I reviewed Dr. Farkas’ IBCC chapter on acute exacerbation of COPD back in March of this year. But I reviewed the podcast again today. And I reviewed the show notes also. So I moved the post up to today and redid my excerpts.
In this chapter I link to and excerpt from the Acute Exacerbation Of COPD chapter of May 19 ,2020 from the Internet Book Of Critical Care [Link is to TOC] by Dr. Josh Farkas.
Here is the direct link to the COPD podcast and comments page.
Here are excerpts [These are direct links to the different sections of the Acute Exacerbations Of COPD chapter]:
CONTENTS
Continuing the excerpts from Dr. Farkas post:
diagnosis & workup
differential diagnosis
Patients with a history of COPD frequently present to the hospital with dyspnea. Most of them have AECOPD, but some don’t. The following are common differential diagnoses that should be considered, together with key diagnostic findings:
- Pneumonia. Key findings = consolidation on ultrasonography, infiltrate on CXR.
- Pulmonary embolism (PE). Key findings = lack of usual features of AECOPD (no sputum, no fever, etc.).
- Pulmonary edema. Key findings = bilateral B-lines on ultrasonography, signs of congestion on CXR.
- Pneumothorax. Key findings = loss of lung slide on ultrasonography, pneumothorax on CXR.
- Upper airway obstruction (e.g., tumor, angioedema, epiglottitis, vocal cord dysfunction). Key findings = wheeze/stridor grossly audible without stethoscope.
- Obesity hypoventilation syndrome: patients may present with hypercapnic respiratory failure, but without other findings of COPD (wheezing, sputum).
- Opioid/sedative effects: among COPD patients who are on chronic opioids, it can be extremely difficult sorting out whether hypercapnia is a medication side-effect or is due to underlying COPD. Ideally, chronic opioids should be avoided in these patients, unless the patient is on a comfort-directed plan of care (DNR/DNI).
basic diagnostic workup
- H&P
- The holy trinity:
- Ultrasonographic examination of heart & lungs
- CXR
- EKG
- Basic labs (CBC, electrolytes)
- Influenza PCR during flu season
- ABG/VBG?
- Generally unhelpful and unnecessary.
- Compared to ABG, VBG is generally fine & more humane. VBG may be obtained simultaneously with other labs.
- ABG/VBG doesn’t generally help diagnose AECOPD or differentiate it from other diagnoses (Burri 2011).
- ABG/VBG is helpful in the somnolent patient, to determine whether somnolence is caused by hypercapnia. [Emphasis added]
- Sputum GS/Cx is not helpful (discussed on section below regarding antibiotics).
AECOPD vs. PNA
- Hardest differential diagnosis to sort out (both may cause fever, chills, purulent sputum, and leukocytosis).
- Key differentiating factor is presence/absence of infiltrate. Unfortunately, chest x-ray isn’t 100% sensitive for pneumonia. In cases which are hard to tease apart, options include:
- Chest CT scan (although it is generally not worth getting a scan solely for this reason).
- Procalcitonin (if <0.5 ng/ml, this argues strongly against typical bacterial pneumonia).
- AECOPD and pneumonia often occur together (“pneumonic AECOPD” – the pneumonia is causing a COPD exacerbation). Treatment of pneumonic AECOPD consists of treating both pneumonia and COPD.
- One potential approach to a patient with COPD and possible pneumonia is the following:
- (1) Start on antibiotic coverage for pneumonia (e.g. ceftriaxone plus azithromycin) and check a procalcitonin.
- (2) If procalcitonin is low (<0.5 ng/ml), this argues against typical bacterial pneumonia. Ceftriaxone can be discontinued, while azithromycin is continued for treatment of COPD.
- (3) If procalcitonin is elevated, then continue combination antibiotic therapy for pneumonia (along with full-bore COPD therapy as well – the presence of PNA doesn’t exclude concomitant COPD).
AECOPD vs. PE
- PE is found in a small, but significant fraction of patients who present with possible AECOPD (~10%).
- PE should be suspected in patients whose presentation is atypical for a COPD exacerbation (e.g. lack of purulent sputum, fever, chills).
- For atypical AECOPD presentations, it is sensible to evaluate for PE.
- COPD patients are at low risk of harm due to contrasted CT scans (because their age makes radiation a nonissue and contrast dye doesn’t cause renal failure). The main risk of a CT scan is finding an incidental lung nodule which will trigger a cascade of iatrogenic harm.
key pathophysiologic concepts for management of COPD
#1) concept of “Flash AECOPD”
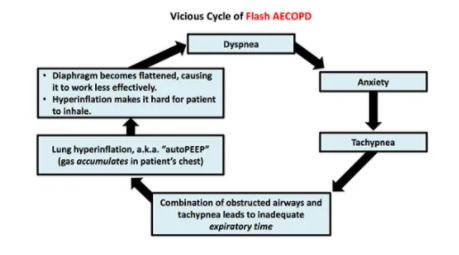
Patients with COPD and anxiety may fall into a cycle shown above with progressive anxiety, tachypnea, dyspnea, and gas trapping. This may cause patients to deteriorate very rapidly, but improve rapidly as well. A combination of BiPAP and anxiolytics may be very helpful in breaking patients out of an episode.
#2) concept of diaphragmatic rest
One of the central problems in AECOPD is exhaustion of the diaphragm. After working hard for a prolonged period of time, the diaphragm becomes fatigued. Diaphragmatic fatigue may require 24-48 hours of rest to recover. Probably one of the key roles of BiPAP or intubation is to rest the diaphragm. Take-home messages based on this concept:
- Even if the patient recovers well after a few hours on BiPAP, it may still be worthwhile to leave the BiPAP on longer (e.g. overnight) to rest the diaphragm.
- If a patient gets intubated for COPD, it is generally wise to leave them intubated for at least ~1 day before they are extubated (assuming that they truly required intubation in the first place).
basic treatments
steroid
- There is no precise evidence on how to dose steroid for COPD patients in the ICU. The following is a reasonable approach:
- (#1) Start with 125 mg IV methylprednisolone in the emergency department.
- (#2) If the patient remains on the verge of requiring intubation, then continue methylprednisolone 125 mg IV daily. Otherwise, proceed to…
- (#3) Prednisone 40-60 mg daily in the morning for a few days, then taper further.
- For patients who are improving and not at imminent risk of deterioration, don’t continue high steroid doses (e.g. 60 mg methylprednisolone IV Q6, which is equal to 300 mg/day of prednisone!).
bronchodilators
- Acutely ill patients are usually too breathless to take their home medications (metered-dose inhalers, etc.). Hold all home inhalers.
- The following regimen of bronchodilators is adequate:
- Albuterol plus ipratropium nebulized Q6hr scheduled.*
- *Duoneb Inhalation Solution – link is to the FDA label
- Albuterol nebulized Q2hr PRN.
- For patients on BiPAP or HFNC, bronchodilators can be nebulized and administered in-line through the device (without having to remove the patient from support).
antibiotics
- Patients sick enough to be in the ICU due to COPD should receive antibiotics (even if there is no infiltrate on the chest X-ray)(Vollenweider et al 2012).
- Patients with COPD have airways which chronically grow a variety of organisms. The goal of antibiotic therapy is generally to suppress this bacterial growth a bit, not to completely sterilize the patient’s lungs (which is impossible in this situation). Therefore, narrow-spectrum antibiotics are fine.
- Avoid getting sputum cultures and ignore them if they have been obtained (these patients will grow weird stuff in their sputum chronically; there is no need to cover every single organism)(Farkas et al 2010).
- Good choices include azithromycin or doxycycline.
- Azithromycin is generally first-line, if the patient hasn’t been exposed to it recently (don’t worry, it doesn’t cause Torsade de Pointes).
- Narrow antibiotics seem to be as effective as broader antibiotics, but may cause less Clostridioides difficile.
avoid excess oxygen
- Excess oxygen may cause diffuse pulmonary vasodilation, which disrupts ventilation-perfusion matching and thereby increases PaCO2 (Abdo WF et al 2012).
- Titrate inhaled oxygen to target an oxygen saturation of 88-92% (with 85-95% being OK).
noninvasive ventilatory strategies
indications for immediate intubation
- Immediate intubation is generally the wrong move. With strategic use of various medications and noninvasive modalities, intubation can very often be avoided.
- Indications for immediate intubation may include:
- Multiorgan failure (e.g. COPD plus cardiogenic/septic shock)
- A patient who is truly not protecting airway (e.g. gurgling secretions in upper airway)
- Respiratory/cardiac arrest
- When in doubt about intubation, a reasonable approach is often to prepare for intubation, while simultaneously placing the patient on BiPAP.
- If the patient improves, that’s great; you can avoid intubation.
- If the patient doesn’t improve, then BiPAP will still optimize their physiology prior to intubation.
BiPAP is the first-line noninvasive strategy
- BiPAP is supported by a very robust evidence base for the treatment of COPD. It has been proven to reduce death (relative risk 0.4), reduce intubation (relative risk 0.4), and reduce treatment complications (relative risk 0.3). This is impressive evidence which argues strongly that whenever possible, the patient should be given a real college try on BiPAP.
- Indications for BiPAP?
- Substantial respiratory distress or tachypnea (respiratory rate >~30/min).
- Somnolence due to hypercapnic encephalopathy, as a result of COPD exacerbation.
- Contraindications to BiPAP
- Need for immediate intubation (see above).
- Vomiting or increased risk of vomiting (e.g. bowel obstruction).
- Copious secretions, difficulty with secretion management.
- BiPAP settings
- Pressure: Start at 10cm iPAP/5 cm ePAP. If tolerated, may up-titrate as needed to ~18 cm iPAP/8 cm ePAP. Titrate the driving pressure (iPAP-ePAP) to achieve an adequate tidal volume. Whether to increase the ePAP slightly to cancel out autoPEEP (e.g. 8 cm) or whether to use 5 cm of ePAP is debatable and probably not clinically relevent.
- Monitor tidal volume & minute ventilation on the BiPAP monitor.
- Really low tidal volumes (e.g. <300-400 ml) and low minute ventilation (e.g. <5-6 L/min) suggest inadequate ventilation. In this situation try up-titrating the pressures and widening the driving pressure (with a rough maximum support level around ~20cm iPAP/5 cm ePAP).
what if the patient can’t tolerate the BiPAP mask?
- Don’t just assume that the patient needs to be intubated. The first step here is often to try some sort of sedation. If that fails, then the patient may be trialed on HFNC.
- Dexmedetomidine
- Excellent anxiolytic to help patients tolerate the mask and rest while on BiPAP. The combination of BiPAP plus dexmedetomidine is termed “BiPAPidex.” This is a powerful approach, especially for anxious patients with flash AECOPD (see figure above).
- Strength of dexmedetomidine is that it doesn’t suppress the respiratory drive and it’s titratable, making it the safest sedative.
- Weakness of dexmedetomidine is that it can take a little while to work. Boluses of dexmedetomidine can cause hemodynamic instability, so a reasonable approach may be to start the infusion at a high rate (1-1.4 mcg/kg/hr) and then titrate down as the patient becomes sleepy. This will take ~30-60 min to really work.
- Low-dose IV haloperidol or olanzapine is another option which may calm patients without suppressing respiratory drive or causing delirium.
- Benzodiazepines have mixed results here: occasionally they work, but they often cause the patient to get more confused/agitated. For patients who are on benzodiazepines chronically and respond well to this class of medication, this makes sense. In most cases I avoid benzodiazepines.
- Ketamine: For the acutely agitated patient this is a good option, with some bronchodilatory properties.
- Fentanyl: For patients with severe tachypnea and air hunger, small divided doses of fentanyl can be used to help them decrease their respiratory rate sufficiently to give them time to exhale properly (see: pathophysiology above). This must be done with very careful monitoring of minute ventilation & respiratory rate, by someone with extensive experience in treating respiratory failure. IV fentanyl is the way to go here because it works rapidly, so you can titrate it meticulously to hit a sweet spot where the patient is breathing at a rate of ~12-24 breaths/minute (fast enough to stay alive, but slow enough to allow sufficient time to exhale properly).
high-flow nasal cannula (HFNC)
- HFNC helps COPD patients mostly by reducing their anatomic dead space, improving ventilation, and reducing the work of breathing (“blowing off CO2” – more on the chapter on HFNC).
- There isn’t much evidence to support the use of HFNC in COPD (unlike BiPAP, which is supported by robust evidence). Thus, HFNC is currently a second-line therapy here.
- HFNC may be useful in the following situations:
- Patients who are unable to tolerate BiPAP.
- Patients in whom BiPAP is contraindicated (e.g. due to vomiting), but who aren’t sick enough to require intubation.
- Titration of settings:
- Flow rate should be maximized to the highest level that the patient will tolerate (ideally at least 50-60 liters/minute flow).
- FiO2 should be adjusted to target a saturation of 88-92% (accepting sats of 85-95%), as discussed above.
monitoring on BiPAP/HFNC
- Key parameters
- Oxygen saturation: Target saturation 88-92%, tolerate 85-95%. Excessive oxygen may impair VQ matching and thereby impair CO2 clearance.
- FiO2 requirement: COPD itself generally impairs CO2 clearance, but it shouldn’t cause profound hypoxemia. If the patient has escalating oxygen requirements, this suggests that something else is going on (e.g. pneumonia, mucus plugging, pulmonary embolism) – you need to investigate this further.
- Respiratory rate. Significant tachypnea (e.g. >~25-30 b/m) is a bad sign that the patient may eventually tire out. Ideally HFNC/BiPAP should cause a drop in respiratory rate.
- Work of breathing: Look for deterioration (e.g. retractions, abdominal paradoxical breathing, tripoding).
- BiPAP monitor: BiPAP allows you to monitor tidal volume & minute ventilation as described above. Note that a mask leak may cause these measurements to be imprecise.
- ABG/VBG or mental status
- If the patient has an intact mental status, I don’t think you need serial ABG/VBG values. If the patient is arousable and able to report how they are feeling, then just follow the clinical exam. Ideally the patient will report that they are feeling better. If the patient starts getting progressively more sleepy/confused, then you may be in trouble (check an ABG/VBG to exclude severe hypercapnia).
- If the patient is sedated, then you do need to follow ABG/VBG values to make sure the patient isn’t becoming dangerously hypercapnic (sedation prevents you from using mental status to exclude severe hypercapnia). While either ABG or VBG is fine, serial VBG monitoring using a peripheral vascular catheter that allows blood withdrawal is usually the most humane approach. More on ABG versus VBG differences here.
indications for delayed intubation