In this post I link to and excerpt from Ultrasound for Lower Extremity Deep Venous Thrombosis: Multidisciplinary Recommendations From the Society of Radiologists in Ultrasound Consensus Conference [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Circulation. 2018 Apr 3;137(14):1505-1515
Here are excerpts:
ABSTRACT:
Venous ultrasound is the standard imaging test for patients
suspected of having acute deep venous thrombosis (DVT). There is variability and disagreement among authoritative groups regarding the necessary components of the test.The panel recommends a comprehensive duplex ultrasound protocol from thigh to ankle with Doppler at selected sites rather than a limited or complete compression-only examination. This protocol is currently performed in many facilities and is achievable with standard ultrasound equipment and personnel. The use of these recommendations will increase the diagnosis of calf DVT and provide better data to explain the presenting symptoms.
The panel recommends a single point-of-care protocol that minimizes underdiagnoses of proximal DVT.
The panel recommends the term chronic postthrombotic change to describe the residual material that persists after the acute presentation of DVT to avoid potential overtreatment of prior thrombus.
Adoption of a single standardized comprehensive duplex ultrasound and a single point-of-care examination will enhance patient safety and clinicians’ confidence.
CONSENSUS CONFERENCE RECOMMENDATIONS
The recommendations of the consensus conference can
be summarized into 5 key areas: (1) patient selection,
(2) ultrasound protocols, (3) serial and follow-up considerations, (4) terminology for ultrasound reports, and
(5) diagnostic criteria.Patient Selection
Issue
Multiple guidelines recommend clinical prediction rules to estimate pretest probability of DVT before ultrasound
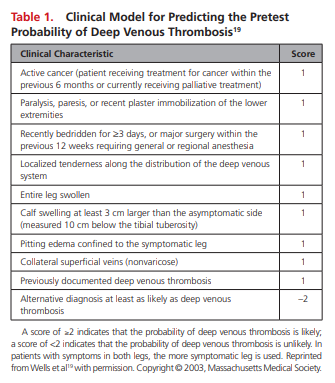
ordering.17–20 There are several tools, but the most commonly used clinical decision rule for risk stratification is the Wells score (Table 1).19
After an unlikely pretest probability of DVT based on a clinical decision rule assessment, a negative D-dimer test is adequate to safely exclude DVT. Venous ultrasound is not appropriate for those individuals.
Ultrasound is appropriate for patients with a likely pretest
probability of DVT, an unlikely pretest probability of DVT with a positive D-dimer, and those in whom pretest probability was not assessed.17,18Recommendation
All patients should be evaluated for pretest probability of DVT. For those with low (unlikely) pretest probability, obtaining a high-sensitivity D-dimer is appropriate.Ultrasound Protocols
We suggest that a single complete study is the safest
strategy. A limited examination to the knee requires a second examination to safely exclude undiagnosed calf DVT that may propagate proximally between the studies (Figure 1).
Recommendation
Complete duplex ultrasound (CDUS) is the preferred venous ultrasound test for the diagnosis of acute DVT.
CDUS is compression of the deep veins from the inguinal ligament to the ankle (including posterior tibial and peroneal veins in the calf), right and left common femoral vein spectral Doppler waveforms (to evaluate symmetry), popliteal spectral Doppler, and color Doppler images (Figure 2). Compression is performed at 2-cm intervals.3,21
Symptomatic areas should be evaluated to determine if there is superficial venous thrombosis or other pathology, in particular if the assessment of the deep veins is normal.
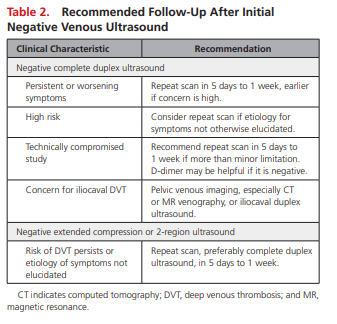
Limited protocols (not including calf veins) and selective evaluation of the calf are not recommended because limited protocols require a second study in 5 to 7 days to safely exclude DVT (Table 2).
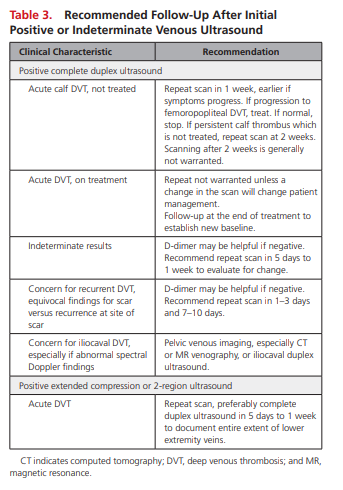
Patients with calf DVT who the clinician decides to manage expectantly should have a repeat scan at 1 week or sooner if risk factors or symptoms warrant. Repeat scans are ended after 2 weeks or if treatment is begun (Table 3).
Availability of Duplex Ultrasound and Point-of Care Ultrasound
Issue
Duplex ultrasound equipment and staff are not available in all sites at all times.
Recommendation
A point-of-care ultrasound consisting of a limited
evaluation with compression from thigh to knee
(extended compression ultrasound [ECUS]) (Figure 2 above) is appropriate when CDUS is not available in a timely manner.ECUS is favored over 2-region compression because isolated femoral vein DVTs may be missed. After a negative ECUS, CDUS in 5 to 7 days is required to safely exclude DVT.
If ultrasound is not available, anticoagulation before a confirmatory ultrasound is a safe strategy.22,23
Iliocaval DVT
Issue
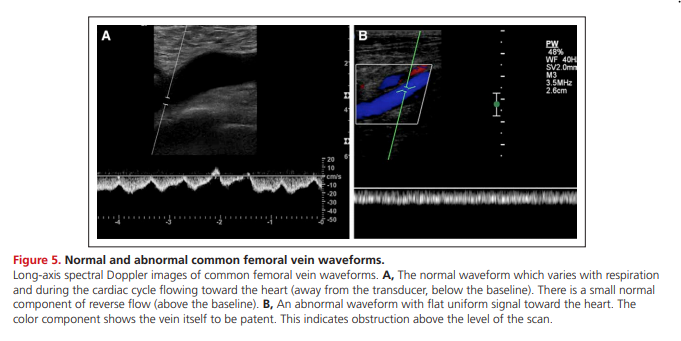
Iliocaval DVT may be undetected because the thrombus is cephalad to the standard examination. Whole-leg swelling with a normal compression ultrasound or the finding of continuous or asymmetrical common femoral Doppler spectra suggests a more central obstructive process.
Spectral Doppler abnormalities can be used to identify obstruction in the vein segments central to the sample site. Spectral Doppler assessment of both common
femoral or external iliac veins for phasicity and symmetry
may yield important information (Figure 5).
An abnormal spectrum, particularly a flat (continuous) waveform, has good specificity for iliocaval venous obstruction that may be the result of central thrombosis, scarring, or extrinsic compression from pelvic pathology.41,42
Recommendation
If iliocaval disease is suspected because of signs and symptoms or abnormal spectral Doppler waveforms, the threshold for pelvic ultrasound, computed tomography, or magnetic resonance venography should be low.
Serial and Follow-Up Considerations
Patients at High Risk, Those With Persistent Symptoms or Limited Studies
Issue
Occasional patients will have DVT despite a normal CDUS examination because of technical limitations, equivocal findings, or the lower sensitivity of the calf examination in comparison with examination of the femoropopliteal veins (Tables 2 and 3 above).
Recommendation
Repeat ultrasound may be required for patients who have a negative CDUS with persistent or worsening signs and symptoms, a technically inadequate CDUS, or an equivocal finding.
Follow-up is usually 5 to 7 days but can be shorter if concern is
high or clinical symptoms warrant.Patients with normal examinations to the knee or 2-region ultrasound require a serial ultrasound in 5 to 7 days.
Recurrent DVT
Issue
The diagnosis of recurrent DVT is difficult in the absence of an unequivocally new site of acute DVT (Figure 3). Persistent scarring may reduce the ability to distinguish chronic scarring from a new DVT.
Recommendation
Equivocal ultrasound findings may require serial imaging after 1 to 3 and 7 to 10 days to determine if there are any acute changes that would indicate recurrent DVT. D-dimer may also be helpful to establish if recurrent DVT is present.
Follow-Up of Patients on Anticoagulation
Issues
Repeat studies while the patient is on anticoagulation
are not standardized. There is no standard for ordering
an ultrasound at the end of anticoagulation.Recommendation
Imaging while on adequate anticoagulation is
unwarranted unless it will change the patient’s
treatment.Repeat ultrasound at or near the end of anticoagulation is recommended to establish a new
baseline and to determine if scarring is present.Complete Ultrasound Protocols
A single complete compression ultrasound is a safe strategy. A meta-analysis reported the 3-month risk of venous thromboembolic disease after negative complete compression ultrasound to be 0.57% (95% confidence interval, 0.25%–0.89%).11
The panel agreed that establishing a diagnosis of calf DVT is warranted even if anticoagulation is not instituted. Decisions regarding treatment of isolated calf DVT and risk stratification should be informed by as complete a diagnostic assessment as possible.
The presence of calf DVT may give information relevant to the patient’s ultimate outcome such as risks for recurrent DVT, mortality, subsequent diagnosis of cancer, and chronic venous insufficiency.15,32
The primary argument against implementation of
CDUS relates to the management of isolated calf DVT and concerns of overtreatment.33 False-positive diagnosis of calf DVT by ultrasound is rare; the specificity of compression ultrasound for calf DVT is 97.8% (97.0%–98.4%).34If isolated calf DVT is diagnosed and managed expectantly, there are well-defined protocols for followup.17
Patients with calf DVT that was observed without
anticoagulation should have a repeat scan, at 1 week
and again at 2 weeks if the calf DVT persists but does
not extend.17If there is proximal propagation or significant extension of the thrombosis, the patient should receive anticoagulation.
No further imaging is warranted if the distal DVT resolves at 1 week or does not extend significantly at 2 weeks.
Serial ultrasound is not indicated if the patient receives anticoagulation unless a change in the clinical condition warrants consideration of a change in treatment.39
Because the decision to withhold anticoagulation in a patient with diagnosed isolated calf DVT mandates additional scans, limited ultrasound protocols also require repeat imaging to be a safe strategy.
A negative CDUS does not completely exclude all DVT, in particular calf DVT.
The sensitivity of compression ultrasound for calf DVT is 56.8% (95% confidence interval, 49%–66.4%), less than that of duplex ultrasound for proximal DVT 96.5% (95% confidence interval, 95.1%– 97.6%).34
Propagation of calf DVT usually causes persistent or worsening symptoms. Appropriate patient followup and serial scans can address this complication.
Muscular (gastrocnemius or soleus) vein DVT may present as pain. Scans of symptomatic regions are part of CDUS protocol and can diagnose these DVTs.
Spectral Doppler abnormalities can be used to identify obstruction in the vein segments central to the sample site. Spectral Doppler assessment of both common femoral or external iliac veins for phasicity and symmetry may yield important information (Figure 5).
An abnormal spectrum, particularly a flat (continuous) waveform, has good specificity for iliocaval venous obstruction that may be the result of central thrombosis, scarring, or extrinsic compression from pelvic pathology.41,42
Point-of-Care Ultrasound Protocols
Complete protocols require a duplex Doppler ultrasound machine and are generally performed by a sonographer or vascular technologist.
There are circumstances (eg, emergency departments, rural areas, off hours) when a complete study cannot be performed in a clinically relevant time frame. In this situation, if point-of-care ultrasound can be performed by a competent practitioner, it should be performed.46,47
Extended compression ultrasound is a point-of-care protocol that has compression ultrasound from the inguinal ligament through the popliteal vein to the calf veins confluence.48
The most appropriate point-of-care examination for diagnosis of DVT is ECUS.
A negative ECUS or 2-region test requires a follow-up CDUS in 5 days to 1 week because the calf is not evalvuated.46,50 A CDUS should be performed after a positive limited ultrasound so that the entire venous system is mapped, including Doppler and calf evaluation.
Follow-Up Ultrasound
Most patients do not need additional ultrasound after a negative CDUS study in qualified laboratories. There are exceptions. If symptoms of DVT persist or worsen, a follow-up ultrasound at 5 days to 1 week or earlier is recommended.53
Isolated iliac vein thrombosis occurs in 1.6% of those with DVT.12 Imaging of the iliac and pelvic veins is warranted in patients whose signs and symptoms suggest iliocaval disease (eg, patients with whole-leg swelling with normal compression ultrasound). This may be accomplished by pelvic venous ultrasound, computed tomography, or magnetic resonance. Because the accuracy of duplex ultrasound for iliocaval DVT is not established, the threshold for computed tomography or
magnetic resonance venography should be low.55Follow-Up on Treatment
Patients on adequate treatment do not benefit from serial ultrasound during the course of treatment unless the findings of a repeat examination would affect management.39 Modest progression in the extent of thrombus can occur despite adequate anticoagulation. These changes, per se, do not indicate the need for an inferior vena cava filter or a change in anticoagulant.24,63,6
Ultrasound at the end of treatment is recommended to establish a baseline for future assessments.14,57,59,61,65 The reliability of CDUS to diagnose or exclude recurrent DVT is improved by having a posttreatment baseline ultrasound to determine which veins are normal and which are scarred.61,65
UNADDRESSED ISSUES
The prevalence of isolated calf vein thrombosis is variable, and more research is needed to determine its frequency and the risk and risk factors for propagation of untreated calf thrombus.67