Three additional resources: A quick Google search, “guidelines for the evaluation of subjective cognitive decline” showed a number of articles including [After reviewing these three articles on 7-8-2023, I did not find any of the three clinically helpful–so don’t reread.]
- Association of CSF, Plasma, and Imaging Markers of Neurodegeneration With Clinical Progression in People With Subjective Cognitive Decline [PubMed Abstract] [Full-Text HTML] [Full-Text PDF]. Neurology. 2022 Mar 29; 98(13): e1315–e1326. doi: 10.1212/WNL.0000000000200035
- I did not find this article clinically helpful. 7-8-2023
- Evaluating measurement properties of subjective cognitive decline self-reported outcome measures: a systematic review [PubMed Abstract] [Full-Text HTML] [Full-Text PDF]. Syst Rev. 2022; 11: 144. Published online 2022 Jul 18. doi: 10.1186/s13643-022-02018-y
- The conclusion from the Abstract: “Our findings suggest that available SCD questionnaires lack content validity evaluation. Currently available measurements of SCD lack development and validation standards. Further work is needed to develop and validate SCD self-reported measurement with good quality measurement properties.”
- ATN classification and clinical progression in subjective cognitive decline The SCIENCe project [PubMed Abstract] [Full-Text HTML] [Full-Text PDF]. Neurology. 2020 Jul 7;95(1):e46-e58. doi: 10.1212/WNL.0000000000009724. Epub 2020 Jun 10.
- I did not find this article clinically helpful.
In this post*, I link to and excerpt from Subjective Cognitive Decline — A Public Health Issue from the Centers For Disease Control And Prevention, accessed 7-7-2023.
*In this post, I simply copy the above CDC web page. I do this because it helps fix the information in my memory and I can easily find the resource using my blog’s search function. Readers should go to the CDC web page.
All that follows is from the above resource.
Available for Download pdf icon[PDF – 2 MB]
Subjective Cognitive Decline (SCD) is the self-reported experience of worsening or more frequent confusion or memory loss.1,2 It is a form of cognitive impairment and one of the earliest noticeable symptoms of Alzheimer’s disease and related dementias.2,3 SCD can have implications for living with and managing chronic disease, or performing everyday activities like cooking or cleaning.2 Because SCD is self-reported, it does not imply a diagnosis of cognitive decline by a health care professional.1,2
Cognition is a combination of processes in the brain that includes the ability to learn, remember, and make judgments.1 When cognition is impaired, it can have a profound impact on an individual’s overall health and well-being.1 Cognitive decline can range from mild cognitive impairment to dementia, a form of decline in abilities severe enough to interfere with daily life.1 Alzheimer’s disease is the most common form of dementia.1-3
Some cognitive decline can occur as adults age, but frequently forgetting how to perform routine tasks, for example, is not a normal part of aging and can affect a person’s ability to live and function independently. Some people with cognitive decline may be unable to care for themselves or perform activities of daily living, such as meal preparation, managing medical appointments, or managing their personal finances. Limitations in cognitive ability may impact a person’s ability to effectively manage medication regimens which can result in poor health outcomes of comorbid chronic diseases like heart disease or diabetes. By educating people about modifiable risk factors, encouraging early assessment and intervention, and understanding its impact on adults and their families, the health and well-being of many older adults may be improved.1,2
Subjective Cognitive Decline is self-reported confusion or memory problems that have been happening more often or getting worse in the past 12 months.4
By acting quickly and strategically to stimulate needed changes to systems and environments, public health professionals can work to mitigate future impacts of SCD as well as Alzheimer’s disease and related dementias on the health and wellness of the public.
Subjective Cognitive Decline is a Growing Public Health Issue
With the growing older adult population and the related increase in the need for health and social services, the public health community is challenged to be proactive. By acting quickly
and strategically to stimulate needed changes to systems and environments, public health professionals can work to mitigate future impacts of SCD as well as Alzheimer’s disease and related dementias on the health and wellness of the public. This is particularly important as these issues can impact not only older adults but also their family and friends who act as caregivers.This brief examines the following questions:
- What percentage of adults live with SCD?
- What percentage of adults with SCD live alone?
- What percentage of adults with SCD have discussed their memory loss or confusion with a health care professional?
- What percentage of adults with SCD experience coronary heart disease (including angina and myocardial infarction) or strokes?
- What percentage of adults with SCD also have other chronic diseases?
- What percentage of adults with SCD also report issues with their mental health?
- What percentage of adults with SCD have difficulty with everyday activities, like cooking, cleaning, or with work or volunteering?
SCD data presented in this brief were collected from communitydwelling adults aged 45 years and older in 2015-2017 through the Behavioral Risk Factor Surveillance System (BRFSS).4
Questions related to SCD were administered as part of the BRFSS in 49 states, the District of Columbia and Puerto Rico. For states administering the module during multiple years, and the most recent data were used for this brief. Additional results for these data were previously published.5 Additional data reports can be generated and viewed at the CDC Alzheimer’s Disease and Healthy Aging Data Portal.
These data were examined in two age groups, adults 45-64 years and 65 years of age and older, as well as by sex, race, Hispanic ethnicity, chronic disease status, and other demographic characteristics.
- The prevalence of subjective cognitive decline (SCD) is 11.1%, or 1 in 9 adults.
- The prevalence of SCD among adults aged 65 years and older is 11.7% compared to 10.8% among adults 45-64 years of age.
- The prevalence of SCD is 11.3% among men compared to 10.6% among women.
- The prevalence of SCD differs among racial/ethnic groups, 10.9% of Whites report SCD compared to 12.8% of Blacks/African Americans, 11.0% of Hispanics, and 6.7% of Asians and Pacific Islanders.
- Lower prevalence of SCD is reported in adults with more years of formal education.
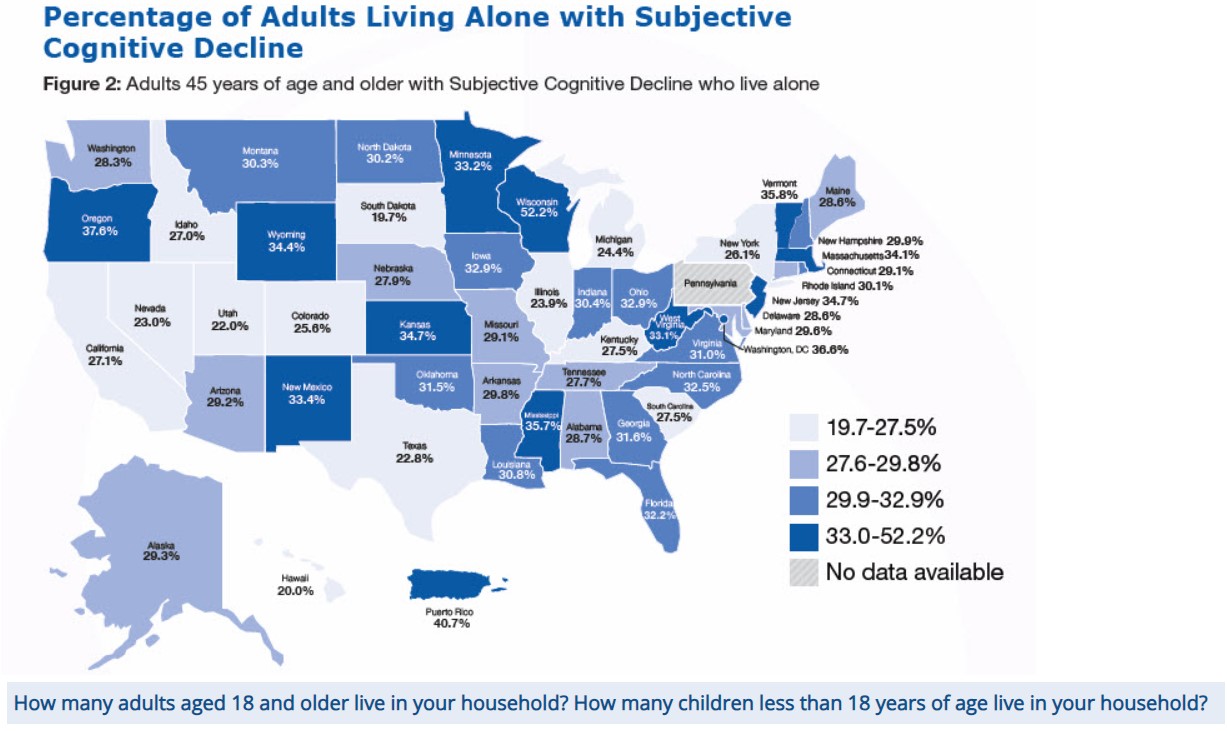
Older adults who live alone can be at risk for poor health outcomes, are less likely to use health services, and are more vulnerable to self-neglect and fall-related injuries than those living with others.6,7 Older adults who live alone report more unmet needs such as managing money, medications, mobility, and some activities of daily living.6,7
- Of adults with SCD, 29.3% live alone.
- Among persons reporting SCD aged 45-64 years, 24.7% live alone compared to 36.2% of those aged 65 years and older.
- 30.3% of women with SCD live alone compared to 28.1% of men.
- The prevalence of living alone among adults with SCD differs among racial/ethnic groups. Of those with SCD, 30.4% of Whites live alone compared to 35.5% of Blacks/African Americans, 18.3% of Hispanics, and 15.3% of Asians and Pacific Islanders.
Researchers have found that few adults with SCD discussed their confusion or memory loss with a health care professional.7-9 In fact, the prevalence of cognitive decline identified in community surveys is over twice that reported in medical records of general practitioners.8,9 Opportunities for improvement exist for increased screening, diagnosis, and identification of treatable cause(s).9
- Less than half of adults with SCD (45.3% of adults aged 45 years and older) reported discussing symptoms of confusion or memory loss with a health care professional.
- Among persons reporting SCD, 48.8% of those aged 45 to 64 years reported discussing their memory loss or confusion with a health care professional compared to 39.8% of persons aged 65 years and older.
- Half (50.5%) of women reported discussing SCD with a health care professional compared to 39.2% of men.
- The percentage of those who discussed SCD with a health care professional varies by race and ethnicity. Among Whites, 46.0% reported discussing SCD with a health care professional compared to 45.3% of Blacks/African Americans, 40.2% of Hispanics and 34.1% of Asians and Pacific Islanders.
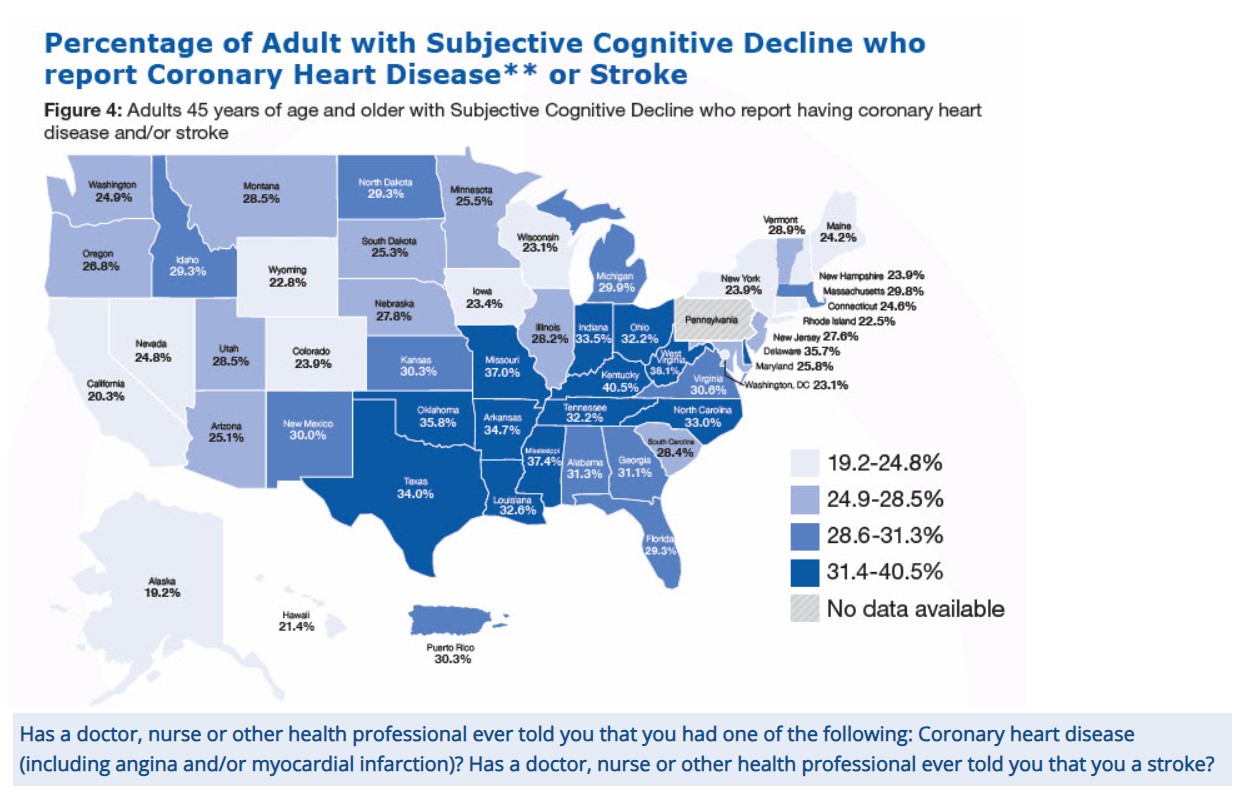
Coronary heart disease can lead to decreased cognitive function that can impact effective chronic disease self-management.10-13 Cognitive impairment in areas of learning, memory, and decision-making can increase the need for assistance in self-management, such as help with medication management or scheduling medical appointments.10-13
- More than 1 in 4 (28.6%) adults with SCD reported having coronary heart disease or stroke.
- Among adults with SCD, 23.9% of adults aged 45-64 years report having coronary heart disease or stroke, compared to 35.9% of adults aged 65 years and older.
- One in four (26.3%) women with SCD reported having coronary heart disease or stroke, compared to nearly one-third (31.3%) of men.
- The prevalence of CHD among adults with SCD is 25.7% in adults who completed at least some post high school education or higher compared to 31.7% among adults with a high school degree and 31.0% among adults with less than a high school degree.
** Respondents were classified as having coronary heart disease if they reported experiencing a heart attack (i.e., myocardial infarction) or angina
Multiple chronic diseases (two or more) have been found to be associated with increased cognitive decline.12-14 As the number of chronic diseases increases, the management of these conditions becomes increasingly complex, which may lead to a greater need for assistance. The presence of chronic diseases includes the report of at least one of the following: heart attack, coronary heart disease, stroke, asthma, cancer, arthritis, or diabetes.
- More than two-thirds (66.2%) of adults with SCD and have two or more chronic diseases.
- More than two-thirds (69.1%) of adults 65 years of age and older have both SCD and two or more chronic diseases, compared to 64.3% of adults 45-64 years of age.
- With respect to sex, 70.7% of women report SCD and having 2 or more chronic diseases compared to 61.2% of men.
Subjective Cognitive Decline and Frequent Mental Distress
Mental distress includes stress, depression and problems with emotions.15 Frequent mental distress (FMD) is defined as experiencing mental distress or having mentally unhealthy days for at least 14 days in a 30 day period.15
About how many days during the past 30 days was your mental health not good? (14 or more days = frequent mental distress)
- One third (33.7%) of adults with SCD report FMD.
- One in five (20.9%) adults 65 years of age and older with SCD reported FMD compared to 42.0% of adults 45-64 years of age.
- 37.6% of women with SCD reported FMD compared to 29.4% of men.
Subjective Cognitive Decline—related Functional Difficulties
SCD can impact people’s lives in ways that extend beyond thinking and remembering. It may interfere with a person’s ability to engage in activities they typically perform, like chores, socializing, taking medications, or working outside the home. An SCD-related functional difficulty is defined as always, usually, or sometimes giving up day-to-day household activities or chores and/or experiencing interference in engaging in activities outside the home.16
During the past 12 months, as a result of confusion or memory loss, how often have you given up day-to-day household activities or chores you used to do, such as cooking, cleaning, taking medications, driving, or paying bills?
During the past 12 months, how often has confusion or memory loss interfered with your ability to work, volunteer, or engage in social activities outside the home.
- Half (50.6%) of adults with SCD experienced SCD-related functional difficulties.
- SCD-related functional difficulties were more common among middle-aged adults (45-64 years of age; 58.7%) than among older adults (age 65 and older; 38.0%).
- More than half (53.4%) of women aged 45 years and older reported SCD related functional difficulties compared to 47.3% of men.
Call to Action
Subjective Cognitive Decline (SCD) is a public health issue and public health has a role in alleviating its impact. Below are some of the actions that can be taken to improve the health and well-being of persons with SCD. For additional actions, refer to The Healthy Brain Initiative: State and Local Public Health Partnerships to Address Dementias, The 2018-2023 Road Map.17
- Educate the public and health care professionals about brain health and the burden of SCD.
- Increase awareness that dementia, such as Alzheimer’s disease, is not a normal part of aging.
- Raise awareness about the best available evidence on dementia (including detection) and dementia caregiving, including risk reduction.
- Use this report and other analyses to make informed decisions and policies and promote the role of public health in addressing SCD as a priority.
- Increase awareness about the importance of managing chronic diseases, including conditions associated with coronary heart disease or stroke, among people with SCD and at all stages of dementia.
- Encourage patients and health care professionals to discuss SCD during routine medical office visits.
Page last reviewed: July 30, 2019
Content source: Division of Population Health, National Center for Chronic Disease Prevention and Health Promotion