In this post, I link to and excerpt from PedsCases‘ Approach to Pediatric Bradycardia (Part 2) by Damian.Feldman-Kiss Dec 03, 2021.
All that follows is from the above resource.
This podcast is the second part of a two-part series on pediatric bradycardia. This episode will discuss high-quality cardiopulmonary resuscitation, list pharmacologic interventions used in management of pediatric bradycardia with a pulse and poor perfusion, list rhythms that are shockable and rhythms that are non-shockable in pediatric pulseless arrest, list the key investigations in workup of pediatric bradycardia, and list indications for pacing in chronic pediatric bradycardia. This podcast was developed by Damian Feldman-Kiss, a medical student at the University of British Columbia, under the supervision of Dr. Aisling Young, a pediatric cardiologist at Victoria General Hospital, and Dr. Karen Forbes, a pediatrician and medical educator at the University of Alberta.
Related Content
All that follows below is from Approach to Pediatric Bradycardia (Part 2) Script
PALS: Introduction
Before we discuss the steps of specific algorithms, there are a few important points to consider about PALS in general. The steps of PALS are presented as if there was a single rescuer; however, it is important to understand that PALS is a team effort and actions are performed simultaneously.1 Strong leadership, effective communication, organization, clear roles, and efficiency are integral to its success. Importantly, this podcast does not replace the need for formal training in PALS.
The most important part of PALS is high-quality cardiopulmonary resuscitation (CPR). The American Heart Association defines high-quality CPR as the following1
• A compression rate of at least 100 compressions per minute
• A compression depth of at least one-third of the anterior-posterior (A-P) diameter
of the chest (~4 cm in infants and ~5 cm in children)
• Allowing complete chest recoil between compressions
• Minimizing interruptions in compressions, and
• Avoiding excessive ventilationPALS Bradycardia Algorithm 1
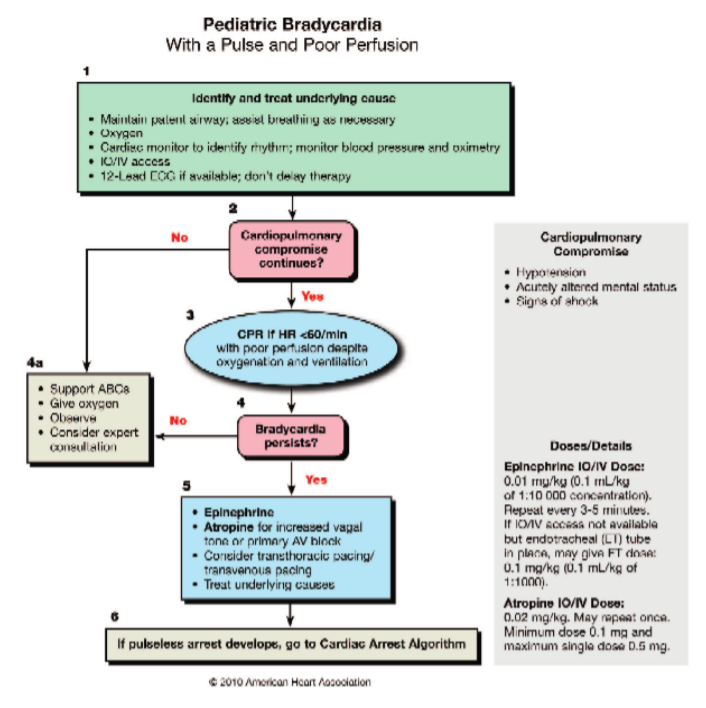
Let’s start with the PALS Bradycardia Algorithm. This algorithm is indicated for both infants and children with bradycardia, poor perfusion, and a palpable pulse. If, however, your patient no longer has a pulse at any time throughout the resuscitation, you must switch to the PALS Cardiac Arrest Algorithm. Also, throughout the entire algorithm, you must try to identify and treat the underlying cause of the bradycardia. Okay, let’s get
started. If you would like to follow along visually, see the script of this podcast for a
picture of the algorithm. The PALS Bradycardia Algorithm contains the following steps.PALS Bradycardia Algorithm, 2010 American Heart Association 1:
Step 1: Upon recognizing a patient with bradycardia, poor perfusion, and a palpable pulse, call a code and send for the crash cart. Then, assess the airway and keep it patent (e.g., you could use a head-tilt/chin-lift or jaw thrust). Administer 100% oxygen and, if necessary, support breathing. Once the crash cart arrives, attach the defibrillator pads so you can monitor the rhythm. It is very important to note that in this algorithm,
these pads are used for monitoring purposes only and not shock delivery. A regular cardiac monitor may be also be used if the crash cart is not readily available. Next, place a blood pressure cuff and pulse oximeter. Obtain intravenous (IV) or intraosseous
(IO) access and obtain a 12-lead ECG if available.Step 2: Reassess your patient. Is the monitor still showing bradycardia despite supporting their airway and breathing? What do they look like? For example, are they showing signs of cardiopulmonary comprise such as altered mental status? Do they appear shocky? Are they hypotensive?
If their ABCs are improving, further emergent treatment is not indicated, so skip ahead to step 4a.
Step 4a: continue to support their ABCs, monitor for any changes in status, and consult pediatric cardiology.
However, if supporting their airway and breathing do not improve the bradycardia and restore perfusion, proceed to step 3.
Step 3: Start high-quality CPR and perform for 2 minutes. For single-rescuer CPR, the compression to breath ratio is 30:2. For two-rescuer CPR, the compression to breath ratio is 15:2.
Step 4: After 2 minutes, reevaluate your patient. Again, what do they look like and what’s on the monitor? Are they altered, shocky, hypotensive, or bradycardic? Also, take this opportunity to ensure that their airway and breathing are being managed
adequately and that high-quality CPR is being performed. Don’t forget that CPR is exhausting, and rescuers must rotate giving compressions at least every 2 minutes.If their ABCs are improving, further emergent treatment is not indicated so, again, move on to step 4a—continue to support their ABCs, monitor for any changes in status, and consult pediatric cardiology.
However, if they are still compromised, continue airway management, ventilation, oxygenation, and high-quality CPR and proceed to step 5.
Step 5: The next step is to administer epinephrine. Epinephrine induces vasoconstriction and increases aortic diastolic pressure, which, in turn, increases coronary perfusion pressure. The dose is 0.01 mg/kg IV or IO* and can be repeated every 3 to 5 minutes.
*0.01 mg/kg of epinephrine is 0.1 mL/kg of 1:1oooo concentration of epinephrine.
If you’ve determined that the bradycardia is due to hypervagatonia or primary AV block, administer atropine. Atropine increases sinus and atrial automaticity and increases AV conduction velocity. The dose is 0.02 mg/kg IV or IO with a minimum dose of 0.1 mg and a maximum dose of 0.5 mg. In summary, the two medicines that can be used here are epinephrine and atropine. Importantly, shock delivery is NOT indicated in the
bradycardia algorithm. Remember, the patient has a pulse and an organized rhythm; the rhythm is just not sufficient to provide adequate cardiac output.At this point, if none of your interventions have improved your patient’s status, the next step is emergency transcutaneous or transvenous cardiac pacing. The transcutaneous method involves pacing the heart via chest pads, whereas the transvenous method involves pacing the heart via wires inserted into the venous system and advanced to the right heart. These temporary pacing techniques may save your patient’s life if the
bradycardia is secondary to sinus node dysfunction or complete AV block. At this point, consulting pediatric cardiology and pediatric critical care would be essential.PALS Cardiac Arrest Algorithm 1,2
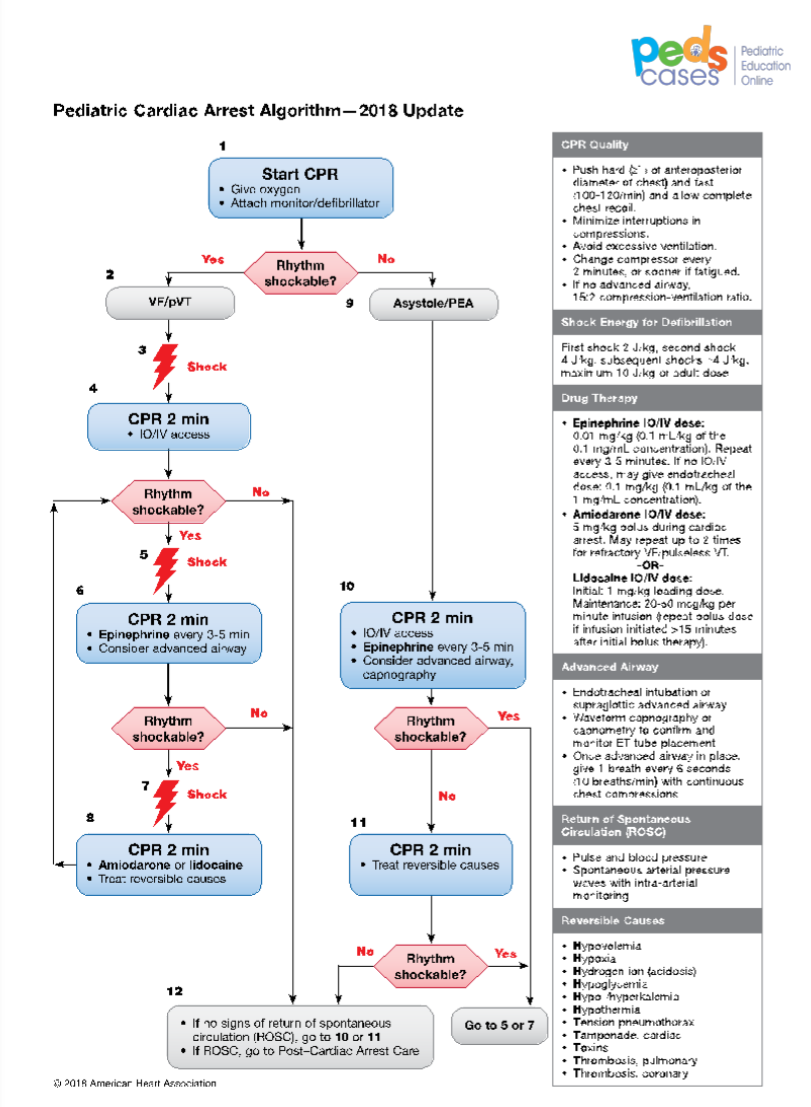
Okay, let’s move on to the PALS Cardiac Arrest Algorithm. This is the algorithm to follow if your patient does NOT have a pulse. It is slightly more complicated than the Bradycardia Algorithm because it contains two arms. The decision of which arm to follow depends on whether the rhythm is ‘shockable’. If the rhythm is shockable (i.e., the rhythm is ventricular fibrillation [VF] or pulseless ventricular tachycardia [pVT]), follow the steps on the left arm. If the rhythm is non-shockable (i.e., the rhythm is asystole or pulseless electrical activity [PEA]), follow the steps on the right arm. If at any point throughout this algorithm, a non-shockable rhythm becomes shockable, you must switch to the left arm and vice versa.
A key point that simplifies the decision of which arm to follow is that you do NOT need to differentiate between VF and pVT. If you see either of these rhythms, the rhythm is shockable. Likewise, you do NOT need to differentiate between asystole and PEA. However, this distinction will likely be more straightforward as asystole is a flatline and PEA is any organized electric activity without a palpable pulse. PEA most commonly has a slow rate and wide QRS complex.
Okay, let’s get started. Again, if you would like to follow along visually, see the script of this podcast for a picture of the algorithm. The PALS Cardiac Arrest Algorithm contains the following steps.
Step 1: Upon recognizing a patient in cardiac arrest (i.e., they are unresponsive, not breathing, and do NOT have a pulse), call a code, send for the crash cart, and begin high-quality CPR at 30:2 for single-rescuer CPR or 15:2 for two-rescuer CPR. Once the crash cart arrives, attach the defibrillator pads, and administer 100% oxygen. Next, determine whether the rhythm is shockable. If the rhythm is shockable (recall that means, VF or pVT) follow the steps on the left arm. If the rhythm is non-shockable (recall that means asystole or PEA), follow the steps on the right arm.
Let’s discuss the right arm first.
Step 9 to 11: Once you’ve decided that the rhythm is non-shockable, do not shock, of course, and continue high-quality CPR for 2 minutes. During this time, obtain IV or IO access, and consider an advanced airway (e.g., endotracheal intubation) andcapnography to monitor respiratory CO2 levels. Administer epinephrine IV or IO at 0.01 mg/kg* (max dose of 1 mg) and repeat every 3 to 5 minutes.
*0.01 mg/kg of epinephrine is 0.1 mL/kg of 1:1oooo concentration of epinephrine
Once an advanced airway is obtained, compressions need not be interrupted for ventilations. Compressions should then be continuous at a rate of at least 100 compressions per minute with the only interruptions for checking the rhythm and rotating the compressor role every 2 minutes or earlier to prevent fatigue. Ventilations should be given at a rate of 1 breath every 6 to 8 seconds, which is approximately 8 to 10 breaths per minute.
After 2 minutes of high-quality CPR, stop to check the rhythm. If the rhythm is non-shockable, continue cycles of high-quality CPR, epinephrine, and checking the rhythm every 2 minutes. Continue until spontaneous circulation returns (termed “return
of spontaneous circulation” or ROSC), which is noted by a palpable pulse, or your team decides to stop the effort. During this time, you should also be searching for and treating
reversible causes, which are the so-called H’s and T’s.[The Hs] include hypovolemia,hypoxia, hydrogen ions (i.e., acidosis),hypoglycemia, hypo or hyperkalemia,
hypothermia,[And the Ts include] tension pneumothorax, tamponade, toxins [ie medications like beta-blockers, calcium channel blockers and other drugs in overdose, and poisons such as insecticides, illicit drugs, etc] thrombosis of the lungs or heart.
However, if at any point the rhythm identified is shockable, meaning VF or pVT, charge the defibrillator to 2 J/kg, deliver a shock, and switch over to the left arm.
Now, let’s discuss the left arm.
See script to review details.
PALS: Summary
In summary, the most important part of PALS is high-quality CPR. The PALS Bradycardia Algorithm is indicated for both infants and children with bradycardia, poor
perfusion, and a palpable pulse.1 It focuses on reversing bradycardia. The PALS Cardiac Arrest Algorithm is indicated for patients who are unresponsive, not breathing, and who do not have a palpable pulse.1,2 It contains two arms. The left arm focuses on reversing VF or pVT, and the right arm focuses on reversing asystole or PEA. Remember that if you’re following the steps on the right arm and the rhythm becomes
shockable, you must switch to the left arm and vice versa. For more information on PALS, check out the PedsCases Podcast, “Pediatric Advanced Life Support”. Even better, sign up for a PALS provider course if it is within your scope of practice or training.Case: Resuscitation
After you finish reviewing PALS, EMS arrives and brings the patient into the trauma bay. The patient is a 14-year-old male with a past medical history significant for ADHD who took a toxic dose of his clonidine. He is bradycardic at 20 and has hypotension, respiratory depression, altered mental status, and weak pulses. Dr. Li assumes the team leader role and asks a respiratory therapist to assess the airway while two nurses set up the monitoring equipment and obtain IV access. Given the bradycardia, Dr. Li asks you to begin high-quality CPR. You and the respiratory therapist alternate 15 compressions and two breaths with a bag-valve-mask. After two minutes of CPR, you
and a nurse switch the compressor role, and the second nurse administers epinephrine. The bradycardia persists after two doses of epinephrine, so Dr. Li orders transcutaneous pacing. While the transcutaneous pacing is set up, Dr. Li reminds you
that since the patient had a palpable pulse throughout the resuscitation, you did not need to switch to the cardiac arrest algorithm and, therefore, did not need to consider
shock delivery. The transcutaneous pacing restores the patient’s heart rate and perfusion, and you and Dr. Li consult pediatric critical care.Case: Sharing Results and Next Steps
After helping out on the resuscitation, you debrief at the workstation and then visit Adrianne in her room. [the first case] You explain that her ECG demonstrated a problem with her
heart’s conduction system, which is the most likely reason for the syncopal episode. You explain that she will need to be admitted to the hospital and see a pediatric cardiologist.Back at the workstation, Dr. Li asks if you would like to practice your SBAR by calling pediatric cardiology. She reminds you that SBAR is a communication tool that stands for situation, background, assessment, and recommendation. It is an organized approach to communicating with your attending or a consultant over the phone.