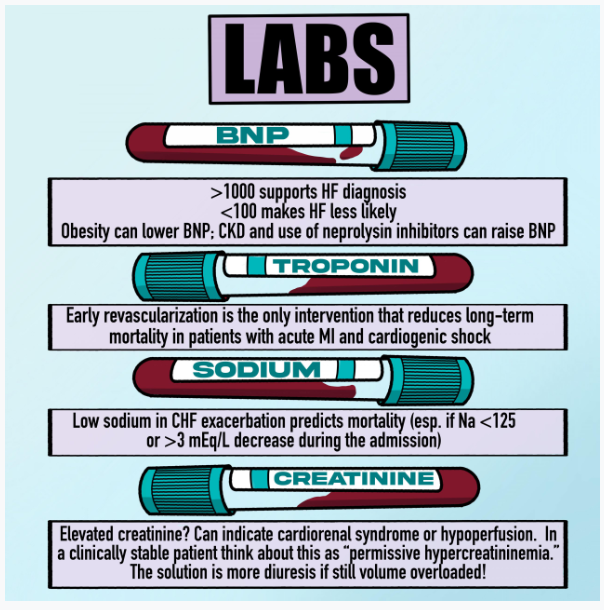
- BNP
- Elevated BNP (>1000) supports HF diagnosis, and <100 makes CHF less likely
- BNP of 350 has a likelihood ratio of 1 in one study
- Assess the trend. Some factors increase or decrease the BNP
- BNP levels are usually lower in obese patients with heart failure
- Patients with chronic kidney disease tend to have elevated BNP levels
- Neprilysin inhibitors (e.g. sacubitil-valsartan) can cause elevated BNPs, so we generally check a pro-BNP instead of BNP in patients on neprilysin inhibitors
- Troponins
- Particularly for patients with impending shock or shock or if any clinical symptoms concerning of acute coronary syndrome as a culprit of decompensated heart failure
- In patients with an acute MI who developed cardiogenic shock, early revascularization lowers 6 month mortality
- Sodium
- Low Na on admission is a predictor of both all-cause mortality and cardiovascular mortality for patients admitted with a heart failure exacerbation
- A drop in sodium levels of >3 mEq/L was associated with increased mortality
- Risk of death was particularly worse for Na <125 in heart failure exacerbations
- Creatinine
- Assess cause of elevated creatinine, since you may not always need to hold or decrease diuresis
- Elevation compared to baseline on admission is usually a sign of cardiorenal syndrome from elevated renal venous congestion
- Management of cardiorenal syndrome is with diuresis
- If the elevation occurs during diuresis, it may not be due to renal injury so much as elevation in creatinine without true kidney injury
- Small elevations secondary to diuresis in a patient who is clinically improving, the best course of management may be continuing diuresis if no other cause of the elevated creatinine is found