In addition to today’s resource, please see and review the video of “Case Scenario: Peri-Anesthetic Management of Laryngospasm In Children” accessed 9-1-2021.
In this post I link to and excerpt from Anesthesiology‘s “Case scenario: perianesthetic management of laryngospasm in children” [PubMed Abstract] [Full-Text HTML] [Full-Text PDF]. Anesthesiology. 2012 Feb;116(2):458-71.
There are 86 similar articles listed in PubMed.
The above article has been cited by 11 articles in PubMed.
All that follows is from the above article.
PERIOPERATIVE laryngospasm is an anesthetic emergency that is still responsible for significant morbidity
and mortality in pediatric patients.1 It is a relatively frequent
complication that occurs with varying frequency dependent
on multiple factors.2–5 Once the diagnosis has been made,
the main goals are identifying and removing the offending
stimulus, applying airway maneuvers to open the airway, and
administering anesthetic agents if the obstruction is not relieved. The purpose of this case scenario is to highlight key
points essential for the prevention, diagnosis, and treatment
of laryngospasm occurring during anesthesia.Case Report
A 10-month-old boy (8.5 kg body weight) was taken to the
operating room (at 11:00 PM), without premedication, for
emergency surgery of an abscess of the second fingertip on
the right hand. Past medical history was unremarkable except
for an episode of upper respiratory tract infection 4 weeks
ago. The mother volunteered that he was exposed to passive
smoking in the home. He had been fasting for the past 6 h.
Preoperative evaluation was normal (systemic blood pressure
85/50 mmHg, heart rate 115 beats/min, pulse oximetry
[SpO2] 99% on room air). The procedure was expected to be
very short, and general anesthesia with inhalational induction and maintenance, but without tracheal intubation, was
planned. The child was placed over a forced air warmer (Bear
Hugger™, Augustine Medical, Inc., Eden Prairie, MN). Anesthesia was induced by a resident under the direct supervision of a senior anesthesiologist with inhaled sevoflurane in a 50/50% (5 l/min) mixture of oxygen and nitrous oxide. Two
min after loss of eyelash reflex, a first episode of airway obstruction with inspiratory stridor and suprasternal retraction
was successfully managed by jaw thrust and manual positive
pressure ventilation. An IV line was obtained at 11:15 PM,
while the child was manually ventilated. Anesthesia was then
maintained by facemask with 2.0% expired sevoflurane in a
mixture of oxygen and nitrous oxide 50/50%. Sufentanil (1
mcg) was given intravenously and the surgeon was allowed to
proceed 5 min later. At 11:23 PM, an inspiratory stridulous
noise was noted again. Manual facemask ventilation became
difficult with an increased resistance to insufflation and SpO2 dropped rapidly from 98% to 78%, associated with a decrease in heart rate from 115 to 65 beats/min. A new episode of laryngospasm was immediately suspected. Despite a jaw
thrust maneuver, positive pressure ventilation with 100%
O2, and administration of two bolus doses (5 mg) of IV
propofol (0.6 mg/kg), the obstruction was not relieved and
SpO2 decreased to 52%. A 0.2-mg IV bolus dose of atropine
was injected and IV succinylcholine was given at a dose of 16
mg, followed by tracheal intubation. Thereafter, surgery was
quickly completed, while tracheal extubation and postoperative recovery were uneventful.Epidemiology of Laryngospasm in Pediatric Patients
Children are more prone to laryngospasm than adults, with
laryngospasm being reported more commonly in children
(17.4/1,000) than in the general population (8.7/
1,000).2,5–7 In fact, the incidence of laryngospasm has been
found to range from 1/1,000 up to 20/100 in high-risk surgery (i.e., otolaryngology surgery).2,5–7 Many factors may
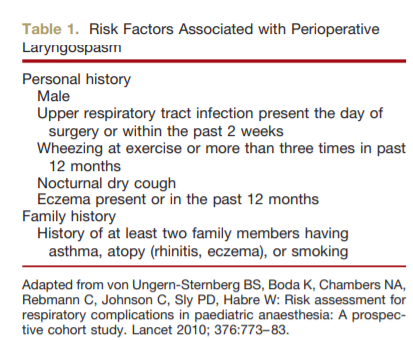
increase the risk of laryngospasm. These risk factors can be
patient-, procedure-, and anesthesia-related (table 1).Diagnosis of Laryngospasm in Children
The diagnosis of laryngospasm depends on the clinical judgment of the anesthesiologist. Laryngospasm is usually defined as partial or complete airway obstruction associated
with increasing abdominal and chest wall efforts to breathe
against a closed glottis.3,5,7 In both partial and complete
laryngospasm, signs of varying degrees of airway obstruction,
such as suprasternal retraction, supraclavicular retractions,
tracheal tug, paradoxical chest, and abdominal movements
may be seen.3 In addition, inspiratory stridor may be heard in
partial laryngospasm but is absent in complete spasm. In
addition, in complete laryngospasm, there is no air movement, no breath sounds, absence of movement of the reservoir bag, and flat capnogram.3 Finally, late clinical signs occur if the obstruction is not relieved including oxygen
desaturation, bradycardia, and cyanosis.3Treatment of Laryngospasm
Start here.