In this post, I link to and excerpt from Acute scaphoid fractures: guidelines for diagnosis and treatment [PubMed Abstract] [Full-Text HTML] [Full-Text PDF]. EFORT Open Rev. 2020 Feb 26;5(2):96-103.
All that follows is from the above excellent article.
Abstract
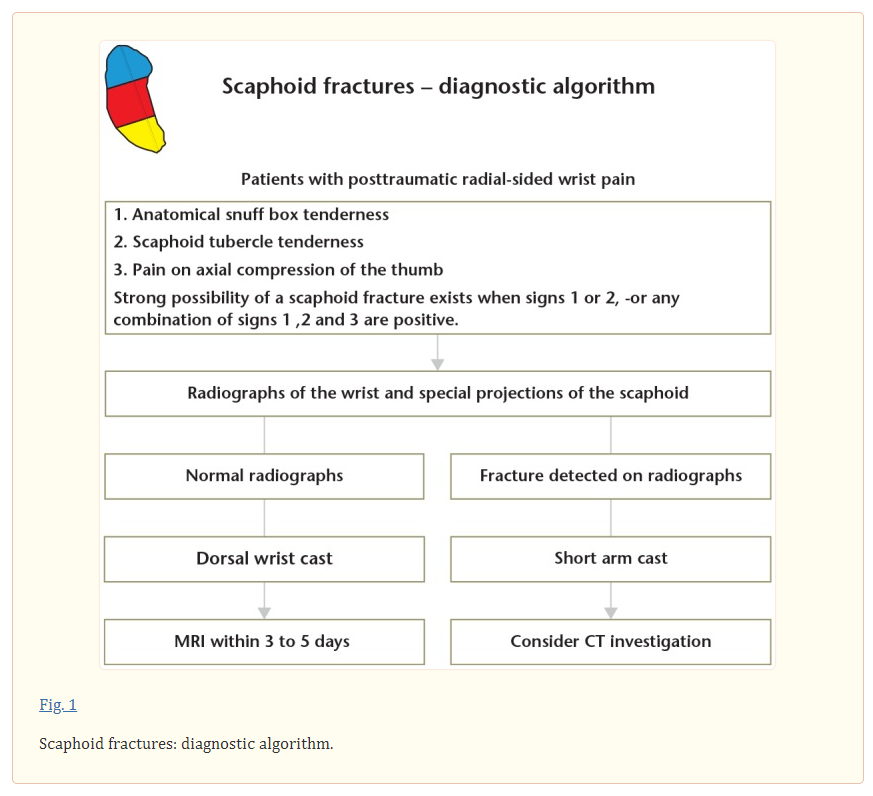
In cases of suspected scaphoid fracture where the initial radiographs are negative, a supplementary MRI, or alternatively CT, should be carried out within three to five days.
Fracture classification, assessment of dislocation as well as evaluation of fracture healing is best done on CT with reconstructions in the coronal and sagittal planes, following the longitudinal axis of the scaphoid.
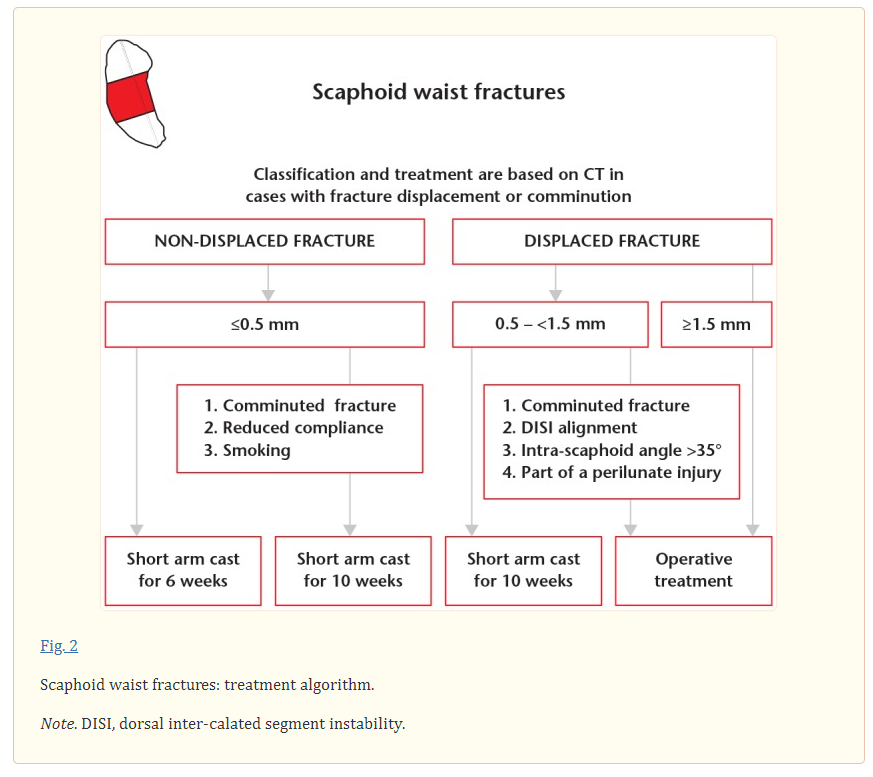
After adequate conservative management, union is achieved at six weeks for approximately 90% of non-displaced or minimally displaced (≤ 0.5 mm) scaphoid waist fractures.
Scaphoid waist fractures with moderate displacement (0.5–1.5 mm) can be treated conservatively, but require prolonged cast immobilization for approximately eight to ten weeks.
Internal fixation is recommended for all scaphoid waist fractures with dislocation ≥ 1.5 mm.
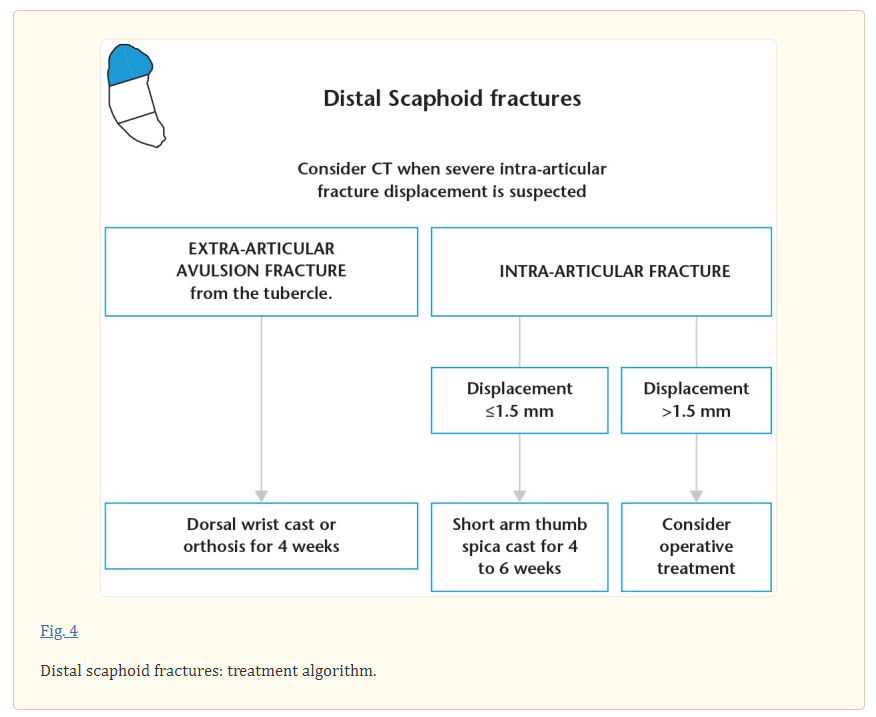
Distal scaphoid fractures can be treated conservatively. The majority heal uneventfully after four to six weeks of immobilization, depending on fracture type.
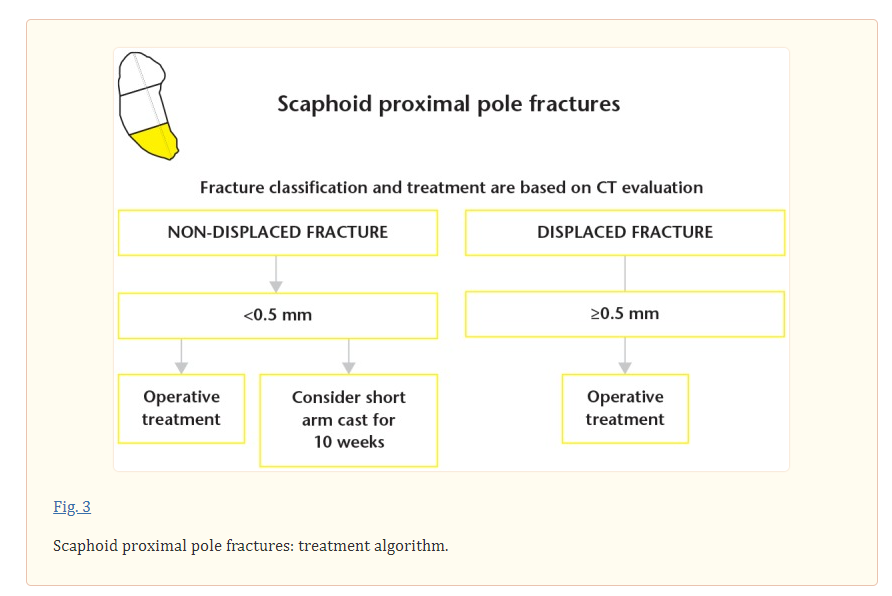
In general, proximal scaphoid fractures should be treated with internal fixation.
Cite this article: EFORT Open Rev 2020;5:96-103. DOI: 10.1302/2058-5241.5.190025
Keywords: internal fixation, non-operative treatment, scaphoid fractureIntroduction
Post-traumatic radial-sided wrist pain is common and can represent a fracture, wrist sprain, ligament disruption or a combination of injuries. Previous studies have shown that a scaphoid fracture is the most common fracture among patients with post-traumatic radial-sided wrist pain.1,2
It is well known that scaphoid fractures can be difficult to diagnose on initial radiographs. In cases of suspected scaphoid fracture where the initial radiographs are negative, magnetic resonance imaging (MRI) is recommended for diagnostics, while computed tomography (CT) has proven more reliable and accurate in the assessment of scaphoid fracture characteristics and union.7–9
The aim of this review is to present an algorithm for diagnosis and treatment of acute scaphoid fractures.
Diagnosis
Radiological investigation
A non-displaced or minimally displaced scaphoid fracture will only be detected if the X-ray beam is pointed parallel to the fracture line, which is why three to four special projections at difference angles of the scaphoid are recommended. However, the sensitivity of radiography to detect a scaphoid fracture is no higher than 70%.27
Traditionally, in cases of suspected scaphoid fracture where the initial radiographs are negative, patients had their wrist immobilized in a cast or splint for two weeks which was followed by repeated clinical and radiological examination. Consequently, this approach may lead to considerable overtreatment as in the end only 4–20% of cases are diagnosed with a fracture.13
As an alternative, several recent studies recommend MRI early on in cases of suspected scaphoid fracture, (Fig.1).2,9 With a sensitivity of 99–100%, it is cost effective to assure immediate diagnosis and adequate treatment.28 In addition, MRI can provide information on other fractures or ligament injuries in the affected wrist. Nonetheless, it is important to be aware that the difficulty of distinguishing a fracture from a bone bruise creates a potential risk for false-positive MRI scans.29
If MRI is not available, CT with a sensitivity of 93–95% is a reliable alternative.2
When a diagnosis is established, reliable fracture classification is mandatory to support the surgeon in deciding on treatment as well as to estimate prognosis. Radiographs have been demonstrated to be less reliable to describe fracture morphology and to evaluate displacement. However, CT with the possibility of coronal and sagittal plane reconstructions in the longitudinal axis of the scaphoid provides more detailed fracture characteristics and allows quantitative measurement of fracture gap, translation (step-off), and angulation given by the intra-scaphoid angle.8,32
At our institution, if a scaphoid fracture is presented as a hair-thin line on some radiographs but not necessarily all, or diagnosed by MRI only, we do not proceed with CT. However, if the fracture is clearly visible on the radiographs and displacement or instability is suspected, we recommend supplementary CT (Fig.1).
It is agreed that fracture displacement and/or instability is correlated with prolonged time to union and increased risk of non-union.33 Generally, signs of instability include: fracture displacement > 1 mm, DISI (dorsal inter-calated segment instability) scaphoid-lunate angle > 60 degrees, lateral intra-scaphoid angle > 35 degrees, fracture comminution and a scaphoid fracture as part of a perilunate injury.18,34 At our institution fracture displacement is categorized as: non or minimally displaced (≤ 0.5 mm), moderately displaced (0.5–1.5 mm) or severely displaced (≥ 1.5 mm).5,6,32
A strong correlation has been demonstrated between scaphoid fracture comminution in the form of a radial-sided cortico or cortico-spongeous fragment and arthroscopically verified fracture instability.35 However, while fracture displacement in the majority of cases indicates instability, instability may also be found in non-displaced fractures. Also, arthroscopically verified scaphoid-lunate (SL) ligament rupture may co-exist with a non-displaced scaphoid fracture in up to 25% of cases.36
Treatment
Before MRI
For patients with suspected scaphoid fracture where the initial radiographs are negative, major fracture displacement or instability is not expected. Consequently, we trust that immobilization in a dorsal wrist cast is sufficient until supplementary MRI has been carried out.
Negative MRI
In cases of post-traumatic radial-sided wrist pain and negative MRI, patients do not benefit from cast immobilization and can be mobilized early on.38 However, in such cases it is important to not overlook other wrist pathology such as intrinsic ligament injuries. Typically, radiologic signs of SL ligament rupture such as SL gap or DISI configuration may not appear until months after trauma. Even though contrast enhanced, high-field MRI may improve diagnostic sensitivity to detect intrinsic ligament injuries, arthroscopy is still considered the reference standard.39,40 A repeat clinical examination is advocated if symptoms have not diminished three to four weeks post trauma. If an SL ligament rupture is suspected, then surgery is recommended within six weeks post trauma.41
Scaphoid waist fractures
After adequate cast treatment, union is achieved at six weeks for approximately 90% of non or minimally displaced (≤ 0.5 mm) scaphoid waist fractures.5 Nevertheless, it is important to be aware that fracture comminution represented by a separate cortical or cortico-spongeous fragment on the radial side of the scaphoid, even in otherwise non-displaced fractures is associated with instability and prolonged time to union (Fig.2).5,35,42
The article has detailed information on the appropriate treatment of scaphoid waist fractures following the above Fig. 2. [Seven detailed paragraphs relevant to the treating orthopedic specialist. pp 98+99 of the PDF.]
Scaphoid proximal pole fractures
Proximal pole fractures have an inherent instability due to the small size of the fragment and an unbalanced linkage with the SL ligament on its dorsoulnar side only. Even so, there may be no ligament attachment at all depending on the orientation of the fracture line.55 The scaphoid following kinematics of both the proximal and distal carpal row leads to a large lever-arm stress affecting the proximal scaphoid especially during extension.56 Together with a tenuous blood supply, it predisposes proximal pole fractures to prolonged time to union and increased risk of non-union. Conservative treatment has been reported to result in a non-union rate of 10–14% for non-displaced fractures and as high as 50% for displaced fractures.57 A distinction between non-displaced and displaced fractures is crucial, which is why we recommend CT investigation for all proximal fractures and internal fixation if displacement is found (Fig.3). However, based on CT, a truly non-displaced fractures without signs of instability and not part of a high-energy trauma, can be considered for conservative treatment but with prolonged immobilization for 8 to 10 weeks (Fig.3).58
A volar surgical approach with the wrist in extension has an increased risk for displacement of a proximal pole fragment. Furthermore, it is difficult to securely engage the proximal fragment with the leading threads of the compression screw when inserted in the distal-to-proximal direction. Therefore, a dorsal approach is generally recommended.7 At our institution, we prefer a mini-open technique to visualize the fracture line as it allows a more precise screw placement as perpendicular to the fracture plane as possible. Also, it reduces the risk of extensor tendon damage. Small screw diameters such as 1.7 mm or 1.9 mm should be used to reduce the risk of splitting the fracture fragment. However, for the smallest fracture fragments of the proximal sixths of the scaphoid 0.8 mm or 0.9 mm K-wires may be the only possibility. There is no consensus regarding addition of bone grafting for internal fixation of acute proximal pole fractures.58,59
Distal scaphoid fractures
The distal third of the scaphoid is well vascularized, and fractures in this part of the scaphoid are often non or minimally displaced which has led to the current experience that these fractures heal uneventfully after conservative management.7 An avulsion of the radio-volar tip of the tuberosity with non or minimal articular involvement is the most common among this fracture type and accounts for more than 50% of all distal fractures.22,60 These fractures are sufficiently treated with four weeks of immobilization in a short arm cast or orthosis (Fig.4). The second most common fracture type of the distal scaphoid is an intra-articular fracture in the radial half of the joint surface caused by compression or shearing forces through the trapezium. A prolonged immobilization for four to six weeks is recommended (Fig.4). In rare cases, a comminute fracture pattern which involves the entire articular surface of the distal scaphoid is found. In such cases, we recommend a short arm cast with immobilization of the thumb for four to six weeks (Fig.4).
From radiographs it can be difficult to assess displacement and congruency of the distal articular surface; CT is therefore of value if fracture displacement is suspected. If severe displacement is found, operative treatment may be considered.
Assessment of fracture union
Bone union should always be assessed by combining clinical investigation of the wrist with radiological findings. Persistent pain over the fracture site may indicate incomplete or delayed union, but may also relate to an associated injury. Still, long-term anatomical snuff box soreness is not uncommon even years after a united scaphoid fracture.23,61
Scaphoid fractures unite by primary bone healing; with direct remodelling of lamellar bone, the Haversian canals and blood vessels, and without external callous formation.62,63 This is similar to other intra-capsular fractures. However, primary bone healing is difficult to visualize and evaluate on radiographs and limited by poor inter-observer agreement.64 CT with its higher spatial resolution and possibilities to reconstruct images in the longitudinal axis of the scaphoid, has been demonstrated as a more reliable method to assess bone union.65 At our institution, using 1 mm or 2 mm thick reconstructions in the coronal and sagittal planes along the longitudinal axis of the scaphoid, we define bone union as continuous trabecular bridging over more than 50% of the cross-section of the fracture site.5,6,65
With CT to evaluate bone union, 90% of all non or minimally displaced scaphoid waist fractures can be mobilized at six weeks.5,6 However, if bone union is < 50%, but no adverse features such as increased fracture displacement, fracture line sclerosis or cystic changes are identified, then cast immobilization should be prolonged repeatedly in four week periods until union is achieved.7 The vast majority of fractures unite within 10 to 12 weeks of continuous cast treatment, which must be weighed against the risk of surgical complications if early surgical intervention is considered.66 However, with doubtful or delayed union at 12 to 14 weeks a change in treatment strategy towards internal fixation is recommended.5,67
We believe, that if the patient is more or less pain free and CT demonstrates substantial bone union, no further radiological examination is needed. However, in those cases where pain in the scaphoid area has not evidently diminished, and CT despite bone contact leaves an uncertainty about trabecular bridging the fracture site, a repeat CT after three to six months should be considered.