Please see Resources after the end of this post for more great articles on prevention of cardiovascular disease.
This post contains links to and excerpts from Use of Risk Assessment Tools to Guide Decision-Making in the Primary Prevention of Atherosclerotic Cardiovascular Disease: A Special Report From the American Heart Association and American College of Cardiology [PubMed Abstract] [Full Text HTML] [Full Text PDF]. J Am Coll Cardiol. 2019 Jun 25;73(24):3153-3167. doi: 10.1016/j.jacc.2018.11.005. Epub 2018 Nov 10.
The above article is outstanding and merits close and repeated review by every clinician.
Here are excerpts:
Risk assessment is a critical step in the current approach to
primary prevention of atherosclerotic cardiovascular disease. Knowledge of the 10-year risk for atherosclerotic cardiovascular disease identifies patients in higher-risk groups who are likely to have greater net benefit and lower number needed to treat for both statins and antihypertensive therapy. Current US prevention guidelines for blood pressure and cholesterol management recommend use of the pooled cohort equations to start a process of shared decision-making between clinicians and patients in primary prevention. The pooled cohort equations have been widely validated and are broadly useful for the general US clinical population. But, they may systematically underestimate risk in patients from certain racial/ethnic groups, those with lower socioeconomic status or with chronic inflammatory diseases, and overestimate risk in patients with higher socioeconomic status or who have been closely engaged
with preventive healthcare services. If uncertainty remains for patients at borderline or intermediate risk, or if the patient is undecided after a patient–clinician discussion with consideration of risk enhancing factors (eg, family history), additional testing with measurement of coronary artery calcium can be useful to reclassify risk estimates and improve
selection of patients for use or avoidance of statin therapy.This special report summarizes the rationale and evidence base for quantitative risk assessment, reviews strengths and limitations of existing risk scores, discusses approaches for refining individual risk estimates for patients, and provides practical advice regarding implementation of risk assessment
and decision-making strategies in clinical practice.Use of Quantitative Risk Estimation in Current Prevention Guidelines
The 2018 Cholesterol Clinical Practice Guidelines 10 recommend the use of quantitative 10-year risk assessment, based on measurement of traditional ASCVD risk factors and with use of a validated risk prediction tool, as the first step in considering treatment options for primary prevention.
Results of 10-year risk estimation should be communicated through a clinician-patient risk discussion to decide on the intensity of preventive measures, especially whether to initiate medical therapy.
In present guidelines, patients with estimated 10-year ASCVD risk of 5% to <7.5% are considered to be at “borderline” risk and may be considered for drug therapy with a statin under certain circumstances; those with “intermediate” 10-year risk (7.5% to <20%) should be considered for initiation of moderate- to high-intensity statin therapy; and those with “high” 10-year risk (≥20%) should be considered for initiation of high-intensity statin therapy.10
In the 2017 Hypertension Clinical Practice Guidelines,7 quantitative risk estimation is recommended to guide the intensity of initial therapy for patients with stage 1 hypertension (SBP 130-139 mm Hg or diastolic blood pressure [DBP] 80-89 mm Hg). Patients with stage 1 hypertension and a 10-year ASCVD risk estimate <10% should be managed initially with nonpharmacological therapy, whereas those with 10-year risk ≥10% are recommended for initial management with both nonpharmacological approaches and antihypertensive drug therapy.7
Here are the direct links to Risk Scores in the table below:
Special Populations
Quantitative risk assessment with current risk scores should not be performed for patients with clinical ASCVD that requires secondary prevention, or for those with confirmed familial hypercholesterolemia or baseline low-density lipoprotein–cholesterol of ≥190 mg/dL. These groups require intensive preventive efforts with lipid-lowering drug therapy (given their considerable risk for future ASCVD events). Similarly, most patients with established diabetes mellitus should be considered
for statin therapy and for antihypertensive drug therapy (if blood pressure is elevated) regardless of predicted 10-year risk. However, 10-year risk estimation may still be useful in patients with diabetes mellitus to inform thresholds for initiation of antihypertensive drug therapy and intensity of statin dosing.Long-Term or Lifetime Risk Assessment
Guidelines5,6,10 have also promulgated use of tools for long-term or lifetime risk assessment (available at: https://tools.acc.org/ascvd-risk-estimator-plus/#!/calculate/estimate/42 and https://professional.heart.org/professional/GuidelinesStatements/ASCVDRiskCalculator/UCM_457698_ASCVD-Risk-Calculator.jsp43) to provide further perspective on the long-term consequences of single elevated clinical risk factors and the aggregate burden of risk factor levels over a longer time horizon. Therefore, lifetime risk assessment appears to be particularly useful for describing and communicating ASCVD risk in younger individuals (<50 years of age) who may have high lifetime risk, but in whom 10-year risk may be low even when significant risk factors are present, because of their young age and the 10-year risk prediction window.50–54
For example, more than half of the US adult population has a 10-year risk estimate <10% and a lifetime risk estimate ≥39%.53 To date, lifetime risk estimates have generally been recommended to promote therapeutic lifestyle change in younger individuals5,10 rather than as a means for patient selection for drug therapy. However, indirect evidence of benefit for initiation of statin therapy in individuals with lower 10-year risk (mean <10%) and high lifetime risk (based on inclusion criteria requiring at least 1 additional CVD risk factor50,52) was seen in the HOPE–3 (Heart Outcomes Prevention Evaluation–3) trial. In this trial, 10 mg of rosuvastatin reduced CVD events compared with placebo (3.7% versus 4.8%; hazard ratio: 0.76; 95% confidence interval: 0.64–0.91) over a median of 5.6 years of follow-up.55
A trial of statin versus placebo among younger individuals with low short-term and high lifetime risk is ongoing56 and may inform the potential use of using lifetime risk assessment for selection of younger patients for lipid-lowering drug therapy. Simultaneous assessment of 10-year and lifetime risks is therefore reasonable for the purposes of the clinician-patient discussion with an individual patient.
REFINING RISK ASSESSMENT FOR INDIVIDUAL PATIENTS: THE CLINICIAN PATIENT DISCUSSION
When considering drug therapy for primary prevention of ASCVD, clinicians and patients should begin by calculating the 10-year and lifetime ASCVD risk estimates.
Data including the absolute 10-year and lifetime risk estimates, the relative and absolute risk reduction benefit to be expected from drug therapy, and even numbers needed to treat over 5 and 10 years to prevent 1 ASCVD event or death may be useful concepts to address and to put in context for individual patients. Several tools and documents exist that may assist clinicians and patients in this discussion, including:
ACC’s ASCVD Risk Estimator Plus tool, which can predict 10-year risk using the PCE and can project expected benefit from different therapy choices (eg, initiation of statin, aspirin, or antihypertensive therapy, or smoking cessation in primary prevention; https://www.acc.org/ASCVDApp);57
Mayo Clinic Shared Decision Making Cardio vascular Primary Prevention Choice tool (https://shareddecisions.mayoclinic.org/decision-aid-information/decision-aids-for-chronic-disease/cardiovascular-prevention/);58
A monograph by Martin et al.59 describing the conceptual framework and practical implementation of the clinician-patient discussion; or
Table 7 in the 2018 Cholesterol Clinical Practice Guidelines,10 which provides a framework and tips for the clinician-patient discussion.
The paragraph below is critically important in refining an individual’s risk assessment.
In using these tools, it is important to recognize that quantitative 10-year risk assessment provides estimates of risk based on group means from large-scale population studies. There is, of course, uncertainty around these estimated probabilities, creating a distribution of risk for patients with a given risk estimate. Where an individual patient falls within the distribution around the estimated 10-year risk depends in large part on other factors, not included in the PCE, that may be considered by the clinician and patient. For example, a 45-year-old patient with a strong family history of premature-onset ASCVD is likely to be at higher risk than a patient with the same age, sex, race and risk factor profile but without such a family history. Discussion of these concepts may assist in eliciting patient preferences and attitudes toward ASCVD risk and views on drug therapy for prevention.
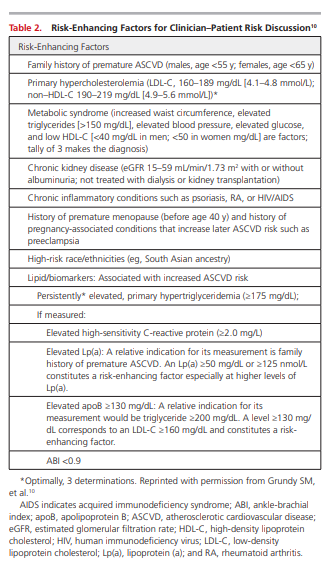
The 2018 Cholesterol Clinical Practice Guidelines 10 identify risk-enhancing factors, or comorbidities, that should be considered to affect the 10-year risk estimate for individual patients (Table 2).
However, it is difficult to determine how much a risk-enhancing factor or comorbidity may change the 10-year risk estimate quantitatively for an individual patient. Therefore, clinician judgment is crucial to determine whether the presence of a risk-enhancing factor is significant enough to reclassify an individual to a higher (or lower) risk category that may cross a treatment decision threshold for consideration of drug therapy.
If, after the clinician-patient discussion, the benefits of statin medication for the individual patient remain unclear, the patient has important risk-modifying factors that suggest a better or worse risk than the original estimate, or if the patient is undecided regarding drug therapy, additional testing to help with the decision in patients at borderline (5% to <7.5%) or intermediate 10-year risk (7.5% to <20% 10-year risk) is reasonable.
Some patients may also desire more specific personal information to guide their decision through demonstration of the presence or absence of the condition of interest (ie advanced atherosclerosis). Presently, the best additional test to help reclassify ASCVD risk in these situations is measurement of a CAC score for decision-making regarding statin therapy. Additional testing for decision-making for antihypertensive therapy may have lower clinical utility.60
CAC Measurement to Reclassify Risk
Recognizing the imprecision of multivariable CVD risk prediction scores—as well as the uncertainty clinicians and patients may encounter regarding the potential benefits of drug therapy for an individual patient at borderline or intermediate 10-year ASCVD risk—additional testing for assessment of the presence of subclinical atherosclerosis is reasonable. In such cases, additional testing should only be used if it can provide sufficient information to modify the decision. In general, identification of subclinical atherosclerosis rather than use of serum biomarkers is preferred, because of the extensive body of evidence demonstrating the superior utility of atherosclerosis disease assessment, particularly with CAC measurement, over any serum biomarker for the prediction of future ASCVD events, including both coronary heart disease and stroke.61–63 Other modalities for assessing subclinical atherosclerosis, including carotid intima-media thickness and carotid plaque burden assessment, are weaker predictors of overall ASCVD events compared with the CAC score.5,62,63
Reclassification of Risk Using CAC Scores
Since the publication of the “2013 ACC/AHA Guideline on the Assessment of Cardiovascular Risk” and
the “2013 ACC/AHA Guideline on the Treatment of
Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults,”5,6 a substantial amount of evidence has been published demonstrating the utility of CAC measurement to reclassify risk specifically in the context of the PCE.32,62,63,72–76 Data demonstrate the important improvements in discrimination, calibration, and net reclassification that can occur for intermediate-risk patients with measurement of CAC after quantitative risk assessment, as is frequently seen in
sequential Bayesian testing strategies using effective
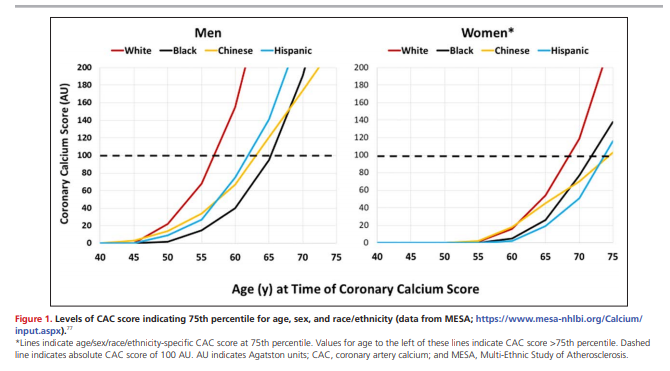
secondary tests with reasonable sensitivity and specificity for prognosisReclassification of borderline and intermediate-risk patients with demonstration of a CAC score of ≥100 Agatston units (AU) (or ≥75th percentile for age, sex, and race/ethnicity; see the MESA [Multi-Ethnic Study of Atherosclerosis] CAC tools website, https://www.mesa-nhlbi.org/Calcium/input.aspx)77 identifies patients who have a 10-year event rate ≥7.5%, who would be expected to have greater benefit from statin therapy (“up-risking”).32,62,63,72–76 Figure 1 shows the CAC score values indicating the 75th percentile for age/sex/race/ethnicity. Men <50 years of age and women <60 years of age with any CAC will nearly always exceed the 75th percentile. Similarly, men <60 years of age and women <70 years of age with CAC measurement of ≥100 AU will nearly always exceed the 75th percentile. Conversely, reclassification of intermediate-risk patients who have a CAC score of 0 AU identifies patients with low observed 10-year event rates that fall below the range where statins may provide net benefit (“derisking” or “downrisking”).32,62,63,72–76,78
For details on integrating CAC scoring with risk scores review:
- CAC Scoring in Intermediate-Risk Patients (Predicted 10-Year ASCVD Risk of 7.5% to <20%)
- CAC Scoring in Low-Risk and Borderline Risk Patients
- CAC Scoring in High-Risk Patients (≥20% 10-Year Risk)
PRACTICAL APPROACH TO RISK ASSESSMENT AND CLINICAL DECISION-MAKING
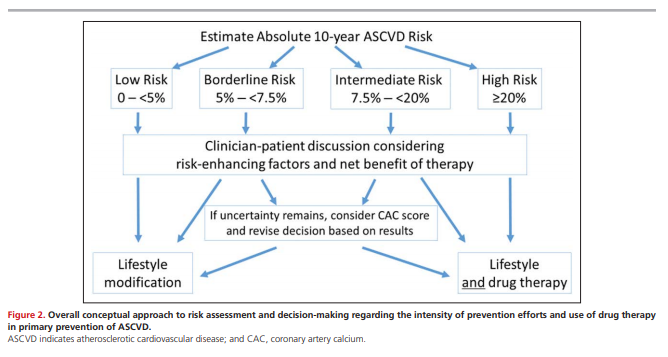
Figure 2 displays the conceptual approach to risk assessment and its role in decision-making regarding the intensity of prevention efforts and use of pharmacotherapy in primary prevention of ASCVD, particularly in the context of decision-making for use of statin medications.
Figure 2 below is the same as the one I included above:
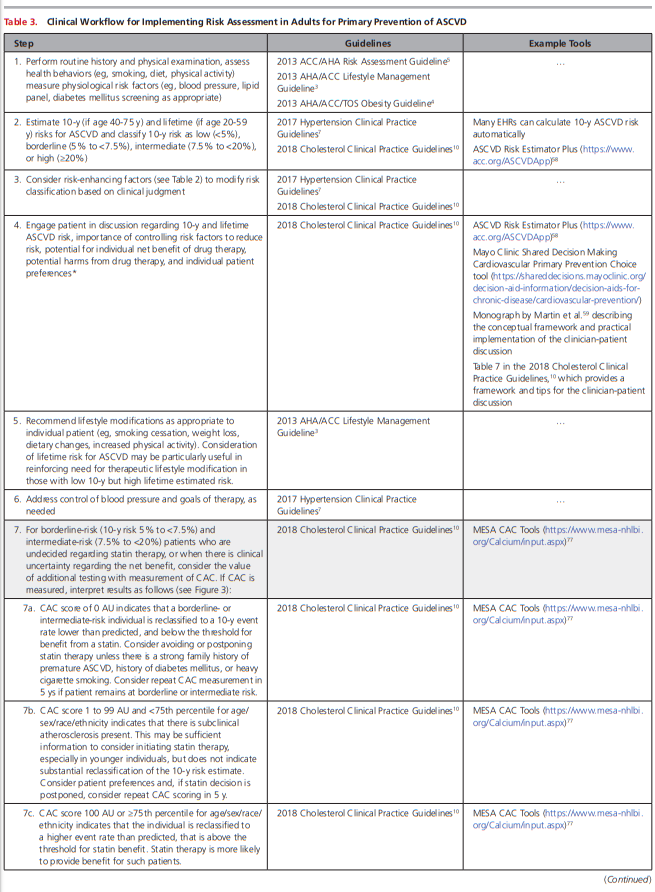
Table 3 provides a stepwise approach, in addition to clinical practice guidelines and tools to assist clinicians and patients through this process.
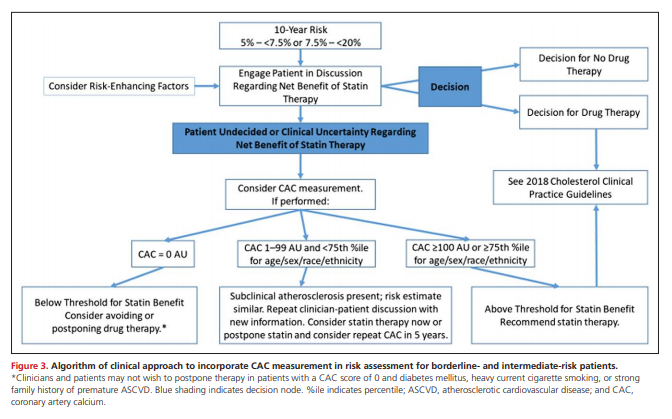
The interpretation and clinical response to a CAC score in borderline- or intermediate-risk patients merits further discussion. Table 3 provides guidance, and Figure 3 provides an algorithm of the clinical workflow to incorporate CAC measurement and interpretation.
Those with CAC score of 0 AU appear to have 10-year event rates below the range where statins provide net benefit, suggesting that drug therapy may be less beneficial at present.
Those with CAC score of ≥100 AU (or ≥75th percentile for age/sex/race/ethnicity) are reclassified to the extent that they have event rates in a range where statin therapy would be even more clearly beneficial.
Posttest risk estimates do not differ substantially from pretest estimates for those with CAC scores of 1 to 99 AU and <75th percentile for age/sex/race/ethnicity, so it is recommended to continue the risk discussion to make a decision regarding the use of drug therapy. Patient preference may be particualrly important to elicit in this scenario.
Figure 2 presents the CAC score thresholds at which
the CAC score meets the 75th percentile for age, sex,
and racial/ethnic subgroups (based on data from the
MESA study; https://www.mesa-nhlbi.org/Calcium/
input.aspx).
Resources:
(1) Use of Risk Assessment Tools to Guide Decision-Making in the Primary Prevention of Atherosclerotic Cardiovascular Disease: A Special Report From the American Heart Association and American College of Cardiology [PubMed Abstract] [Full Text HTML] [Full Text PDF]. J Am Coll Cardiol. 2019 Jun 25;73(24):3153-3167. doi: 10.1016/j.jacc.2018.11.005. Epub 2018 Nov 10.
(2) The ASCVD Risk Estimator Plus
What follows is from the above link:
For Optimal Use:
- Estimate patient’s 10-year ASCVD risk at an initial visit to establish a reference point.
- Forecast the potential impact of different interventions on patient risk.
- Reassess ASCVD risk at follow-up visits. Follow up risk incorporates change in risk factor levels over time and requires both initial and follow up values.
- Use the information above to help with clinician-patient discussions on risk and risk-lowering interventions. [This point refers to the three tabs at the very top of the app screen: Estimate Risk, Therapy Impact, and Advice Tab]
- See the “About the App” screen in this app for a definition of terms and additional instructions.
(3) 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Hypertension. 2018; 71:1269–32
(4) 2018 ESC/ESH Guidelines for the management of arterial hypertension [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Eur Heart J. 2018 Sep 1;39(33):3021-3104. doi: 10.1093/eurheartj/ehy339.
(5) 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/ AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines [PubMed Abstract] [Full Text HTML] [Full Text PDF]. J Am Coll Cardiol. 2019 Jun 25;73(24):3168-3209. doi: 10.1016/j.jacc.2018.11.002. Epub 2018 Nov 10.
(6) 2016 European Guidelines on cardiovascular disease prevention in clinical practice [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Atherosclerosis. 2016 Sep;252:207-274. doi: 10.1016/j.atherosclerosis.2016.05.037.