In this post I link to and excerpt from Emergency Medicine Cases’ “Ep 159 Geriatric Trauma Part 1: The Under-Triaging Problem, Resuscitation, Airway, Head and C-spine Imaging, Clearing the C-spine“.*
*Helman, A. Wong, C. Haas, B. Tillman, B. Geriatric Trauma Part 1: The Under-Triaging Problem, Resuscitation, Airway, Head and C-spine Imaging, Clearing the C-spine. Emergency Medicine Cases. August, 2021. https://emergencymedicinecases.com/geriatric-trauma-under-triaging-resuscitation-airway-head-c-spine-imaging-clearing-c-spine. Accessed 8-27-2021.
All that follows is from this awesome podcast and show notes.
Just as pediatric patients are not small adults, geriatric patients are not just old adults. Here are a few facts: the oldest old are the fastest growing population in North America. Older adults with severe injuries represent at least 40% of all adults with severe injuries in the Canadian trauma system. Older patients are more likely to experience trauma and to have worse outcomes after a trauma. In this Part 1 of our 2-part EM Cases podcast series on Geriatric Trauma, Dr. Barbara Haas, Dr. Camilla Wong and Dr. Bourke Tillman answer questions such as: why are older patients under-triaged to trauma centers and how does that affect outcomes? What is the utility of the Shock Index in older patients? How should we adjust airway management for the older trauma patient? Which older patients do not require head or c-spine imaging after a ground level fall? Why is it challenging, yet of utmost importance, to clear the c-spine of a geriatric trauma patient as soon as possible? When can anticoagulation medications be safely resumed after an older person has sustained a minor head injury? and many more…
The problem of under-triaging geriatric trauma patients
Undertriage, both at the ED triage and to the lead trauma center, may be the single most important modifiable problem in trauma in older adults. In Ontario, >2/3 of older adults with major traumatic injuries (often related to minor mechanisms of injury such as ground-level falls) are triaged to a non-trauma center and <50% of these patients are transferred to a trauma center. Observational studies suggest as much as a 25% reduction in mortality, a reduction in delirium (51 vs 41%, P = 0.05) and fewer discharges to long term care (6.5% vs 1.7%, P=.03) when injured older patients are cared for at a lead trauma hospital. Trauma centers not only provide definitive surgical care, but they improve mortality and functional outcomes through access to multidisciplinary teams specialized in trauma care. Older patients with non-operative injuries also benefit from care at a lead trauma center. The lack of need for emergency surgery should not preclude consideration for transfer to a lead trauma center. Ground-level falls are are the most common mechanism of injury in older patients and carry a 10-fold higher mortality rate in older patients.
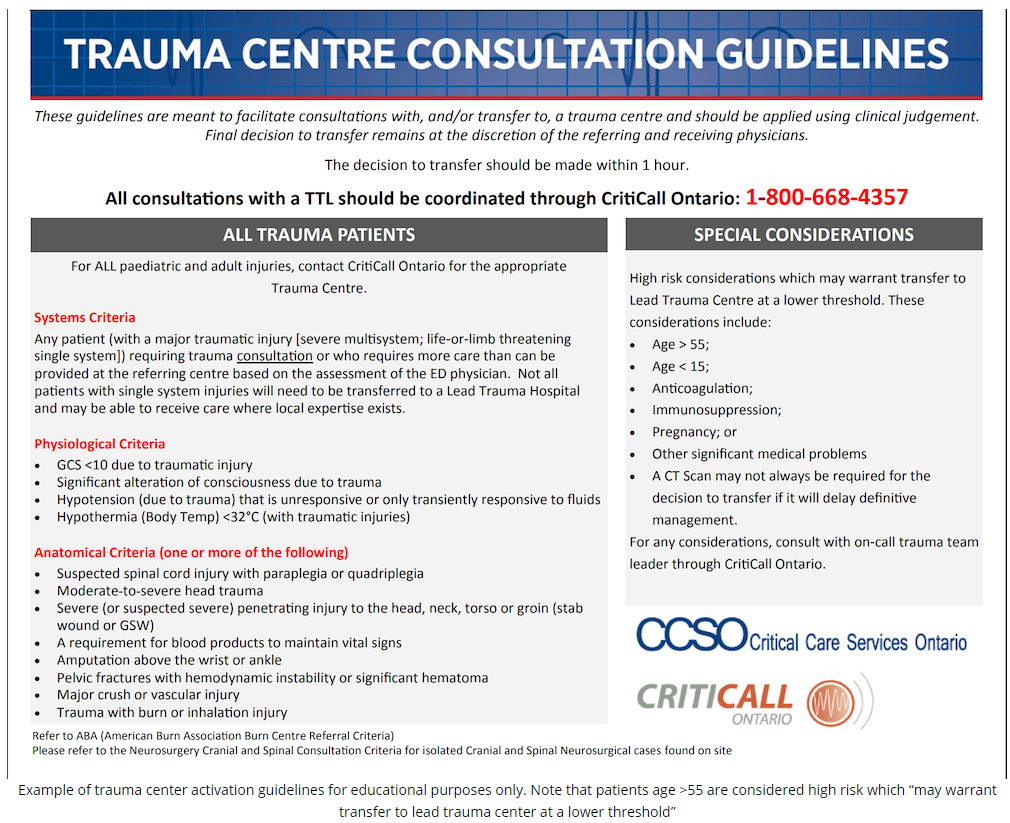
What can we do as emergency physicians to mitigate undertriage of older trauma patients? Be an advocate for your older trauma patients even if they have non-operative injuries, be familiar with your local trauma transfer guidelines (see below for example) and maintain a low threshold to transfer older trauma patients to a lead trauma center.
The lack of need for emergency surgery should not preclude consideration for transfer to a lead trauma center.
Anatomic and physiologic considerations in geriatric trauma care
- Comorbid disease, medications and frailty may all affect the expected physiologic presentation of trauma in older people
- Multiple studies have shown frailty* to be more predictive of poor outcomes than age after trauma
- Consider removal from backboard ASAP, measures to prevent hypothermia, being vigilant in maintaining c-spine precautions, more frequent assessments, acting on small changes in vital signs more readily, binding the pelvis early and placing an arterial line early
-
-
- For resources on the diagnosis and implications of frailty please see The Diagnosis Of Frailty And Its Implications
Posted on March 6, 2018 by Tom Wade MD
- For resources on the diagnosis and implications of frailty please see The Diagnosis Of Frailty And Its Implications
-
Hemodynamic considerations, the utility of the Age Shock Index (ASI) and fluid resuscitation
Normal vital signs in the elderly patient should not be considered as reassuring as they might be in younger patients. It is more challenging to recognize the early symptoms of shock in older patients owing to diminished physiologic reserve, chronic diseases that impair their ability to respond to injury, medications for cardiac conditions, e.g. antihypertensives, β-blockers, all of which may blunt a physiologic tachycardic response to stress or hemorrhage.
In patients with traumatic brain injury, the mean blood pressure target might better be 80 than the 60 we target in other patients, according to one of the speakers.
Concerning vitals in the geriatric trauma population:
- sBP <110 or sBP 40 less than baseline
- HR > 90
- RR < 10
Use Age-adjusted Shock Index (age x HR/SBP ) to augment (but not replace) clinical suspicion. It alone is not sensitive enough to rule out serious injury.
If age-adjusted shock index > 50: suspect shock or occult shock
Pitfall: A negative Age Shock Index should not be used as a rule out for significant injury
Other hemodynamic considerations include narrow window of normal volume status (patients are often volume deplete, however they are more sensitive to fluid overload). Be judicious with fluid resuscitation, use PoCUS as a tool to guide resuscitation and consider placement of an arterial line. While blood products are generally favoured over crystalloid in the hypotensive young trauma patient, our elderly trauma patients are often fluid deplete at baseline and may be on diuretics that further worsen their volume status. In the elderly trauma patient, it is reasonable to give a small bolus of crystalloid (250-500cc) and reassess their volume status during the initial resuscitation.
Pitfall: A common pitfall is to be dogmatic about volume resuscitation only with blood products in all trauma patients suspected of hemorrhagic shock. Do not dismiss crystalloids in geriatric trauma patients the way you might in younger patients; many older trauma patients are volume depleted at baseline.
Airway considerations in the geriatric trauma patient
Older patients often have multiple predictors of a difficult anatomic (dentures, restricted mouth opening, c-collar) and physiologic (low pulmonary reserve, underlying disease etc) airway . Endotracheal intubation carries a higher risk of complications in older patients such that the pros and cons should be carefully considered.
- Preoxygenation
- Lower physiologic pulmonary reserve, pre-oxygenate fully whenever possible
- Do a finger sweep to feel for dislodged dentures
- Dentures provide an excellent scaffold during pre-oxygenation/BVM, but may inhibit laryngoscopy; the timing of denture removal just prior to laryngoscopy when making the switch from BVM to ETT is important
- Airway equipment
- Consider hyperangulated videolaryngoscope + adjunct (bougie in all but grade 3b and 4 airways) given reduced c-spine and jaw mobility
- RSI medications dose adjustments
- Given higher risk of hypotension and slower distribution time, reduce dosages of induction agent (3/4 to ½ usual adult dose)
- Use higher dose of paralytic (eg. rocuronium 1.2mg/kg)
Neurologic considerations in the geriatric trauma patient
- Cognitive impairment and/or prior CVA may preclude a reliable assessment
- Older patients often demonstrate delayed neurologic signs of significant intracranial pathology due to cerebral atrophy
Pitfall: undertreating and overdosing analgesics in older trauma patients is a common pitfall. Both treating pain and proper dosing that is lower than ‘standard’ adult dosing of analgesics helps reduce the risk of delirium and agitation in these patients.
Common injury patterns in the geriatric trauma patient
Start here