In this post, I link to and excerpt from Diagnosis of peripheral neuropathy [PubMed Abstract]* [Full-Text HTML] [Full-Text PDF]. Neurol Res Pract. 2020 Jul 15;2:20.
*There are links to 27 similar articles at this link as well as to four articles that cite the above resource in the PubMed Abstract.
All that follows is from the above resource.
Abstract
Introduction: Peripheral neuropathy represents a spectrum of diseases with different etiologies. The most common
causes are diabetes, exposure to toxic substances including alcohol and chemotherapeutics, immune-mediated
conditions, and gene mutations. A thorough workup including clinical history and examination, nerve conduction
studies, and comprehensive laboratory tests is warranted to identify treatable causes.First steps: The variability of symptoms allows distinguishing characteristic clinical phenotypes of peripheral neuropathy
that should be recognized in order to stratify the diagnostic workup accordingly. Nerve conduction studies are essential to
determine the phenotype (axonal versus demyelinating) and severity. Laboratory tests, including genetic testing, CSF
examination, nerve imaging, and nerve biopsy, represent additional clinical tests that can be useful in specific clinical
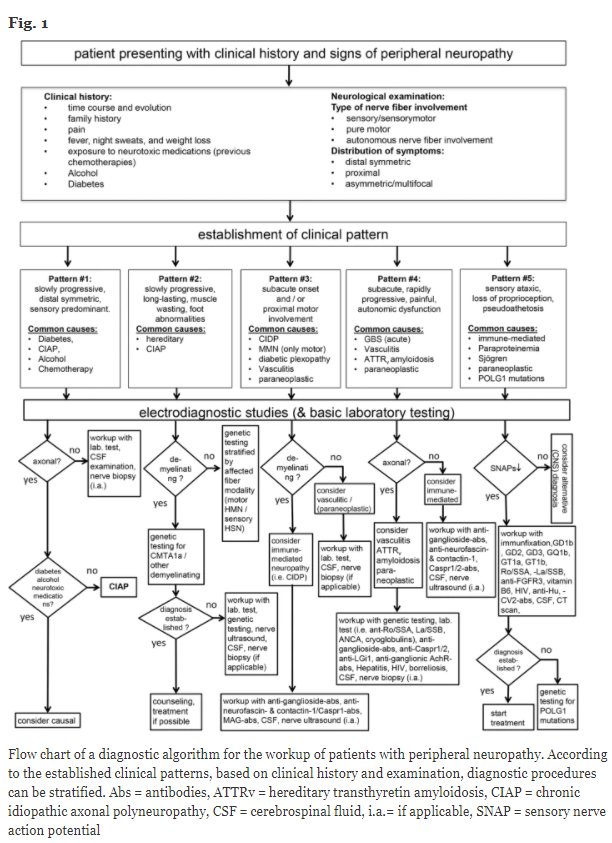
scenarios.Comments: We propose a flow chart based on five common basic clinical patterns of peripheral neuropathy. Based on
these five clinical phenotypes, we suggest differential diagnostic pathways in order to establish the underlying cause.Conclusions: The recognition of characteristic clinical phenotypes combined with nerve conduction studies allows pursuing subsequent diagnostic pathways that incorporate nerve conduction studies and additional diagnostic tests. This two-tiered approach promises higher yield and better cost-effectiveness in the diagnostic workup in patients with peripheral neuropathy.
Keywords: Peripheral neuropathy, Diagnosis, EMG, Nerve conduction studies, Hereditary amyloid transthyretin (ATTRv)
amyloidosis, Chronic Inflammatory Demyelinating Polyneuropathy (CIDP)* , Diabetic, Ultrasound
*Please see Diagnostic challenges in chronic inflammatory demyelinating polyradiculoneuropathy [PubMed Abstract] [Full-Text HTML] [Full-Text PDF]. Brain. 2020 Dec 5;143(11):3214-3224.
Introduction
Peripheral neuropathies are among the most common
neurological diseases with an incidence of 77/100,000 inhabitants per year and a prevalence of 1–12% in all age
groups and up to 30% in older people [1–3].The diagnosis of peripheral neuropathy necessitates a thorough workup of possible etiologies in order to identify treatable causes of this disease spectrum as early as possible.
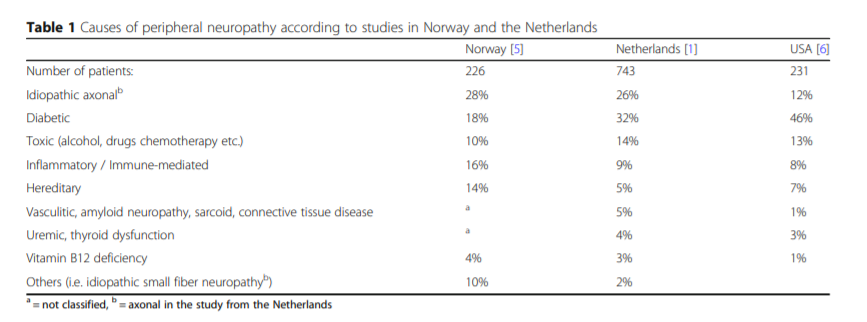
Hospital data-based epidemiological studies provide
(often differing) lists of most frequent causes of peripheral neuropathy in Western countries (Table 1).Importantly, patients may occasionally suffer from more than one disease causing their peripheral neuropathy. Clinically relevant cooccurrences are, for example, diabetes mellitus and
chronic inflammatory demyelinating polyradiculoneuropathy (CIDP), HIV infection and CIDP, or diabetes mellitus and chronic alcohol misuse.By focusing on the initial steps of the diagnostic workup, this standard operating procedure provides a practical guideline including clinical and additional diagnostic parameters that help to identify the underlying cause of peripheral neuropathy. Figure 1 provides a flow chart of this diagnostic workup.
First steps
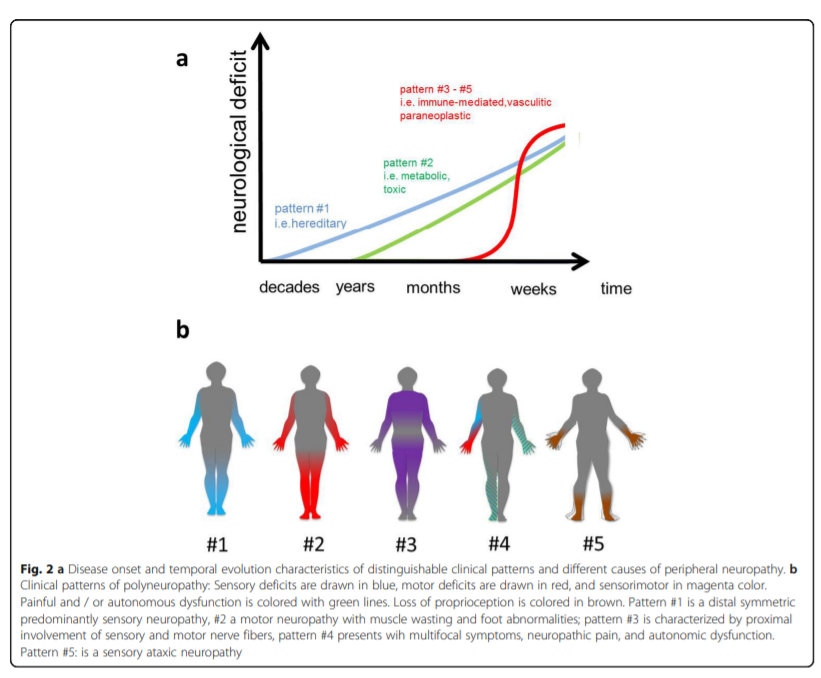
Recognizing specific clinical patterns is essential to stratify the diagnostic workup in a patient who presents with
signs and symptoms of peripheral neuropathy. This
workup should include a detailed history and a thorough
clinical examination. In our flow chart, we propose five
different clinical patterns:Start Here