In this post, I link to and excerpt from The Curbsiders‘ [Link is to complete episode list] #315 Long COVID with Dr. Monica Verduzco-Gutierrez. JANUARY 10, 2022 By DR BETH GARBITELLI.
All that follows is from this incredible resource.
Fatigue, cardiopulmonary, neuropsychiatric, and other long term effects following COVID-19 with Dr. Monica Verduzco-Gutierrez
Summary
Explore the actively evolving clinical landscape of Long COVID as we discuss epidemiology, pathogenesis, manifestations, and patient-centered management options including the role of a dedicated Long COVID clinic. Listen as our expert guest Dr. Monica Verduzco-Gutierrez @MVGutierrezMD (Long School of Medicine at UT Health, San Antonio) helps us navigate this rapidly emerging syndrome. This episode will empower you to provide evidence based, patient-centered care for this challenging facet of the ongoing COVID-19 pandemic. We explore the manifestations including fatigue, dyspnea, psychiatric symptoms, and other neurologic effects. We also examine the emergence of dedicated Long COVID clinics and the imperative of interdisciplinary care.
Credits
- Written and Produced by: Avital O’Glasser MD, FACP, SFHM
- Infographic: Edison Jyang
- Cover Art: Kate Grant, MBChB MRCGP DipGUMed
- Show Notes: Avital O’Glasser MD, FACP, SFHM
- Hosts: Matthew Watto MD, FACP; Paul Williams MD, FACP; Avital O’Glasser MD, FACP, SFHM
- Reviewer: Hannah Abrams, MD
- Executive Producer: Beth Garbitelli
- Showrunner: Matthew Watto MD, FACP
- Editor: Clair Morgan of nodderly.com
- Guest: Monica Verduzco-Gutierrez, MD
Long COVID Pearls
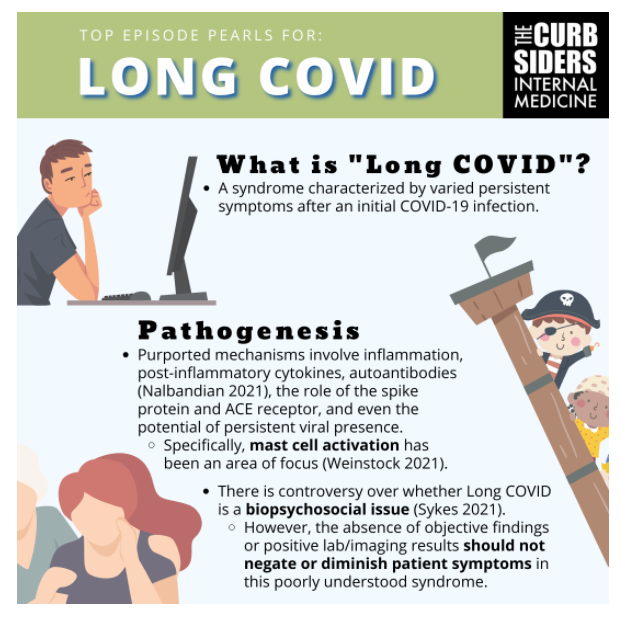
- “Long COVID” is the syndrome characterized by varied persistent symptoms after an initial COVID-19 infection. Different terms may be employed to describe this syndrome or constellation of symptoms after a COVID-19 infection.
- Pathogenesis of Long COVID is likely driven by individual immune responses, including post-inflammatory cytokines and mast cell activation. Research is needed regarding treatment.
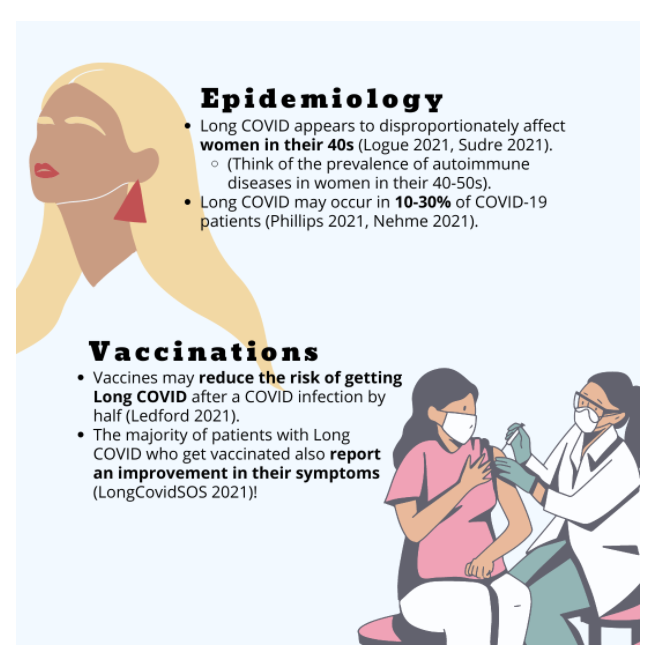
- Long COVID may affect 10-30% of people with COVID-19. Akin to autoimmune conditions, middle-aged women appear at highest risk for Long COVID.
- Long COVID research and care is best delivered by interdisciplinary teams.
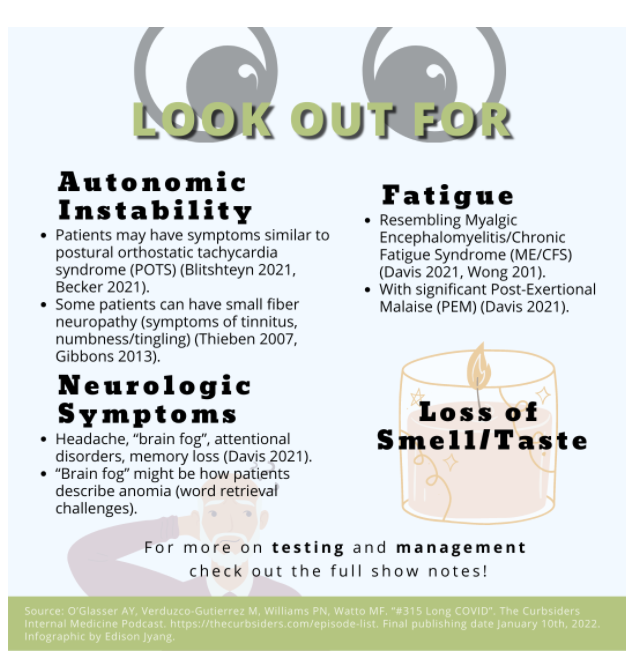
- Cardiovascular symptoms in Long COVID resemble postural orthostatic tachycardia syndrome (POTS).
- Fatigue and other systemic symptoms in Long COVID resemble chronic fatigue syndrome/myalgic encephalomyelitis and post-exertional malaise (PEM).
- Neuropsychiatric manifestations of Long COVID can be common and may need work accommodations as mental activity can trigger post-exertional malaise (PEM) in addition to physical activity.
- Smell training can be beneficial for anosmia.
- Patient validation, counseling, and education cannot be underemphasized in Long COVID.
- Long COVID qualifies for disability assessments according to the ADA.
- Vaccinate, vaccinate, vaccinate patients with Long COVID if they are otherwise eligible.
Long COVID
What’s in a Name?
“Long COVID” is the syndrome characterized by varied persistent symptoms after an initial COVID-19 infection. Different terminology and definitions currently exist. The CDC defines “Post-COVID Conditions” as an array of symptoms four or more weeks after being infected with COVID-19. In February 2021, the NIH announced the name PASC (Post-Acute Sequelae of SARS-CoV-2). In October 2021, the WHO released the first official definition of post COVID-19 condition, which includes the stipulation that these are symptoms that occur after confirmed or presumed COVID-19 infection. The definitions vary slightly in terms of time requirement for symptom onset and duration, but ultimately one should take a patient-centered approach to the fact that patients have new or persistent symptoms after a COVID-19 diagnosis.
The term “COVID Long Hauler” was an early patient-driven term, but this has fallen out of favor for many patients, per Dr. Verduzco-Gutierrez.
Pathogenesis
We do not have a definitive understanding of the pathophysiology of Long COVID yet, but purported mechanisms focus on the role of the individual immune response (Nalbandian 2021). This includes the presence of inflammation and post-inflammatory cytokines as well as the creation of autoantibodies. Research about the pathophysiology looks at the role of the spike protein and ACE receptor, as well as explores questions about the potential for persistent viral presence.
Mast cell activation is one area of focus for the mechanism of Long COVID (Weinstock 2021). Nearly a fifth of the population has a propensity for mast cell activation (Afrin 2017), which might act in synergy with a COVID-19 infection. Illness script for mast cell activation: “everything is a trigger” including allergies (as well as asthma), eczema, and/or gastrointestinal symptoms are now worse, and they may have a long list of medication allergies/intolerances. Dr. Verduzco-Gutierrez utilizes a mast cell protocol for patients with evidence of mast cell activation–this decreases histamine levels by avoiding triggers and adding pharmacotherapy.
Post-viral sequelae exist with other viral infections (including Ebola, MERS, SARS-CoV-1, West Nile Virus). Is post-COVID “just another” post-viral syndrome that we happen to be seeing on a very large scale right one given the large number of COVID-19 cases? Potentially!
Is there an emerging controversy that Long COVID is more of a biopsychosocial issue (Sykes 2021) versus a biological phenomenon (Phillips 2021)? As with other poorly understood syndromes, patients with Long COVID may feel that they are being gaslit, stigmatized, and told “it’s all in your head” especially if available tests are negative (Verduzco-Gutierrez 2021). As Dr. Verduzco-Gutierrez says, we might not have the right tests YET. The absence of objective findings or positive results on laboratory or imaging studies must not negate patients’ symptoms, and we need to look beyond the traditional tests in our wheelhouse and think outside the box by listening to our patients’ symptoms.
Epidemiology
Long COVID appears to disproportionately affect women in their 40s (Logue 2021, Sudre 2021), in comparison to older men being at risk for worse initial infection. Think of the prevalence of other autoimmune diseases in women in their 40-50s! The woman-predominance risks exacerbating the bias and misogyny affecting our ability to diagnose challenging symptoms –and we need to be prepared to LISTEN to our patients.
Long COVID may occur in 10-30% of patients who had COVID-19 (Phillips 2021, Nehme 2021). Given the number of COVID-19 cases in this country, Long COVID is being dubbed the next national health disaster (Phillips 2021) or “this generation’s polio”.
The impact of COVID-19 therapies (ex. steroids, monoclonal antibodies) on the risk of developing Long COVID is still being studied.
Interdisciplinary Care
Who “Owns” Long COVID or Long COVID Clinics?
The work surrounding Long COVID has been highly interdisciplinary so far! Physiatry has been heavily involved (Verduzco-Gutierrez 2021). Cool history: the field of Physiatry has strong historical roots in the polio epidemic, because polio created so many people who had new disabilities. Polio hospitals became rehab hospitals once the polio vaccination was widely available.
Dr. Verduzco-Gutierrez: “[Physiatry is] good at taking care of people during epidemics, but we’re best doing it with a team approach.”
Currently most of the clinical work for Long COVID is being done at academic centers and involves multiple specialties and subspecialties–ex., physiatry, internal medicine, cardiology, infectious disease, rheumatology, physical therapy, speech therapy, occupational therapy.
Testing, Manifestations, & Treatment Options
Autonomic Instability
Patients may have POTS-like symptoms or other signs/symptoms of autonomic instability (Blitshteyn 2021, Becker 2021). Tilt table testing may be needed after echocardiography; orthostatic vitals can also be checked in the clinic. Consider non-pharmacologic care including compression stockings, abdominal binders, small frequent meals, and proactive hydration per Dr. Dr. Verduzco-Gutierrez. Some patients might need pharmacologic therapy including beta-blockers or midodrine.
Patients with autonomic instability can have small fiber neuropathy (Thieben 2007, Gibbons 2013) (again, recall we might not have the right tests yet: EMG has lower sensitivity). Per Dr. Verduzco-Gutierrez symptoms can include tinnitus, numbness/tingling, or a sense of “internal vibration.”
Fatigue and other systemic symptoms
A phenotype of patients with Long COVID will resemble patients with Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) (Davis 2021, Wong 2021). ME/CFS patients can have significant Post-Exertional Malaise (PEM)(Davis 2021). Illness script for PEM: significant fatigue after physical or mental activity. Pacing and energy conservation is the hallmark of PEM management. Patients with Long COVID may need this type of approach rather than traditional physical therapy and exercise training (Rogers-Brown 2021). A consensus guideline on the assessment and treatment of fatigue in Long COVID was recently published (Herrera 2021).
Neurologic/Neuropsychiatric
Neurologic and psychiatric symptoms can be very common after COVID-19 (Taquet 2021). Some of the most common symptoms in Long COVID can be neurologic, including headache, “brain fog”, attentional disorders, or memory loss (Davis 2021). “Brain fog” might be how patients describe anomia (word retrieval challenges). However, anomia may be more multifactorial, with components from fatigue, inattention, and memory slips.
Pathophysiology may include disruption of the blood brain barrier, inflammation, and post-inflammatory cytokines (Moghimi 2021). Neuroinflammation causes neuropsychiatric symptoms, so analogies between Long COVID and “inflammaging” are valuable. It’s unclear if the virus itself might be found in the brain. Advanced brain imaging or advanced neuropsychiatric testing might be needed.
Apt analogies also exist between the neurologic manifestations of Long COVID and traumatic brain injury (TBI), post-concussive, and post-stroke syndromes. Focus on what you can optimize or treat. Example, optimize nutrition, exercise/activity, and sleep. Treat headaches. Consider vestibular rehab for dizziness. Consider speech therapy for cognitive support tools. Provide counseling and validate that cognitive tasks can be more fatiguing than physical activity after a brain injury–including potentially triggering PEM. Patients may need support and accommodations to return to work, including a graduated return to work program.
Loss of Smell/Taste
Cranial nerve 1 is the most common cranial nerve injured in TBIs (Fernandez Coello 2010)! Loss of smell/taste can persist for months (Carvalho-Schneider 2020); it can also progress to altered smell/taste. Treatment options include intranasal steroids and smell training. Otolaryngologists or certain non-medical professionals, like sommeliers, may have a role here. Consider the risk of malnutrition if smell/taste changes persist. Provide counseling and tips for personal safety, including working smoke detectors.
The Patient Voice & Community
In addition to professional support, there may be peer resources for patients with Long COVID, including internet or social media-based support groups. The VA developed the COVID Coach app.
Patients with Long COVID have been instrumental in the launch of Long COVID clinics and active research.
Vaccinations
Vaccines HELP! Vaccination may not be completely protective against the development of Long COVID, BUT vaccines may reduce the risk of getting Long COVID after a COVID infection by half (Ledford 2021). The majority of patients with Long COVID who get vaccinated also report an improvement in their symptoms (LongCovidSOS 2021). While a small percentage of patients with Long COVID will feel worse after vaccination, overall, the numbers favor vaccination, with the majority experiencing improved symptoms (LongCovidSOS 2021). Vaccination will lower the rate of a repeat COVID-19 infection after prior infection (super immunity).
Take Home Points
- BELIEVE patients and tell them you believe them.
- Provide support, education, and validation.
- Engage an interdisciplinary team to do as much as you can.
- Respect PEMs.
- Draw analogies to the treatment of POTS, PEMS, CFS/ME, and traumatic brain injury.
- Don’t forget about the disability paperwork.
Plugs
- Royal College of Occupational Therapists: Energy Conservation
- Fifth Sense
- AbScent
- Mobile App: COVID Coach
- NIH Recover Trial
Other Stuff
Glossary:
PASC: post-acute sequelae of SARS-CoV-2 infection
PICS: post-intensive care syndrome
POTS: postural orthostatic tachycardia syndrome
PEM: post-exertional malaise
ME: myalgic encephalomyelitis
CFS: chronic fatigue syndrome
TBI: traumatic brain injury