Note to myself: I originally posted this on December 18, 2018. I have reposted it today as it contains a nice summing up of the treatment of both allergic and non-allergic rhinitis and sinusitis.
The bottom line, it seems to me, after reviewing Resources (1) and (2) below, is to use the the same medications for nonallergic rhinitis that you would use for allergic rhinitis and see which ones best work for the individual patient.
Resource (3) has information on how to use general Quality Of Life Questionnaires such as the Medical Outcomes Survey Short Form 36 (SF-36) and the disease specific questionaires such as adult Rhinoconjunctivitis Quality of Life Questionnaire and the Paediatric Rhinoconjunctivitis Quality of Life Questionnaire.
The above quality of life questionnaires can be used to help patients characterize how they are doing with their rhinitis treatment plan [Better, worse, the same, or can’t really say (can’t really tell)].
Resource (4) below is a review of chronic sinusitis from emedicine.medscape.com as is Resource (5) on turbinate dysfunction. Both are worth reviewing for help with the patient with nonallergic rhinitis who has not improved on your therapy.
Here are excerpts from Resource (1) below:
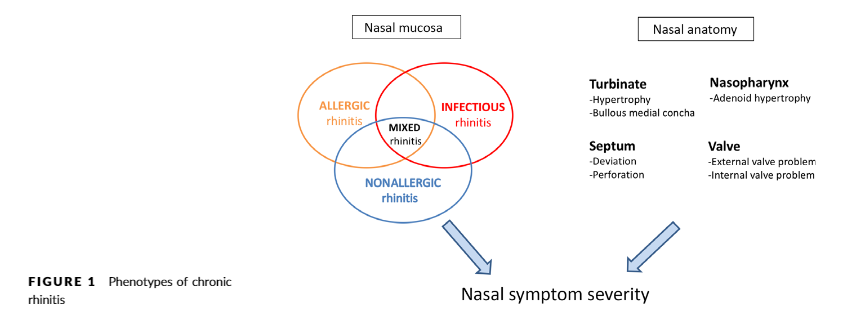
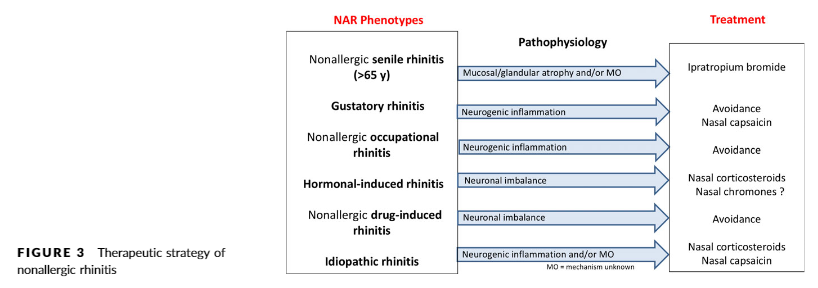
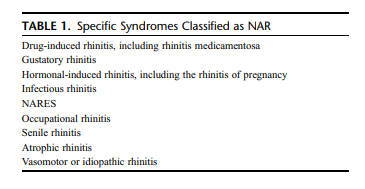
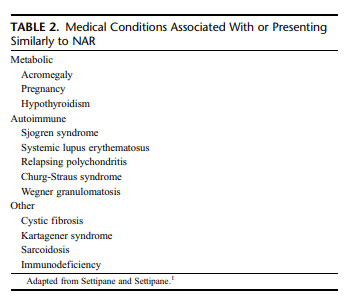
NAR patients constitute a group of patients with different pheno-types, with variable severity, underlying etiology and type of inflammation. The phenotypes warrant different treatment strategies depending on the etiology. However, most of the studies on treatment for NAR have been performed in unselected NAR patients. It makes sense to link the therapeutic strategy to the known or suspected underlaying etiology, being inflammation, neurogenic dysfunction, environmental exposure, and/or medication use (Figure 3).The inflammatory group (occupational rhinitis and drug-induced rhinitis) may benefit from anti-inflammatory treatment such as nasal/oral corticosteroids and/or nasal/oral antihistamines. However, mostRCTs evaluating local corticosteroids in NAR patients showed a lack of efficacy. Only two studies 57, 58 comprising 101 patients showed a positive outcome, whereas all other studies comprising more than 1000 patients did not show a major benefit of nasal corticosteroid treatment 59,60,61
Interestingly, two double-blind, placebo-controlledtrials have been published showing a therapeutic effect for azelastine nasal spray in NAR patients 62,63 The precise mode of action (antihistaminic, anti-inflammatory, or otherwise) remains to be elucidated.
Here are excerpts from Resource (2) below:
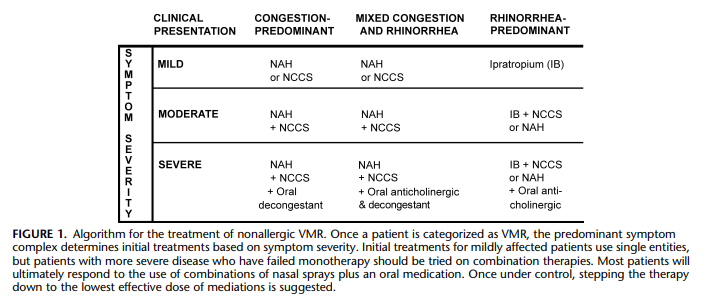
Nasal Corticosteroids
Nasal corticosteroids treat inflammatory conditions regardless of etiology. There is substantial evidence that corticosteroids benefit AR, some forms of NAR including VMR, and chronic rhinosinusitis.
In VMR, the scent of fluticasone is sometimes a negative
feature in patients for whom scent is a trigger. However, as a
class, NCCS treats the broadest spectrum of NAR symptoms
and seems to have at least some degree of efficacy in all NAR variants, including VMR. Thus, for the treatment of NAR,
NCCSs are considered a first-line therapy.Antihistamines
It is quite likely that all NAR patients have tried oral
antihistamines, either in the form of over-the-counter medications or as prescribed by physicians who assume that the
symptoms are caused by allergies. Histamine release has not
been seen in NAR and is specifically not seen in VMR other
than cold-airYinduced rhinitis.20 Thus, the use of oral antihistamines makes little sense, and these medications have rarely been studied in VMR.By contrast, intranasal antihistamines are very effective
in treating AR (both azelastine and olopatadine are approved
for treating SAR). Azelastine is also approved by the FDA for
treatment of nonallergic VMR. Although azelastine is primarily an antihistamine, it is unlikely that its efficacy in VMR
is due to histamine receptor blockade. Instead, it is probably
azelastine’s actions as an anti-inflammatory and neuroinflammatory blocker that makes this medication useful in treating VMR or NAR. Azelastine has been shown to deplete inflammatory neuropeptides in the nasal mucosa; to reduce levels of proinflammatory cytokines, leukotrienes, and cell adhesion molecules; and to inhibit mast cell degranulation.25 . . . . On the basis of both published clinical studies and extensive clinical experience, the use of azelastine (and possibly olopatadine) alone and in combination with NCCS is a preferred first-line treatment of VMR/NAR as well as AR.Anticholinergics
Ipratropium bromide (IB) is a potent intranasal anticholinergic with utility in the treatment of rhinorrhea in AR
and NAR. It has been studied in both adults and children.
Ipratropium bromide specifically treats rhinorrhea and does
little to improve congestion. Intranasal anticholinergics work
best for rhinorrhea predominant NAR variants such as coldairYinduced rhinitis (skier’s nose)29 and gustatory and senile rhinitis.30 In 28 patients with cold-airYinduced rhinitis, IB reduced the symptoms and the number of tissues required
during and after cold exposure (P = 0.0007 and 0.0023, respectively).31 In children with perennial AR or NAR, the effect
of IB was superior to placebo and equivocal to beclomethasone dipropionate (BD) for the treatment of both rhinorrhea
and congestion. However, IB was less effective than BD for
controlling sneezing.32Similar to the nasal antihistamines, there seems to be an
additive effect when IB is used in conjunction with NCCSs.33
In a study comparing beclomethasone versus IB versus the two
combined, the combination group had better symptom control
of rhinorrhea. Beclomethasone monotherapy was found to
better treat sneezing and congestion than IB monotherapy.
Both medications were very well tolerated.Conclusion
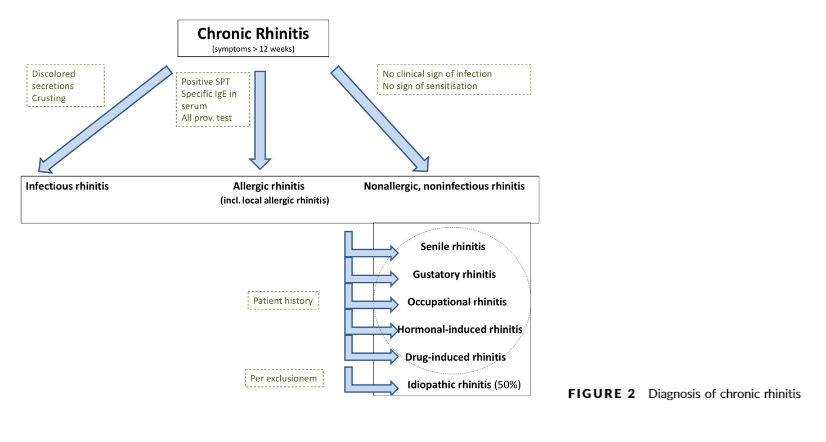
Nonallergic rhinitis is an underrecognized and inadequately treated condition affecting many subjects. Diagnosis
is dependent on a thorough history and exclusion of other
underlying conditions, including AR and chronic rhinosinusitis.
Nonallergic rhinitis tends to require chronic medical management, and use of topical NCCSs and nasal antihistamines, used alone or in combination, is very effective in most patients. This combination is also extremely effective in treating AR. Thus, recognizing that the combination of both NCCSs and nasal antihistamines effectively treat AR, VMR, and mixed rhinitis, this combination of medications seems to be a useful first-line treatment for the overwhelming majority of rhinitis patients.
Resources:
(1) Non-allergic rhinitis: Position paper of the European Academy of Allergy and Clinical Immunology [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Allergy. 2017 Nov;72(11):1657-1665. doi: 10.1111/all.13200. Epub 2017 Jun 2.
(2) Nonallergic rhinitis, with a focus on vasomotor rhinitis: clinical importance, differential diagnosis, and effective treatment recommendations [PubMed Abstract] [Full Text HTML] [Full Text PDF]. World Allergy Organ J. 2009 Mar;2(3):20-5. doi: 10.1097/WOX.0b013e3181990aac.
(3) Rhinitis Quality of Life in Clinical Practice [Full Text PDF]
ELIZABETH F. JUNIPER MCSP, MSC.
DEPARTMENT OF CLINICAL EPIDEMIOLOGY AND BIOSTATISTICS,
MCMASTER UNIVERSITY, HAMILTON, ONTARIO CANADA
(4) Chronic Sinusitis Updated: Jul 27, 2018 Author: Itzhak Brook, MD, MSc from emedicine.medscape.com
(5) Turbinate Dysfunction Updated: Jul 11, 2018 Author: Sanford M Archer, MD from emedicine.medscape.com
(6) Montelukast in the management of allergic rhinitis [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Ther Clin Risk Manag. 2007 Jun;3(2):327-32.