In this post I link to and excerpt from CoreIM‘s podcast and show notes of Outpatient Advance Care Planning during COVID-19. Posted May 6, 2020. By: Dr. Jafar Al-Mondhiry, Dr. Amrapali Maitra and Dr. Mariah Robertson
Graphic: Gaby Mayer, Preeyal Patel
Audio: Julia Skubisz
Note to myself: This CoreIM podcast is, like all of their work, outstanding. The show notes beautifully summarize the podcast. However, the podcast and accompanying transcript, are great for reviewing in the car (podcast) or at home or office (transcript) to get all the nuances.
Here are direct links to the sections of the show notes:
Here are the excerpts:
Time Stamps
- 03:22 COVID Crisis as an Outpatient and Advance Care Planning (ACP)
- 08:06 The virtual visit
- 12:44 Vital Talk Mnemonic: “CALMER”
- 22:03 Challenges to Outpatient COVID Care
- 26:03 Parting Thoughts
Show Notes
COVID advanced care planning conversations as an outpatient:
- Nuanced ACP conversations with more branch points, as patients may think of a “COVID goals of care” vs. goals in non-COVID times
- Higher likelihood of high-risk patients getting sick
- Who to prioritize? One approach is to focus on elderly (age >80 years); comorbidities like obesity, hypertension, diabetes; other chronic conditions (metastatic cancer, renal disease on dialysis); and those with poor social support or who may not be in a situation to isolate.
Roadmap for outpatient ACP conversation
- Setup
- Potentially more access to patients and their support system through virtual visits during lockdown
- If possible, use video to get closer and build rapport. Opportunity to contextualize patients in their own environment, akin to a home visit.
- Bring healthcare proxy or family members into the conversation
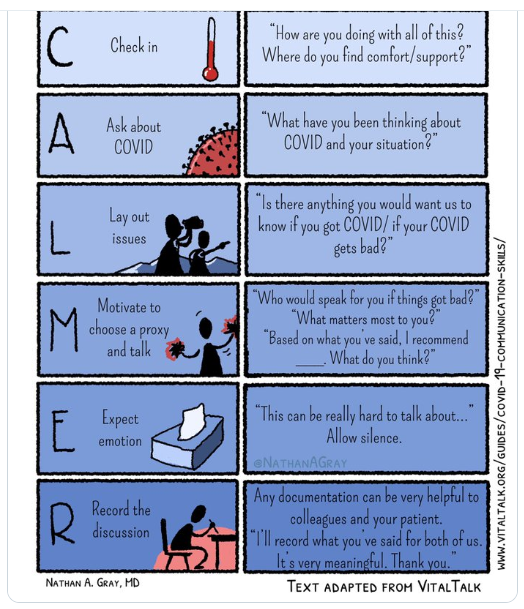
- Framework: CALMER (from VitalTalk)
Nathan Gray MD is very much worth following on Twitter and Instagram
@NathanAGray:
Palliative care doctor at Duke U : husband : foster parent : writer/cartoonist 🖍. Tweets and art are my own. IG: https://instagram.com/inkvessel/
Resuming show notes from the podcast:
- Check in: get the emotional temperature of the conversation
- “How are you doing with this whole pandemic?”
- Ask about COVID: request permission to dive into discussion on serious illness
- “Would it be okay if we talked more about what would happen if you were to get sick from this disease?”
- Lay out the issues: share your concerns about the patient’s risk factors that could contribute to poorer outcomes from COVID19
- Use language of hope and worry: “I hope that we can keep can keep you healthy and safe and out of the hospital, and I worry that if you got so sick that you needed a ventilator or CPR, your chances of leaving the hospital and getting back to how you’re feeling now would be low.”
- Motivate patient to explore goals and take steps
- Identify health care proxy and alternate
- Document phone numbers for these individuals in the chart
- Provide tools for patients to complete an Advance Directive
- Expect emotion
- Give a space for patients and families to process and to be vulnerable
- “I’m sorry, I know this can be hard to think about.”
- Record the conversation: documentation is key!
- Identify healthcare proxy, document code status if discussed, and highlight any specific considerations or language patients use
- The hidden “M”: Make a recommendation
- Use shared decision making by offering a medical plan that fits the patient’s values (see Inpatient GOC episode for more advice on making recommendations)
- Asking permission to do so: “Would it be okay if I make a recommendation based on what I am hearing?”
Documents to discuss with patients and help them fill out:
- Advance Directive: Legal document signed by patients that lists wishes regarding acceptable quality of life and specific medical care preferences during serious illness or end-of-life situation (e.g., feeding tubes, mechanical ventilation).
- POLST (Portable Order for Life Sustaining Treatment): Medical order signed by a clinician that conveys the same information in a direct way, including code status, hospitalization, etc. Physical piece of paper housed with patients and used in emergency situations. Should also scan a copy into the EMR, if available.
Additional challenges of outpatient ACP conversations with COVID19
- Patient resistance to having these conversations
- Remember, these can be ongoing discussions
- It is not our job to convince patients
- How to support patients whose goal is to remain out of hospital at all costs?
- See Center for the Advancement of Palliative Care (CAPC) COVID19 Response Resources Toolkit for medication guide for COVID19 symptom management at home
Conclusion: These conversations are tough, especially when we care so much about our patients and worry for them. We are all human, and things may not go perfectly despite our best intentions. Hopefully, we can find meaning in our work of supporting patients through this difficult time.
References and Resources
- American Heart Association (AHA): Cardiac Arrest Statistics https://cpr.heart.org/AHAECC/CPRAndECC/ResuscitationScience/UCM_477263_AHA-Cardiac-Arrest-Statistics
- American Society for Clinical Oncology (ASCO) Coronavirus Resources https://www.asco.org/asco-coronavirus-information?utm_medium=email&utm_source=TAPEN-+2020-0420
- Center for the Advancement of Palliative Care (CAPC) COVID-19 Toolkit https://www.capc.org/toolkits/covid-19-response-resources/
- POLST COVID-19 Resources https://polst.org/covid/
- VitalTalk COVID Ready Communication Playbook https://www.vitaltalk.org/guides/covid-19-communication-skills/
- PREPARE for your Care COVID-19 Resources https://prepareforyourcare.org/covid-19
- Center to Advance Palliative Care (CAPC) COVID-19 Response Resources https://www.capc.org/toolkits/covid-19-response-resources/
- ACP What Matters Most Workshop (online, for patients) https://www.eventbrite.com/e/what-matters-most-a-free-in-depth-advance-directive-workshop-registration-60629719122?aff=MERI
- Richardson, S., Hirsch, J. S., Narasimhan, M., Crawford, J. M., McGinn, T., Davidson, K. W., … & Cookingham, J. (2020). Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA.
- https://www.optimistic-care.org/docs/pdfs/NH_Advance_Care_Planning_During_a_Crisis.pdf
- https://www.capc.org/toolkits/covid-19-response-resources/
- https://polst.org