Here are links to and excerpts from Standards of Medical Care in Diabetes—2020 Abridged for Primary Care Providers [PubMed Abstract] [Full Text HTML] [Full Text PDF] from American Diabetes Association. Clinical Diabetes 2020 Jan; 38(1): 10-38.
I’m excerpting the figures and tables from the above article for my quick review [but the whole article is a short fast read]. And throughout the post there are links to each of the complete separate chapter in The [Complete] Standards of Medicare Care In Diabetes-2020 From the American Diabetes Association [Link is to the TOC]
This is an abridged version of the current Standards
containing the evidence-based recommendations
most pertinent to primary care. The recommendations,
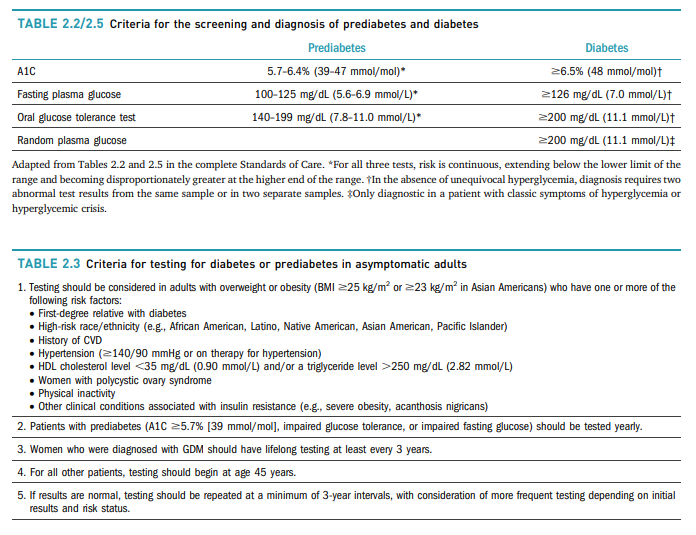
tables, and figures included here retain the same numbering used in the complete 2020 Standards and so are not numbered sequentially in this abridged version.* All of the recommendations included here are substantively the same as in the complete Standards. The abridged version does not include references. The complete 2020 Standards of Care, including all supporting references, is available at professional.diabetes.org/standards.*So if you want more information on a table go to that chapter in the Complete Standards [ex: For more on Table 2.2/2.5 or Table 2.3] go to 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes—2020.
Here are the introductory chapters
- Introduction: Standards of Medical Care in Diabetes—2020
- Professional Practice Committee: Standards of Medical Care in Diabetes—2020
- Summary of Revisions: Standards of Medical Care in Diabetes—2020
1. IMPROVING CARE AND PROMOTING HEALTH
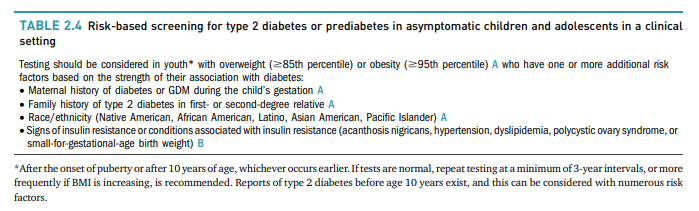
IN POPULATIONS [Link is to the section in The Complete Standards]2. CLASSIFICATION AND DIAGNOSIS OF DIABETES [Link is to the section in The Complete Standards]
3. PREVENTION OR DELAY OF TYPE 2 DIABETES [Link is to the section in The Complete Standards]
4. COMPREHENSIVE MEDICAL EVALUATION AND
ASSESSMENT OF COMORBIDITIES [Link is to the section in The Complete Standards]
5. FACILITATING BEHAVIOR CHANGE AND
WELL-BEING TO IMPROVE HEALTH OUTCOMES [Link is to the section in The Complete Standards]6. GLYCEMIC TARGETS [Link is to the section in The Complete Standards]
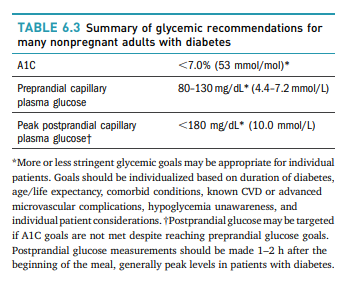
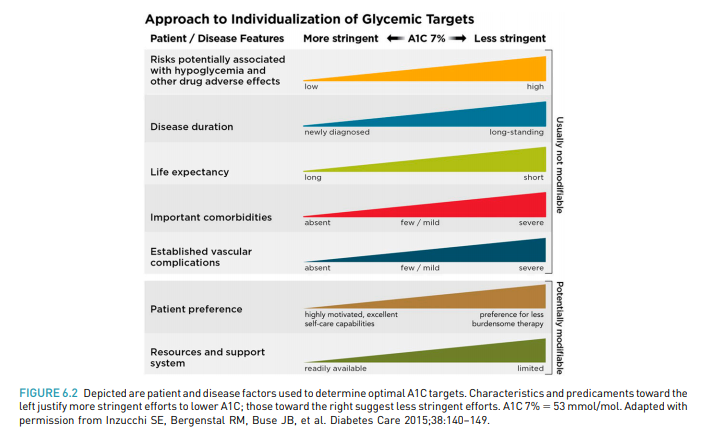
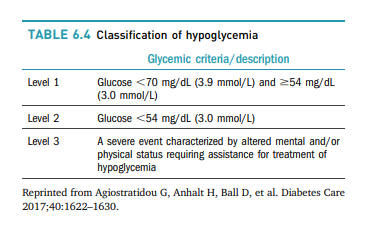
Assessment of Glycemic Control
Glycemic management is primarily assessed with the A1C
test, the primary measure studied in clinical trials
demonstrating the benefits of improved glycemic control.
Self-monitoring of blood glucose (SMBG) may help with
self-management and medication adjustment, particularly in individuals taking insulin. Continuous glucose
monitoring (CGM) also has an important role in assessing
the effectiveness and safety of treatment in many patients
with type 1 diabetes, and limited data suggest it may also
be helpful in selected patients with type 2 diabetes, such as
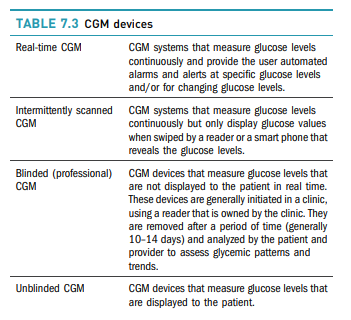
those on intensive insulin regimens.Glucose Assessment Using CGM
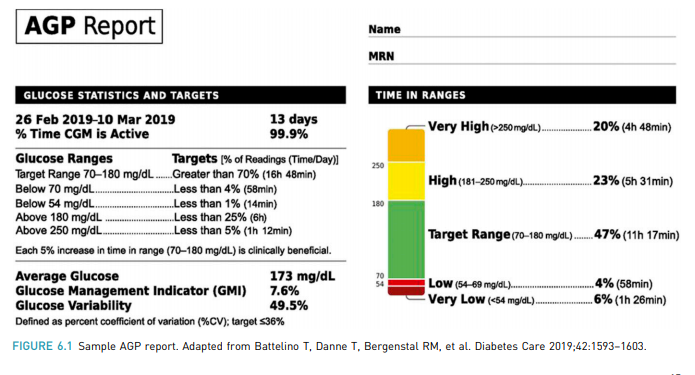
CGM has evolved rapidly in both accuracy and affordability.
To make CGM metrics more actionable, standardized
reports with visual cues such as the AGP (Figure 6.1) are
recommended and may help patients and providers interpret the data and use it to guide treatment decisions.
Diabetes technology describes the devices, software, and
hardware used to manage diabetes. It includes delivery
systems such as insulin pumps, pens, and syringes as well
as CGM devices and glucose meters. Newer forms of
diabetes technology include hybrid devices that both
deliver insulin and monitor glucose levels and software
that provides diabetes self-management support. Increased patient interest has increased the use of diabetes
technology in the primary care setting.
8. OBESITY MANAGEMENT FOR THE TREATMENT
OF TYPE 2 DIABETES [Link is to the section in The Complete Standards]There is strong evidence that treating obesity can delay the
progression from prediabetes to type 2 diabetes. It also has
been shown to be beneficial in the treatment of type 2
diabetes. Modest and sustained weight loss has been
shown to improve glycemic control and reduce the need
for glucose-lowering medications. Clinical benefits can be
seen with a minimum of 3–5% weight loss.9. PHARMACOLOGIC APPROACHES TO
GLYCEMIC TREATMENT [Link is to the section in The Complete Standards]Pharmacologic Therapy for Type 1 Diabetes
Recommendations
9.1 Most people with type 1 diabetes should be treated
with MDI of prandial and basal insulin or CSII. A9.2 Most individuals with type 1 diabetes should use
rapid-acting insulin analogs to reduce hypoglycemia
risk. A9.3 Patients with type 1 diabetes should be trained to
match prandial insulin doses to carbohydrate intake,
premeal blood glucose, and anticipated physical
activity. CSee “9. Pharmacologic Approaches to Glycemic
Treatment” in the complete 2020 Standards of Care for
more detailed information on pharmacologic approaches
to type 1 diabetes management.Pharmacologic Therapy for Type 2 Diabetes
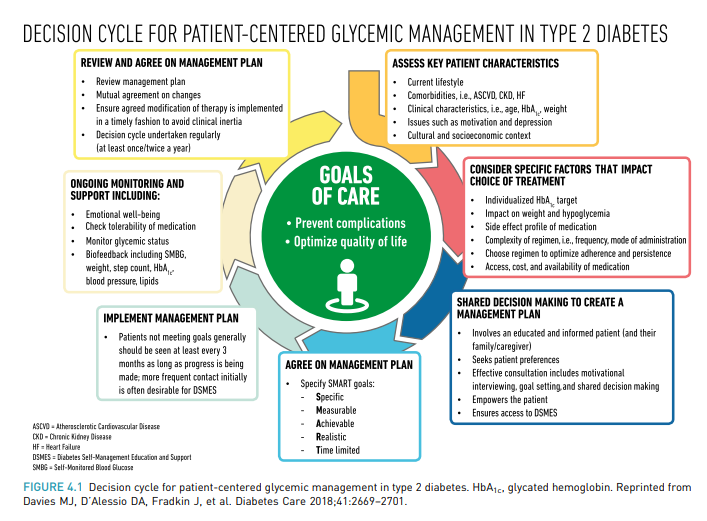
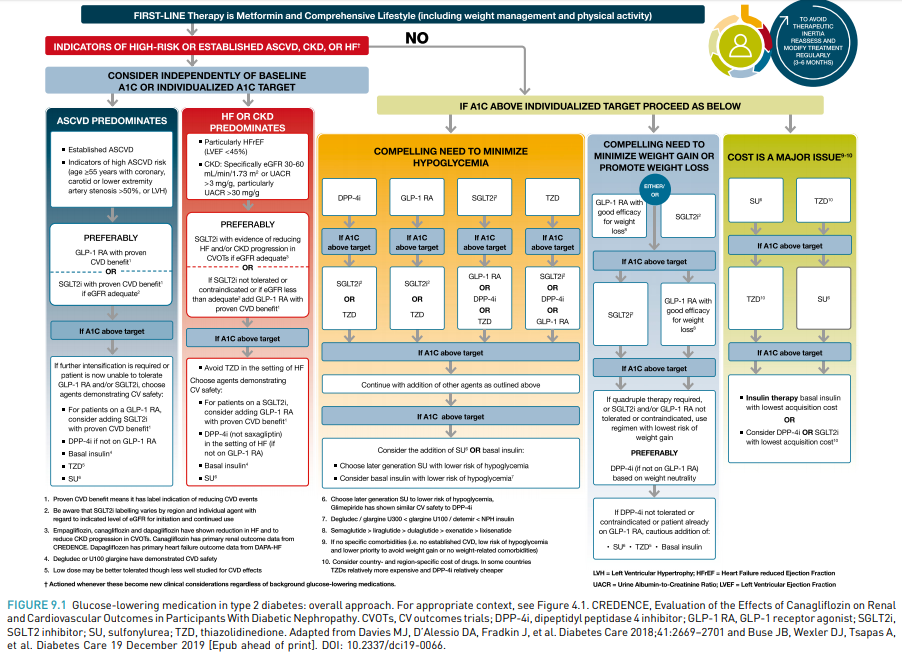
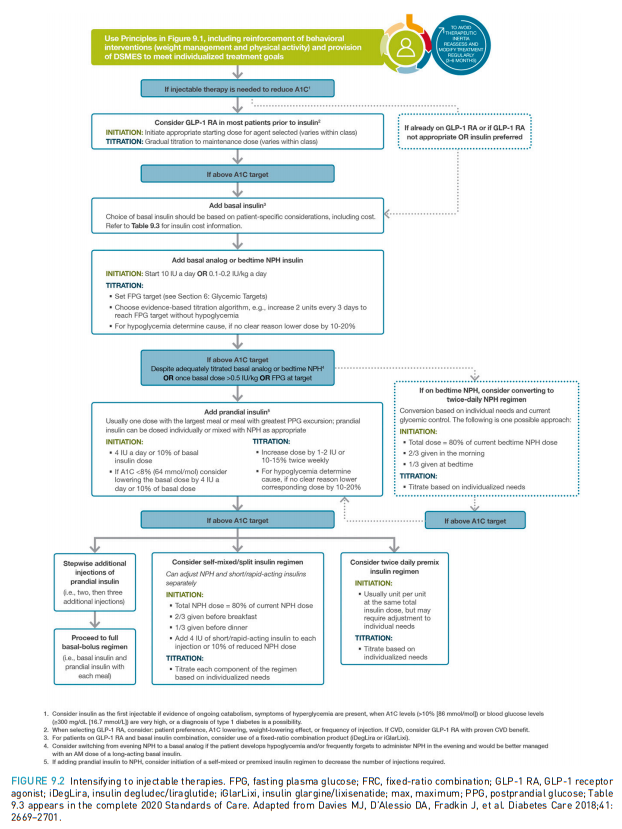
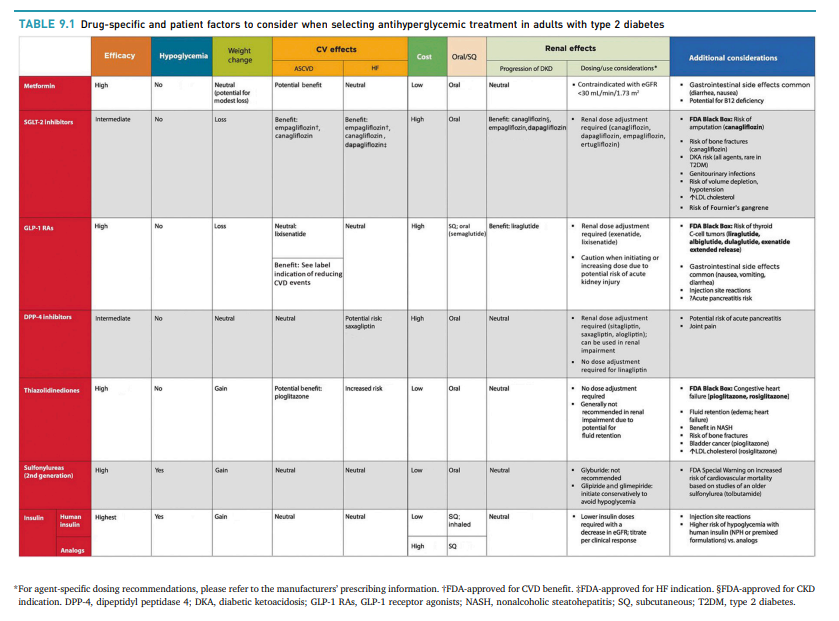
Figure 9.1, Figure 9.2, and Table 9.1 provide details for
informed decision-making on pharmacologic agents for
type 2 diabetes.**Figure 9.1, Figure 9.2, and Table 9.1 are much clearer in the PDF Standards of Medical Care in Diabetes—2020 Abridged
for Primary Care Providers
10. CVD AND RISK MANAGEMENT [Link is to the section in The Complete Standards]
These are my three 2020 posts on the recent Lipid Guidelines:
- 2020 Lipid Guidelines Review – Part 1 – The Curbsiders #191 Lipids Update And Cardiovascular Risk
- 2020 Lipid Guidelines Review – Part 2 – Links And Excerpts From “The 2018 AHA/ACC Guideline on the Managenent of Blood Cholesterol: Executive Summary”
- 2020 Lipid Guidelines Review – Part 3 – Links And Excerpts From “The 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk”
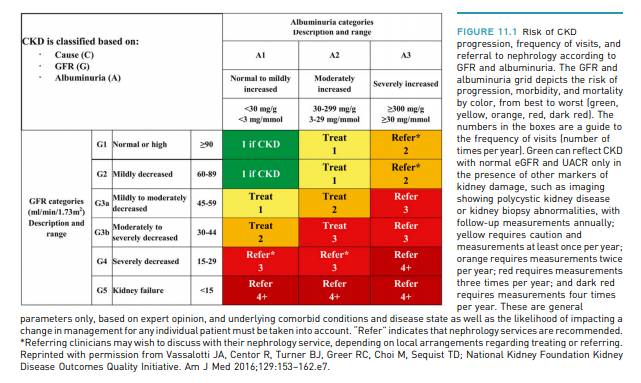
For prevention and management of both ASCVD and
HF, CV risk factors should be systematically assessed at
least annually in all patients with diabetes. These risk
factors include obesity/overweight, hypertension, dyslipidemia, smoking, a family history of premature coronary
disease, chronic kidney disease (CKD), and the presence
of albuminuria.The Risk Calculator
The American College of Cardiology/American Heart
Association ASCVD risk calculator (Risk Estimator Plus) is
a useful tool to estimate 10-year ASCVD risk calculator (Risk Estimator Plus) is a useful tool to estimate 10 year (tools.acc.org/ASCVD-Risk-Estimator-Plus). This calculator includes diabetes as a risk factor because diabetes itself confers increased risk for ASCVD.It should be acknowledged that this risk calculator does not account for duration of diabetes or the presence of diabetes complications such as albuminuria.
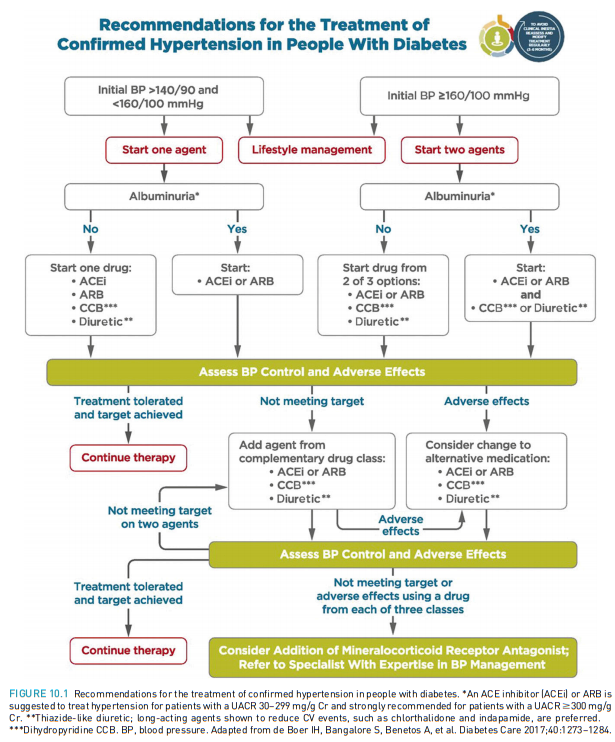
Hypertension/Blood Pressure Control
See also
- Links To The Latest European And American Hypertension Guidelines
Posted on February 27, 2019 by Tom Wade MD - 1 – Definition And Measurement Of High Blood Pressure – Extracts From The New 2017 Hypertension Guidelines
Posted on November 23, 2017 by Tom Wade MD- The above post has links to two good podcasts on the subject from the American College of Cardiology and
- Links to nine posts that contain excerpts from the 2017 Guidelines.
11. MICROVASCULAR COMPLICATIONS AND
FOOT CARE [Link is to the section in The Complete Standards]
12. OLDER ADULTS [Link is to the section in The Complete Standards]
13. CHILDREN AND ADOLESCENTS [Link is to the section in The Complete Standards]
The management of diabetes in children and adolescents
cannot simply be derived from care routinely provided to
adults with diabetes. The epidemiology, pathophysiology, developmental considerations, and response to
therapy in pediatric-onset diabetes are different from
adult diabetes.14. MANAGEMENT OF DIABETES IN PREGNANCY [Link is to the section in The Complete Standards]
The prevalence of diabetes in pregnancy is increasing
in the U.S. along with the epidemic in obesity seen
worldwide. Type 1 and type 2 diabetes are increasing
in women of reproductive age, and there also has
been a dramatic increase in rates of GDM. Diabetes
confers an increase maternal and fetal risk. Specific
risks of diabetes in pregnancy include spontaneous
abortion, fetal anomalies, preeclampsia, fetal demise,
macrosomia, neonatal hypoglycemia, hyperbilirubinemia,
and neonatal respiratory distress syndrome, among others.
In addition, diabetes in pregnancy may increase the risk of obesity, hypertension, and type 2 diabetes in offspring later
in life.15. DIABETES CARE IN THE HOSPITAL [Link is to the section in The Complete Standards]
Among hospitalized patients, both hyperglycemia and
hypoglycemia are associated with adverse outcomes,
including death. Therefore, careful management of inpatients with diabetes has direct and immediate benefits.
When caring for hospitalized patients with diabetes,
consult with a specialized diabetes or glucose management team when possible.16. DIABETES ADVOCACY [Link is to the section in The Complete Standards]
For a list of ADA advocacy position statements, including
“Diabetes and Driving” and “Diabetes and Employment,”
see “16. Diabetes Advocacy” in the complete 2020
Standards of Care.INDEX [Link is to the section in The Complete Standards]